Hip Dysplasia
Ryan Cordry and Richard Santore
Key Points
Introduction
The most common underlying cause of secondary osteoarthritis of the hip is congenital hip disease.1–4 The spectrum of deformities can be quite large. This range represents a continuum from subtle acetabular dysplasia to progressively increasing degrees of subluxation, culminating with complete dislocation. When this process is recognized early, and before significant secondary arthritis, joint preservation surgeries may be possible to delay or prevent the need for hip replacement. In general, joint-preserving surgery is not appropriate once Tonnis II changes are present. However, even Tonnis I arthritis is sometimes best managed nonoperatively until natural progression dictates total hip arthroplasty (THA). When significant articular destruction has resulted in arthritis, THA is the most reliable and appropriate procedure to relieve pain and restore function.
Total hip arthroplasty can be performed in the presence of mild dysplasia, much as in primary osteoarthritis. However, even in mild dysplasia, it is important to anticipate the possible need for special surgical considerations and techniques. Reconstructing the arthritic hip in the setting of severe dysplasia can be one of the most challenging circumstances facing hip surgeons. This chapter covers the indications, surgical approaches, component selection, complications, and techniques used to prepare the hip surgeon for the challenges associated with reconstructing the dysplastic hip.
Classification
Several classification systems have been developed to characterize dysplastic hips in the adult population. The two most frequently used systems are those of Crowe5 and Hartofilakidis.6,7 Both of these systems are relatively easy to use and require only a plain anteroposterior (AP) radiograph of the pelvis. These systems are useful for guiding treatment and providing prognostic information. The system devised by Mendes8 is more complex and is focused on surgical planning.
The Crowe system5 is based on the ratio of the distance the upper femur has migrated proximally relative to the femoral head diameter. A reference line that connects the teardrops of both hips is drawn. Despite the presence of dysplasia, the inferomedial femoral head-neck junction is generally readily recognizable. A point is marked at this position, and the distance from the reference line is carefully measured. The height of the pelvis and the superior-to-inferior diameter of the femoral head should be measured; in practice, however, only one of these two measurements is required. Occasionally, obtaining an accurate measurement of the diameter of the femoral head may be difficult owing to severe bilateral deformity or suboptimal radiographic technique. Because the femoral head diameter is typically 20% of the height of the pelvis, pelvic height may be substituted in calculating the ratio of migration. In normal hips, the inferomedial head-neck junction will sit within a few millimeters of the reference line drawn to connect the teardrops. In class I dysplasia, this point will sit cephalad to the reference line at a distance that is less than 50% of the diameter of the femoral head (<10% of the height of the pelvis). Class II dysplasia is present when this point has migrated 50% to 75% of the diameter of the femoral head (or 10% to 15% of the height of the pelvis). Class III dysplasia is identified with a migration distance of 75% to 100% of the femoral head diameter (or 15% to 20% of the pelvic height). When the proximal femur has migrated more than 100% of the diameter of the femoral head (or 20% of the height of the pelvis), the dysplasia is defined as class IV (Fig. 75-1).
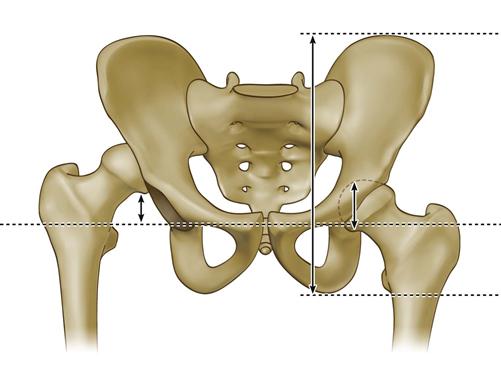
Figure 75-1 Measurements used in the Crowe grading system. (Redrawn from Sanchez-Sotelo J, Berry DJ, Trousdale RT, Cabanela ME: Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options. J Am Acad Orthop Surg 10:334–344, 2002.)
The classification system proposed by Hartofilakidis segregates adult dysplastic hips into one of three categories: dysplastic, low dislocation, or high dislocation.6,7 Dysplastic hips may be subluxated; however, the femoral head is still contained within the true acetabulum. When the femoral head articulates with a false acetabulum, which overlaps the true acetabulum, a low dislocation is identified. This is noted when the inferior lip of the false acetabulum overlaps the superolateral lip of the true acetabulum. When no overlap is encountered and the femoral head is articulating with a false acetabulum located proximal and posterior to the true acetabulum, a high dislocation is identified. This classification system is intuitive and easy to use (Figs. 75-2 through 75-4).

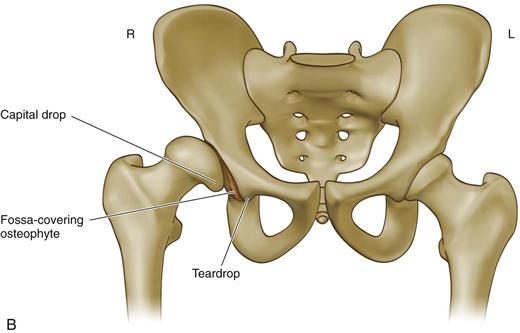
Figure 75-2 The Hartofilakidis dysplastic hip. Radiograph (A) and line drawing (B) of a 28-year-old woman who had a dysplastic hip on the right. (From Hartofilakidis G, Stamos K, Karachalios T, et al: Congenital hip disease in adults: classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am 78:683–692, 1996. Part B redrawn.)
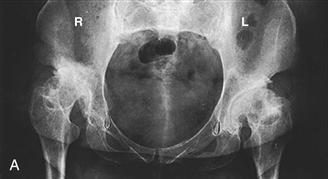
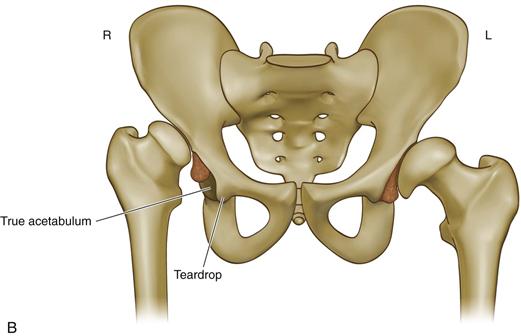
Figure 75-3 The Hartofilakidis low dislocation (right hip) and dysplastic (left hip) hip. A, A 44-year-old woman who had bilateral congenital hip disease. B, Line drawing of the same hips showing the differences between a low dislocation and a dysplastic hip with approximately the same degree of subluxation. (From Hartofilakidis G, Stamos K, Karachalios T, et al: Congenital hip disease in adults: classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am 78:683–692, 1996. Part B redrawn.)
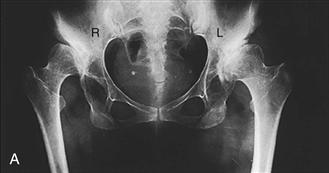
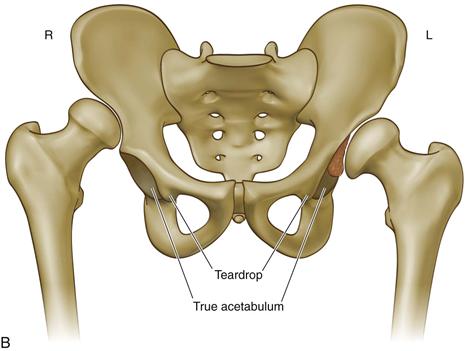
Figure 75-4 The Hartofilakidis high dislocation. Radiograph (A) and line drawing (B) of a 42-year-old woman who had a high dislocation of the hip on the right and a low dislocation on the left. (From Hartofilakidis G, Stamos K, Karachalios T, et al: Congenital hip disease in adults: classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am 78:683–692, 1996. Part B redrawn.)
Mendes8 proposed a classification system that is more focused on surgical planning of the hip arthroplasty and involves concepts beyond radiographic features alone. Its clinical application has not been validated for reproducibility/reliability or for its prognostic information. Nevertheless, it is a useful tool when preparing and templating the reconstructive procedure. There are two general categories of dysplastic hips according to this system: subluxated and high. For each type of hip, priorities are established to guide the procedure. Primary consideration is given to bone stock and acetabular inclination. Bone stock may be considered adequate or deficient. Acetabular inclination is characterized as normal or superior. Characterizing soft tissue abnormalities, based on the presence of weakness or contracture, constitutes the secondary consideration. Tertiary considerations evaluate such factors as leg length inequality, pelvic obliquity, knee valgus, or lumbar curvature. Clearly, taking into consideration all of the unique clinical aspects of dysplasia makes intuitive sense.
A recent study9 showed excellent intraobserver and interobserver reproducibility and reliability for the Crowe and Hartofilakidis classification systems. This confirms the utility of these systems in comparing results among treating surgeons and centers. The manner in which these systems guide treatment for the surgeon is discussed throughout the chapter. Several other studies have reported the prognostic implication of these two classification schemes10–12; one found an increased rate of revision and loosening of the acetabular component in Crowe IV hips compared with Crowe I through III.12 Cameron and associates10 showed that Crowe I hips undergoing THA had equal Harris Hip scores and limp after THA as patients undergoing THA for nondysplastic osteoarthritis. Patients after THA for Crowe II through IV showed progressively lower Harris Hip scores. High complication rates were noted in Crowe III (25%) and IV hips (50%), with no increase in rate of complications in the Crowe I or II group.
Anatomy
Understanding the pathologic anatomy of the dysplastic hip is important when considering its reconstruction. Anatomic changes are present on both the acetabular and femoral sides of the joint and are proportional to the severity of dysplasia.5,13,14 Both bony and soft tissue alterations are common. Computed tomography (CT) scans, although not essential for the diagnosis or treatment of dysplasia, afford a more detailed appreciation of the bony changes present in these hips. These morphologic differences from typical hips form the basis of the potential pitfalls of this operation.
Dysplastic hips are smaller and architecturally abnormal as compared with normal adult hips. The femoral head is small and can become flattened.15 The femoral neck is generally shorter and the upper femur more anteverted compared with age-matched controls.14 Even mildly dysplastic joints have increased femoral anteversion compared with normal adult controls.14,16,17 This anteversion is a rotational deformity localized to the proximal femoral diaphysis rather than the neck itself and is not related to coxa valga.14,16,17 The proximal femoral canal is straighter and narrower, particularly in the coronal plane.5,13-16 The greater trochanter is found more posteriorly5,13 and is soft and underdeveloped.15 Proximal femoral bone is also smaller and weaker than in nondysplastic hips and is more prone to intraoperative fracture.
Structural changes to the acetabulum of adults with congenital hip disease are also common. Volumetric insufficiency describes the appearance of the dysplastic acetabulum with or without dislocation. Dunn and Hess15 described the pathologic anatomy associated with 22 congenitally dislocated hips of 16 patients undergoing THA. The acetabula in their series appeared small, shallow, and poorly developed. In cases of late dislocation after years of subluxation, investigators noted erosion of the superior aspect of the acetabulum. This significantly worsened already shallow sockets and complicated attainment of coverage of the acetabular component. They reported extremely soft bone directly superior to the true acetabulum due to chronic lack of weight bearing in this area.
Hartofilakidis and colleagues7 analyzed 431 hips and described their morphology based on the severity of dysplasia. They classified these hips as dysplasia, low dislocation, or high dislocation. Of these, all 325 dysplastic hips had a deficiency of the superior segment of the acetabulum. In each of the low dislocations, a deficiency of the anterior and posterior segments was evident, and all high dislocations had a deficiency of the entire rim. All low and high dislocations had a narrow opening of the acetabulum and inadequate depth. Posterosuperior bone stock was decreased in 32 of 43 (74%) low dislocations and in 56 of 63 (89%) high dislocations.
Soft tissues are also abnormal. Neurovascular structures are shortened and are no more likely to stretch than in normal hips. Hamstring, quadriceps, and adductor muscles are shortened. As the femoral head migrates proximally, the abductors shorten and insert on the proximal femur from a more horizontal direction. This variance in the orientation of muscles needs to be anticipated during the surgical approach to the hip to avoid unintended damage to the abductors. Harris and coworkers18 in a report of their early experience with 22 patients in the setting of developmental dysplasia of the hip (DDH) described the anatomic alterations present in 27 hips. They noted proximal displacement of the femoral nerve and profunda femoris artery. The femoral nerve was vulnerable to injury as the proximal femur was retracted anteriorly for exposure of the acetabulum. Additionally, the profunda femoris artery passed closer to the inferior pole of the acetabulum, which may predispose it to injury. They also found an elongated hip capsule, which had a proximal rather than distal orientation. The hip capsule was frequently thickened and was described as having an hourglass shape. Dunn and Hess15 found the superior portion of the capsule to firmly adhere to the abductors, while the inferior portion frequently obscured the true acetabulum.
Preoperative Evaluation
The importance of a detailed history and physical examination cannot be overemphasized. It is important to understand what limitations patients are experiencing, as well as their desired level of activity. Patients with Crowe grade II or III disease frequently present at younger ages than those with grade I or IV. These younger patients may have expectations of resuming high levels of activity.
Many patients with DDH will present before advanced osteoarthritic changes are present. Prearthritic patients with definite structural abnormalities about the hip may be candidates for acetabular and/or femoral osteotomy. These joint-preserving procedures may delay the need for arthroplasty and may diminish some of the challenges for the arthroplasty surgeon. However, these procedures are not the subject of this chapter.
As in typical primary osteoarthritis of the hip, patients may experience groin or buttock pain as a direct result of their diseased hip. Ipsilateral knee pain is commonly reported in patients with dysplastic hips. Leg length discrepancy, muscle weakness, and pelvic obliquity may cause a limp and secondary lumbosacral symptoms and problems. Pelvic obliquity and leg length differences can be clinically assessed by placing blocks under the short leg until the pelvis is leveled, by measuring the distance from the umbilicus and the anterosuperior iliac spine (ASIS) to the tip of the medial malleolus, or by performing a scanogram. These assessments should assist the surgeon in determining how much lengthening is desired during the reconstructive procedure.
Stiffness about the hip joint should be assessed so the clinician can further understand any soft tissue releases that may be required. Hip flexion contracture functionally shortens the lower extremity, thereby adversely affecting the patient’s gait. The contracture is most readily observed in the supine position and during gait. The supine patient should be able to place the affected thigh flat on the examination table without accentuating lumbar lordosis. Full extension of the knee should be confirmed to ensure that the restricted motion is isolated to the hip. Observation of a patient during gait is likely to reveal an obvious limp with a short stride, toe-walking, and increased lumbar lordosis during the stance phase. Treatment of the flexion contracture with anterior capsule and/or iliopsoas tendon release will improve hip extension, alleviate compensatory hyperlordosis of the lumbar spine, reduce functional leg length inequality, and facilitate true lengthening of the lower extremity. The need for this adjunctive soft tissue surgery is determined on a case-by-case basis; the procedure is more frequently appropriate in DDH associated with neuromuscular conditions.
The patient should be closely observed while walking to assess the gait pattern. Leg length discrepancy, pain, and muscle weakness are the three contributing factors to the limp in DDH patients. Any real leg length inequality can be normalized with a lift placed on or in the shoe of the short extremity. If the limp persists in spite of the lift, other causes should be considered. Pain causing an antalgic gait may be assessed by injecting a local anesthetic into the hip joint. Documentation of the Trendelenburg sign as well as the patient’s abductor strength against gravity and manual resistance in the side-lying position is helpful in describing the degree of weakness present. Poor abductor function may result from proximal femoral migration or reduced femoral offset. Optimizing abductor function is a critical component of the successful hip reconstruction.
Radiographic evaluation should include a standard anteroposterior (AP) view of the pelvis, including both hips, an AP of the involved hip, and a true lateral of the proximal femur. A false profile view of the involved hip provides additional valuable information regarding the acetabulum. It allows for assessment of anterior and posterior bone stock, as well as acetabular version. As was previously noted, full-length standing orthoroentgenograms of bilateral lower extremities may be used to further quantify leg length inequality when necessary. More detailed images, such as CT scans that include three-dimensional reconstructions, may be used for situations in which plain radiographs fail to provide clarity, in cases of high-grade deformity, or when custom implants will be used. Magnetic resonance imaging (MRI) is seldom useful in the presence of established osteoarthritic changes about a dysplastic hip, although its utility when joint preservation is considered is significant. Imaging results should be correlated with history and physical examination findings.
Indications
Hip pain due to osteoarthritis, which limits activities of daily living, is the most common indication for arthroplasty. Most patients presenting with secondary osteoarthritis caused by developmental dysplasia of the hip will describe pain in the involved groin, hip, or buttock. Other reports may include limp, weakness, leg length inequality, or ipsilateral knee pain due to ambulating with the dislocated hip. Leg length inequality causing pelvic obliquity and compensatory lumbar lordosis may provoke low back pain.
Patients with grade II or III dysplasia according to Crowe5 tend to develop osteoarthritis earlier in life. Counter to intuition, some patients with bilateral grade IV disease may function relatively well despite significant radiographic abnormalities. These patients ambulate with a “waddling” gait bilaterally, with similar leg lengths and relatively limited pain. They frequently respond favorably to oral analgesic medication and a brief period of activity modification. A short course of ambulating with an assistive device such as a crutch or a cane is frequently a powerful tool that may postpone the need for arthroplasty. A course of physical therapy for muscle strengthening exercises may provide relief of symptoms. Delaying surgical intervention in these patients until symptoms worsen is prudent. This subset of patients carries the greatest risk of surgical complications and reduced survivorship. When symptoms are well tolerated, life-long nonoperative management is not inappropriate for these patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








