CHAPTER 33 Hinged External Fixators of the Elbow
INTRODUCTION
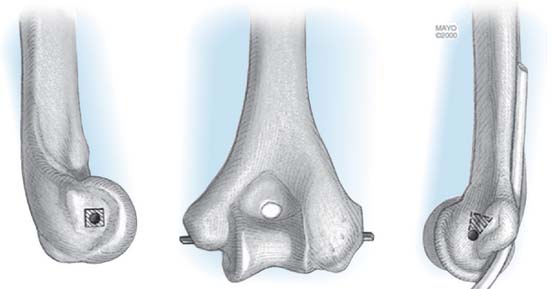
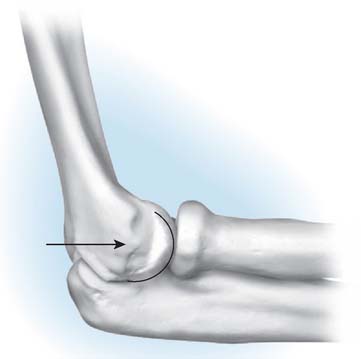
By definition, a dynamic hinged external fixation allows for an axis of rotation to provide elbow stability and motion following trauma or reconstruction.30 With a properly constructed device, the ulna may be separated or distracted from the humerus and still allow physiologic flexion and extension. The mechanics and anatomic landmarks for the application of several fixator devices have been well defined.6,20,28 The axis of rotation of the distal humerus passes through the tubercle of origin of the lateral collateral ligament and through the anteroinferior aspect of the medial epicondyle (Fig. 33-1). Replication of the axis of rotation is essential to avoid pin loosening, persistent stiffness, or instability. In cadaver models, 5 mm of translation or 5 degrees of angulation results in a fourfold increase in resistance to elbow flexion.15
INDICATIONS
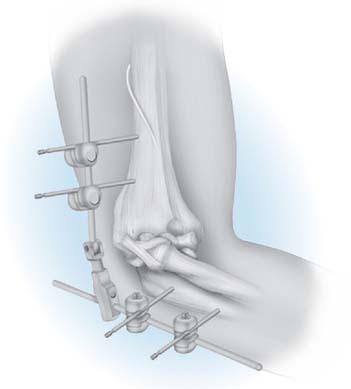
External fixation allows for flexion of the elbow to prevent contracture while still maintaining joint space and appropriate coronal alignment (Fig. 33-2).18 The hinged fixator, when properly applied, maintains a reduced and balanced ulnohumeral joint during motion, thereby protecting repaired or reconstructed collateral ligaments. In trauma, fixators may be used to protect operative fixation of unstable fractures and ligament repair in cases of persistent postoperative instability and for longstanding elbow dislocation or recurrent instability.9 In reconstruction of the elbow, hinged fixators can also be used in the treatment of instability, following ligamentous repair, or with interposition arthroplasty.3,19
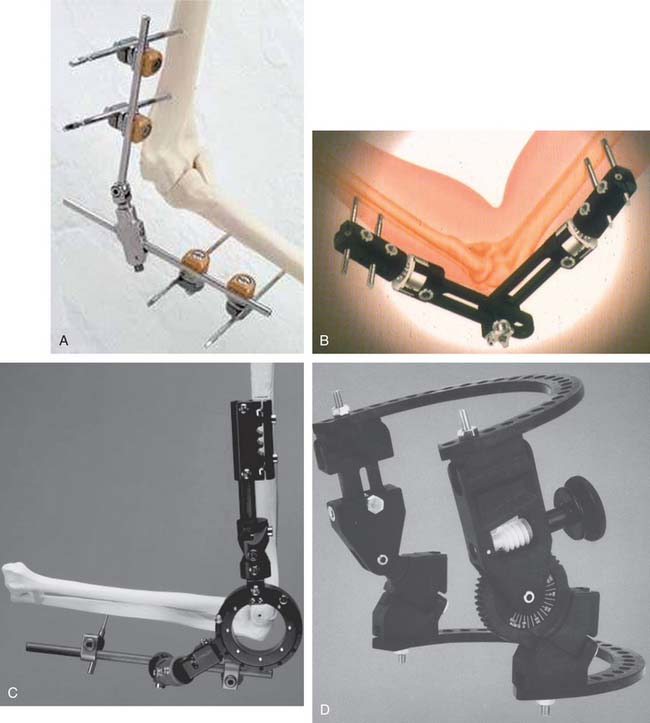
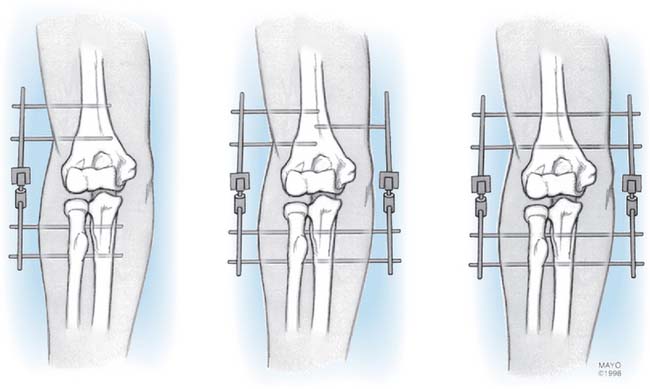
Although goals of treatment may be attained with relatively simple designs, greater flexibility and broader utility have been introduced by Hotchkiss with a more complex fixation. Although several designs are currently available (Fig. 33-3), only the Mayo dynamic joint distractor (DJD)19 and the Hotchkiss Compass Hinge12 are discussed in this chapter because they represent the spectrum from simple to complex.
TRAUMA
Instability
Elbow dislocation with extensive soft tissue injury results in gross instability, even after reduction or repair of involved structures.5 Adjunctive management of late untreated elbow dislocations involve the use of an external fixator.9
Articular Injury (Fracture-Dislocation)
This category includes instability with fractures of the radial head,17,21 some olecranon fractures (Mayo type III)16 as well as Regan-Morrey type II and III coronoid fractures.13,23 Use of a hinged fixator for complex, unstable distal humerus fractures has also been described.7 Open fixation is the primary treatment modality. When gross instability persists or when fixation is deemed vulnerable, an external fixator can be added to allow for immediate postoperative motion and neutralization or unloading of the stresses placed on the fracture fixation (Fig. 33-4).
Residual or Recurrent Subluxation
Residual or recurrent subluxation after simple or complex fracture-dislocation is the third indication for use of a fixator.24 In this setting, percutaneous fixator application can assist in reducing a subluxated joint without having to revert to an open procedure. Maintenance of the device allows for early motion with minimal risk of frank redislocation or continued subluxation. The added stability facilitates proper healing of the capsule and soft tissue restraints.
RECONSTRUCTION
The same basic goals obtain for the use of the fixator after reconstructive interventions.
Ankylosis
When arthrolysis for the post-traumatic joint stiffness is carried out, release of the collateral ligament is sometimes necessary, as well as excision of capsular and bone restraints.8,19 These releases can result in instability. Application of the device protects the repaired collateral ligaments after the arthrolysis while allowing immediate motion of the stabilized concentric joint.
CONTRAINDICATIONS
RELATIVE CONTRAINDICATIONS
SELECTION OF FIXATOR CONFIGURATION
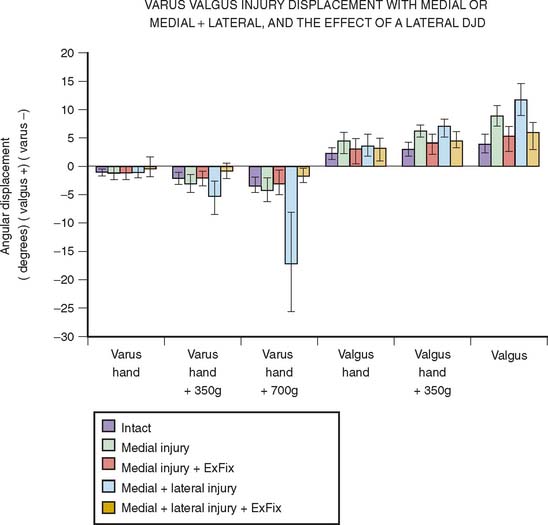
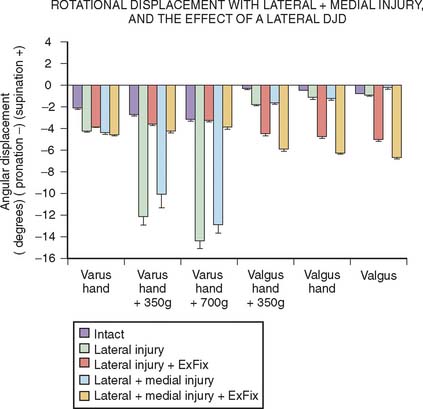
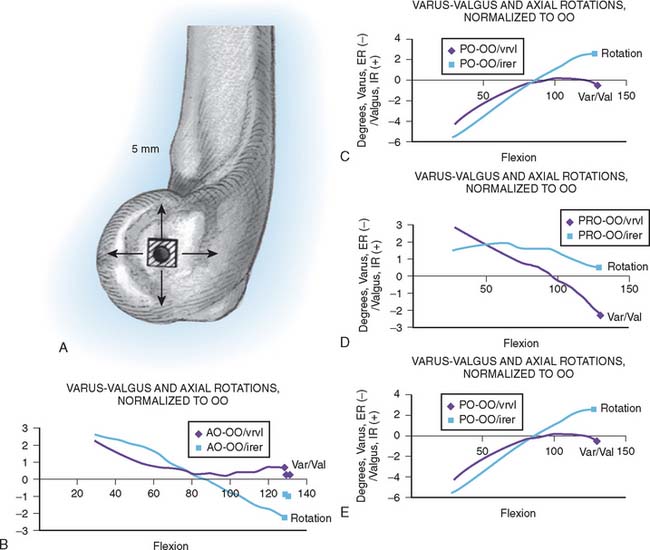
Over the last several years, a number of experiments have been conducted in our laboratory to better understand the function and indications for external fixator configuration. One such assessment demonstrated that compression across the joint with the half-pin lateral application of an external fixator doubles the stiffness of the system in varus load when in extension but had much less effect otherwise. Thus, distraction, one of the recommended applications of the articulated external fixator, does render this system less stable than when the articulation is compressed.27 Of particular importance is the study of Kamineni et al.10 which released the medial and lateral collateral ligaments and assessed the kinematic pattern with a half-pin laterally applied external fixator. In this experiment, it was demonstrated that both varus and valgus stability was restored even with the half-pin lateral configuration and even with up to 7 N out of plane load applied to the forearm (Fig. 33-6). Rotational stability, however, was not as reliably restored (Fig. 33-7). An additional clinical relevant experiment sought to assess the sensitivity of pin placement approximating the axis of rotation. It has been shown that increased energy is needed to move the elbow if a nonoptimum application of the articulated external fixator occurs.15 A subsequent assessment in our laboratory demonstrated that the nonoptimum placement of an external fixator, however, did not alter the kinematics as much as had been anticipated (Fig. 33-8). Based on these data, it was concluded that a slight proximal placement of the axis of the external fixator actually enhances the rigidity of the elbow in a manner that would favor reconstruction of the lateral ulnar collateral ligament. Thus, there may be instances in which slight nonanatomic axis placement is clinically acceptable.2
TECHNIQUE
MAYO DYNAMIC JOINT DISTRACTOR
Author’s Surgical Technique
The patient is supine with a sandbag under the scapula, and a nonsterile tourniquet is applied. The arm is draped free and brought across the chest. In most cases of trauma or reconstruction, a posterior skin incision is used and the elbow joint is exposed either medially or laterally according to the pathologic condition being addressed.
Applying the DJD II External Fixator
Once the elbow has been exposed and the pathologic condition addressed including collateral ligament repair/reconstruction, the external fixator is applied. Several possible configurations are available and are used depending on the lesion and surgeon preference (Fig. 33-9). As noted earlier, we employ the lateral half-pin configuration almost exclusively today.
AXIS IDENTIFICATION
The essential landmarks of the flexion axis are identified. On the lateral aspect of the capitellum, a tubercle is present at the site of origin of the lateral collateral ligament, which represents the geometric center of curvature of the capitellum (Fig. 33-10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree