I. Introduction—Hip dislocations and fracture-dislocations occur across all age groups and represent a spectrum of injuries that can result when abnormal load is placed on the hip. The position of the femur when the force is applied determines the pattern of injury. The force can be dissipated by any combination of femur fracture, intertrochanteric fracture, femoral neck fracture, hip dislocation, acetabular fracture, femoral head fracture, and pelvic fracture. Hip dislocations and femoral head fractures are considered together because a fracture of the femoral head cannot occur without subluxation or dislocation of the hip and the treatment rationale for both is similar.
II. Hip Dislocations
A. Overview—Dislocations of the hip usually result from moderate to severe trauma. The majority (42% to 84%) occur as the result of a motor-vehicle accident. The remainder are associated with falls from a height, sports injuries, and industrial accidents. Posterior dislocations occur much more commonly than anterior dislocations (89% to 92%). Thirty percent of patients with a hip dislocation do not have an acetabular fracture, and most dislocations without fractures are posterior (approximately 80%). Dislocations with acetabular or femoral fractures are almost always posterior (approximately 90%). Historically, the assumed mechanism for posterior dislocation was dashboard impact. However, newer reports have shown that many of these injuries occur in the right hip, and the mechanism of such injuries is now believed to be related to the driver pressing on the brake with the right foot with the hip held in flexion, adduction, and internal rotation. Anterior dislocations often have an associated femoral head fracture and/or impaction. Hip dislocations have the potential for significant long-term disability. Early literature showed poor results with frequent early arthritis and avascular necrosis (AVN). These early reports predated modern imaging modalities and current understanding of the vascularity of the femoral head. It is hoped that by incorporating recent advances, the results of the treatment of patients with these injuries can be improved.
1. Historical overview—The modern phase in the management of dislocations of the hip dates from Henry Jacob Bigelow’s publication in 1869. The clinical presentations and reduction maneuvers described are the same as those used today. In the 1950s, Thompson and Epstein’s classification system and Stewart and Milford’s classification system were devised. Trueta’s description of the vascularity of the femoral head was also published in this time period. It was not until the advent of computed tomography (CT) in the 1970s that the treatment of hip dislocations evolved to its present state.
B. Evaluation—The patient must be examined completely for associated injuries, particularly when the patient is unable to cooperate. Any injury to the pelvis, femur, or knee should raise suspicion of an injury to the hip. The position of the leg is often an indicator of hip dislocation, but this sign may be absent if there is a concomitant ipsilateral femoral neck or shaft fracture.
1. Clinical examination
• Observation—Injuries to the soft tissues near the femur can localize the point of impact. Since dashboard injuries can cause hip dislocations, the physician should look for bruising about the knee. The resting position of the leg often indicates a dislocation. With a posterior dislocation, the leg is shortened and is held in flexion, adduction, and internal rotation. However, often with an irreducible posterior dislocation, the leg may rest in a neutral position. With an anterior dislocation, the leg is held in external rotation, abduction, and mild flexion or extension. The amount of flexion/extension depends on whether the dislocation is superior (pubic) or inferior (obturator).
• Palpation—A feeling of fullness in the soft tissues in the direction of displacement of the femoral head may be palpable.
• Neurovascular examination—Sciatic nerve injuries occur in 8% to 19% of posterior dislocations, mandating documentation of neural function at presentation. The peroneal distribution of the sciatic nerve is involved more often and usually more severely affected than the tibial distribution.
2. Radiographic evaluation—Plain films should always be obtained to look for associated fractures before any reduction attempt. A CT scan should be obtained, if time permits, before irreducible dislocations are taken to the operating room (OR) and after all reductions.
• Plain films—An initial screening anteroposterior (AP) pelvis radiograph is required to evaluate for a suspected dislocation. When evaluating the plain films, the clinician should first look for associated injuries, paying particular attention to the femoral neck, femoral shaft, and acetabulum. The clinician should then carefully compare the congruency of the hip joints. The head of an anteriorly dislocated hip appears larger on plain radiographs than the contralateral normal hip; a posteriorly dislocated hip appears smaller (Fig. 17-1). If a dislocation is suspected, films of the entire femur, including the knee joint, are needed. These films should be carefully evaluated to rule out ipsilateral fractures, in particular nondisplaced fractures of the femoral head, the femoral neck, or the acetabulum. Anteromedial femoral head fractures are most common and will be demonstrated by Judet oblique radiographs. Postreduction plain films in at least two planes (AP and lateral or AP and Judet obliques) must be obtained to evaluate joint congruency and to look for the presence of associated fractures (Fig. 17-2). A postreduction CT is still required because small interposed fragments may be missed on plain films.

FIGURE 17-1 AP Radiograph demonstrates typical appearance of an anterior hip dislocation on the patient’s right and a posterior fracture-dislocation on the left.
• CT—A CT scan of the hip should be obtained after reduction to assess the congruency of the hip joint. This assessment is best done by looking for lateral subluxation in the more proximal cuts that show the hip joint and by comparing the joint space in the more distal cuts of the affected hip to that of the uninjured hip. The postreduction CT scan is also the best means for checking for free osteochondral fragments within the joint (Fig. 17-3). Small foveal fragments may be left, but interposed fragments need to be addressed. If a hip cannot be closed reduced, and if time permits, an emergent preoperative CT scan is recommended to determine whether there are fragments within the joint that will necessitate an open reduction. After open reduction, even if a prereduction CT scan was obtained, a postreduction CT scan is advisable if there is any question regarding the concentricity of the reduction.
• Magnetic resonance imaging (MRI)—MRI can be useful for assessing the hip that has been reduced and has been found to be incongruent but without interposed tissue on CT scan. The MR image is better at evaluating the labrum, the muscles, and the capsule that may be incarcerated within the joint. The role of MRI in the assessment of early AVN, bone bruises, and chondral injuries after hip dislocations has yet to be established. MRI may also show damage to the obturator externus muscle, which may represent injury to the medial circumflex femoral artery and possibly an increased risk of avascular necrosis.
FIGURE 17-2 Postreduction radiograph of the patient shown in Figure 17-1.
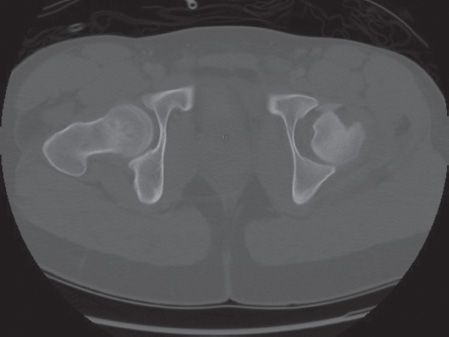
FIGURE 17-3 Axial CT scan demonstrates an incarcerated femoral head fragment.
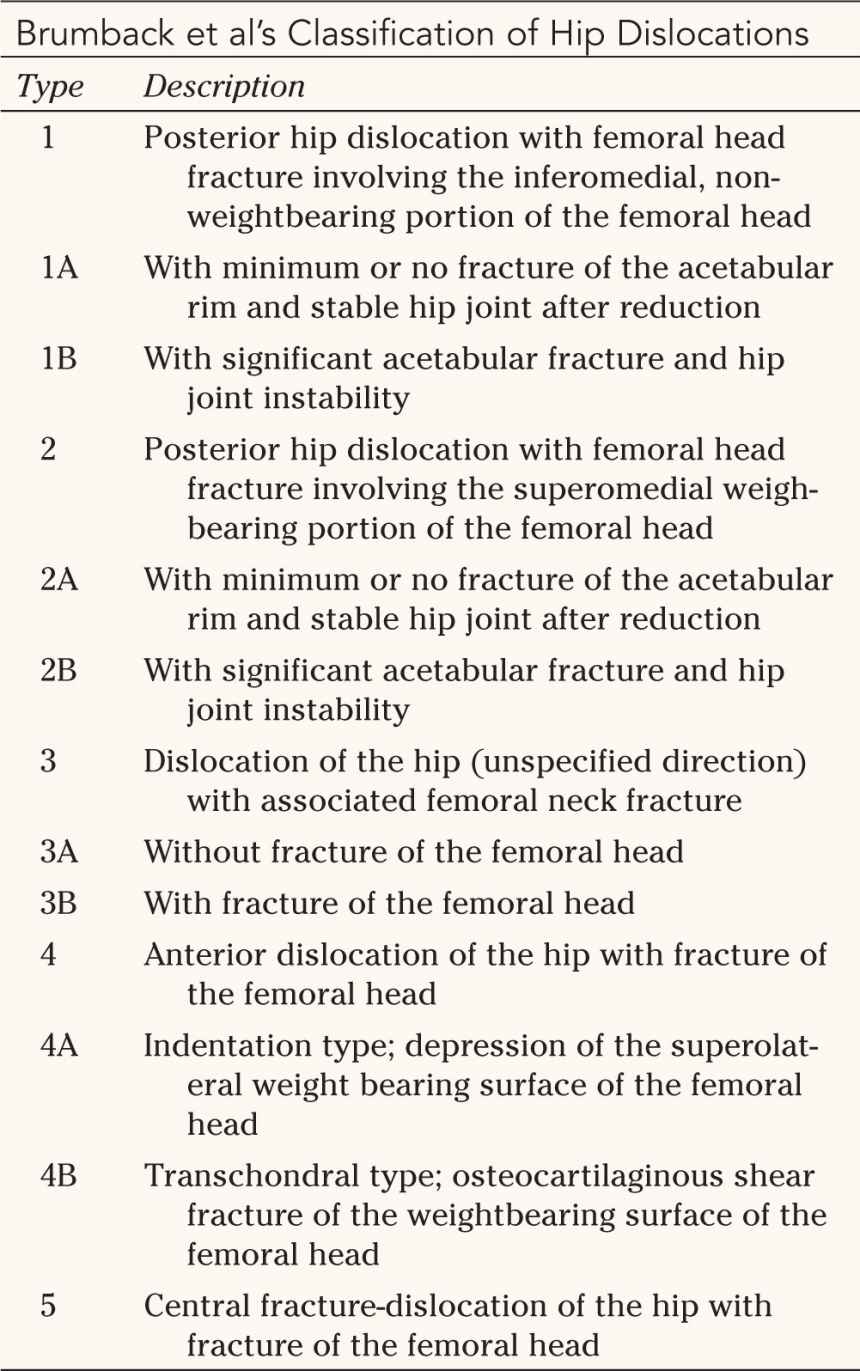
C. Classification (Tables 17-1 to 17-4)—A classification system should help guide treatment and have prognostic value. The two modern classification systems (Comprehensive system and Brumback et al. system) guide clinicians more in terms of treatment than prognosis. The two historical systems (Thompson and Epstein system and Stewart and Milford system) were introduced before the advent of CT. If there is an associated fracture requiring treatment, the prognosis of the injury is usually determined by the quality of the reduction of the associated fracture. The prognosis of a pure dislocation is determined by the incidence of AVN and chondral injuries, both of which are difficult to determine in the immediate postreduction period.

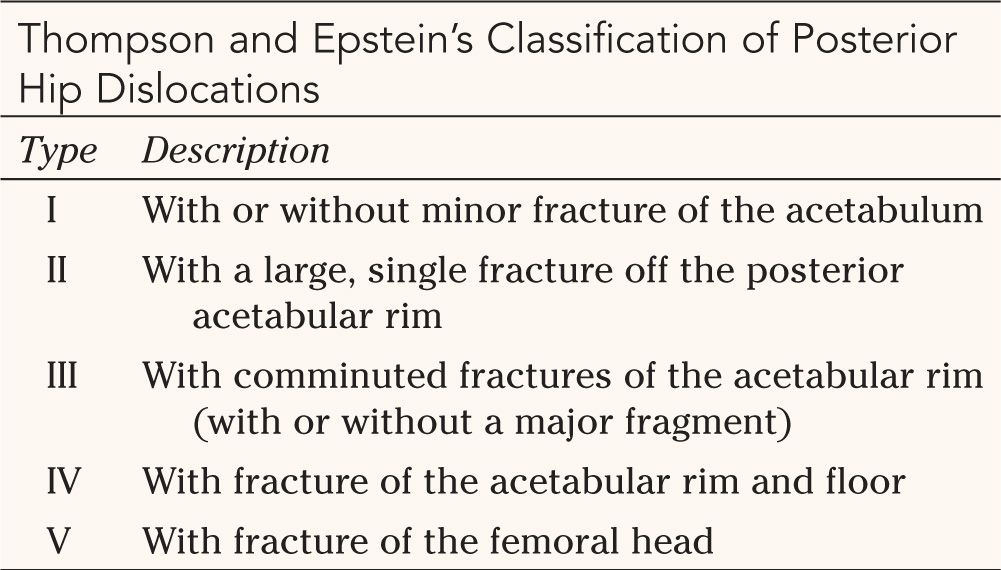
Source: From Thompson VP, Epstein HC. Traumatic dislocation of the hip: a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg. 1951;33A: 746–778, with permission.


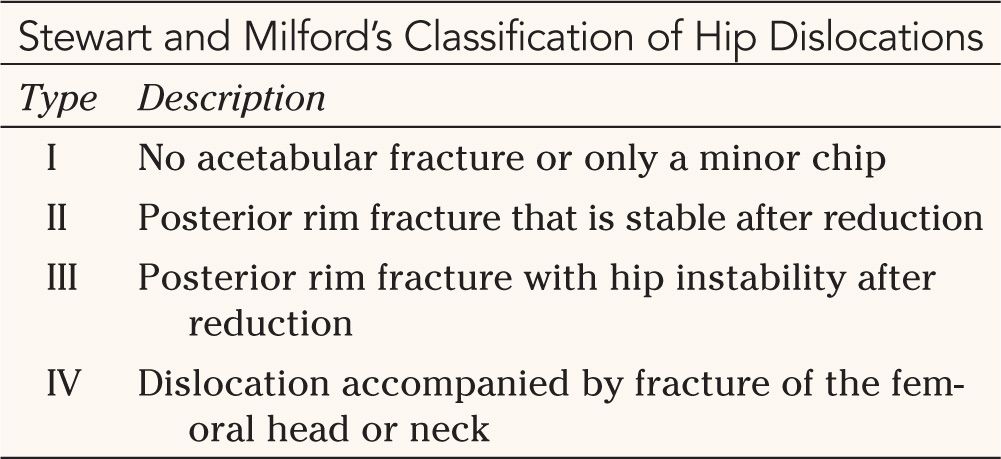
Source: From Stewart M, Milford LW. Fracture-dislocation of the hip: an endresult study. J Bone Joint Surg. 1954;36A:315–342, with permission.


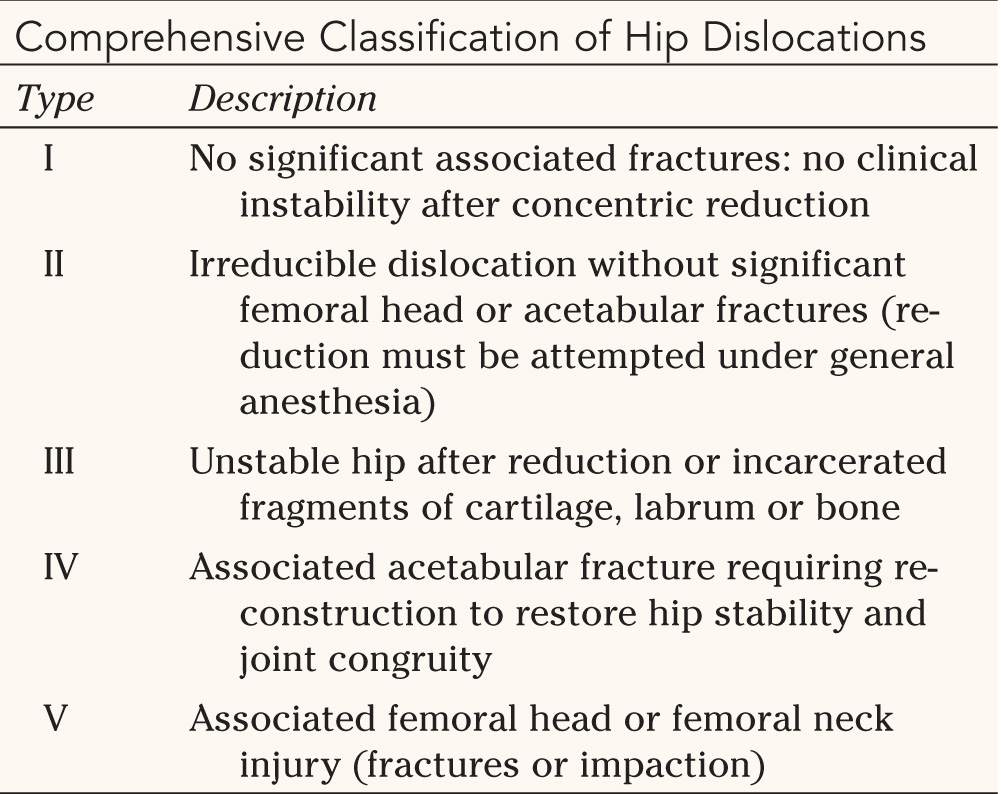
Source: From Levin PE. In: Browner BD, Jupiter JB, Levine AM, et al, eds. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries. Vol 2. 2nd ed. Philadelphia, PA: WB Saunders; 1998, with permission.


Source: From Brumback RJ, Kenzora JE, Levitt LE, et al. Proceedings of the Hip Society 1986. St. Louis, MO: Mosby; 1987, with permission.

1. Thompson and Epstein (1951)—The classification system of Thompson and Epstein is based on the severity of the acetabular and/or femoral head fracture (Table 17-1).
2. Stewart and Milford (1954)—The classification system of Stewart and Milford is based on the stability of the hip after reduction and the condition of the femoral head (Table 17-2).
3. Comprehensive classification—The Comprehensive classification system is based on the reducibility of the hip, the presence of interposed fragments, the stability of the reduced hip, and associated fractures (Table 17-3).
4. Brumback et al.—The classification of Brumback et al. is based on the direction of dislocation and associated fractures (Table 17-4).
D. Associated Injuries—Associated injuries fall into two categories: those associated with the dislocation and those associated with the precipitating trauma. Additional organ-system injuries occur in 95% of patients with a traumatic hip dislocation secondary to a motor vehicle crash; 33% of patients have other orthopaedic injuries, 15% have abdominal injuries, 24% have closed-head injuries, 21% have thoracic injuries, and 21% have craniofacial injuries.
1. Injuries associated with the dislocation—The injury to the hip is determined by the vector of the traumatic load, the rate of load transmission, the point of load transmission, and the position of the leg at the time of impact. A centrally directed force on an abducted leg fractures the pelvis, the acetabulum, the femur, or a combination thereof. As the force is directed more posteriorly and the leg moves into adduction and flexion, a posterior fracture-dislocation is created; with more adduction, a pure dislocation occurs. A posterior impact or a force on an abducted and extended leg creates an anterior dislocation. As the rate of load transmission decreases, the pelvis can rotate, and pure dislocations become more likely. Conversely, when the rate of load transmission is rapid, the pelvis cannot rotate and a fracture of the acetabulum or the femoral head is more likely. The incidence of femoral head fractures is higher with anterior dislocations because the strong anterior ligaments do not easily allow for subluxation of the hip. The anterior wall of the acetabulum is substantial and resists fracturing more than the posterior wall, so the femoral head becomes the weak link and is fractured by the shear force.
• Local bony injuries
(a) Acetabular fractures—One study reported that 70% of patients with hip dislocations had an associated acetabular fracture. Fracture of the posterior wall is most common, but as force is directed more medially, any fracture pattern is possible.
(b) Femoral head fractures—Femoral head fractures are covered in more detail later in this chapter but can include impactions as well as fractures. Most femoral head fractures (90%) are seen with posterior dislocations since posterior dislocations are so much more common than anterior dislocations. However, a higher percentage of anterior dislocations have an associated femoral head fracture (68%) as compared to posterior dislocations (7%).
(c) Femoral neck fractures—Femoral neck fractures are uncommon in patients with hip dislocation. Prereduction films need to be carefully assessed for displaced and nondisplaced fractures along the femoral neck.
(d) Femoral shaft fractures—Femoral shaft fractures are uncommon in patients with hip dislocation. These fractures make leg position no longer predictive of dislocation, and the leg cannot be used as a lever arm during reduction maneuvers.
(e) Patellar fractures and knee dislocations—Patellar fractures and knee dislocations highlight the importance of X-ray films of the joint above and below the injury. If knee pathology is identified and the mechanism of injury is a motor-vehicle accident, there is a high incidence of ipsilateral hip injuries.
• Soft tissue injuries
(a) Blood supply to the femoral head—Multiple sources supply blood to the femoral head. However, the medial femoral circumflex artery (MFCA) is the essential vessel. This vessel anastomoses with a branch of the inferior gluteal vessel at the inferior border of the piriformis and then pierces the capsule deep to the piriformis insertion to run within the synovial reflection to enter the head at the superolateral articular margin (Fig. 17-4). The MFCA vascularizes areas not supplied by other vessels and can supply the entire femoral head. Injury to this vessel by avulsion, transection, thrombosis, or spasm leads to AVN. Posterior dislocations put this vessel at risk, whereas anterior dislocation relaxes the vessel, thus explaining the 2% to 17% rate of AVN with posterior dislocations and the rare incidence with anterior dislocations. Additionally, the MCFA may arise from either the common femoral or more often from the profundus femoral artery. When the MCFA arises from the common femoral artery, a posterior dislocation causes a greater decrease in blood flow to the femoral head. This is theorized to contribute to the variability in AVN rates after dislocation.
FIGURE 17-4 Posterosuperior view of the proximal femur. Note the medial femoral circumflex artery (white arrowhead), the lateral trochanteric vessel (white arrow), and the insertion of the terminal branches into the femoral head (black arrow). (Reprinted with permission from Gautier E, Ganz K, Krügel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679–683.)
(b) Sciatic nerve injuries—Reported rates of sciatic nerve injury range from 7% to 27%. The incidence is approximately 5% in children. These occur exclusively with posterior dislocations, with the highest rate being seen in posterior fracture-dislocations as would be expected from the direction of the displaced posterior wall fragments. The peroneal distribution of the sciatic nerve is more frequently involved than the tibial distribution for unknown reasons, although the posterior portion of the peroneal branch has been implicated because it would be stretched more. The mechanism of injury is proposed to be direct blunt trauma, stretching of the nerve around the posteriorly displaced head, or both. The sciatic nerve variant where the peroneal division branches through the piriformis muscle may place the nerve at increased risk as it is tethered by the piriformis. At least partial sciatic nerve recovery occurs in 60% to 70% of patients, with no clear correlation with injury or treatment.
(c) Ligamentum teres injuries—The ligamentum teres is torn during a dislocation. It can tear mid-substance, or more commonly, it can avulse a small piece of bone from the fovea. If the avulsed piece of bone is interposed between the articular surfaces after reduction, it needs to be removed. However, if it remains in the fovea and does not impinge on the head, it may be left.
(d) Acetabular labrum injuries—The acetabular labrum can be avulsed from the bony acetabular rim on either the side of or the opposite side from the dislocation and can become interposed during reduction. Labral injury can be a source of symptoms even after a successful reduction.
(e) Joint capsule injuries—The joint capsule will be injured during all dislocations. When the femoral head has button-holed through the capsule, reduction can be diificult. The capsule may also become interposed during reduction.
(f) Muscle injuries—The short external rotators are frequently torn during posterior dislocations and may become interposed during reduction. The gluteus medius may be partially avulsed from its femoral insertions during obturator dislocations.
(g) Arterial injuries—Pulses should be evaluated during the physical examination because the femoral artery can be compressed during anterior dislocations.
2. Injuries associated with the trauma—It is important to establish the mechanism of injury to give insight into possible associated injuries.
• Load transmission—The involved limb must be carefully examined from the point of impact all the way to the hip. Foot, ankle, leg, knee, and thigh injuries have all been reported. If the impact was posterior, the pelvis and lumbar spine should be evaluated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









