Fig. 1
Nonoperatively treated calcaneus fracture with resultant post-traumatic arthritis. Note the loss of height and obvious articular incongruity and joint space narrowing. The patient had no anterior ankle impingement or pain and was treated with an in situ subtalar arthrodesis
Osteoarthritis is the second most common and is commonly associated with a deformity (pes planus secondary PTTD or cavus).
Others include inflammatory arthropathy, osteonecrosis, gout, or rarely septic arthritis.
Pathophysiology
Post-traumatic articular incongruity leads to abnormal joint contact forces and loading, resulting in mechanical wear.
Deformity/instability can also lead to joint subluxation, decreased contact area, and increased contact pressure.
Post-traumatic deformity, end-stage posterior tibialis tendon disorder (PTTD), tarsal coalitions, and cavovarus are commonly associated.
Inflammatory processes such RA lead to articular cartilage destruction and wear.
Abnormal purine metabolism results in precipitation and deposition of monosodium urate crystals in joint spaces, resulting to severe inflammatory response.
Radiography
Weight-bearing x-ray (AP, lateral, and oblique views) of the hindfoot
Joint space narrowing or loss (Fig. 2)

Fig. 2
Joint space narrowing in a patient who has isolated talonavicular (arrow) arthritis
Subchondral sclerosis/cysts
Osteophytes and bony erosions
Hindfoot malalignment and deformity (Fig. 3)

Fig. 3
The severe malalignment of the hindfoot precludes visualization of the hindfoot joints in particular the subtalar joint in patients with a pes planus deformity. In these cases, this may be misinterpreted as subtalar DJD. A CT is appropriate in these cases to determine viability of the joints to determine if the patient is a candidate for joint salvage or requires an arthrodesis
Computed tomography (CT) scan
In the setting of deformity, the obliquity if plain radiographs prevent appropriate visualization of the joints. CT is critical in these cases to accurately determine the presence of articular erosion.
Classification
Based on Etiology
Mechanical (post-traumatic)
Degenerative (osteoarthritis)
Inflammatory (rheumatoid, seronegative spondyloarthropathy)
Metabolic (gout, pseudogout (chondrocalcinosis))
Neuropathic
Treatment
Nonoperative
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Activity modification (avoidance of impact and uneven ground)
Bracing such as an ankle-foot orthosis (AFO) or rigid lace up brace such as Arizona brace with an associated rocker bottom shoe modification
Corticosteroid/anesthetic injections: both diagnostic and therapeutic
Treatment of underlying causes such as gout, RA
Operative
Failure of nonoperative treatment with persistent pain and disability is an indication for arthrodesis. Goal of surgery is to obtain a solid fusion and position the hindfoot in 0–5° of valgus, neutral abduction/adduction, congruent talus-first metatarsal axis (Meary line) and create a plantigrade foot (Fig. 4). In many patients a concomitant contracture of the Achilles tendon is present, and an Achilles lengthening should be considered at the time of arthrodesis if a fixed equinus contracture is present.


Fig. 4
Postoperative clinical appearance of a patient s/p subtalar and talonavicular arthrodesis for a severe pes planus deformity. Note the neutral adduction/abduction and restoration of the longitudinal arch
Single joint fusion is indicated for isolated joint arthritis. However, isolated joint fusions, especially TN (TN > ST > CC), are associated to severe hindfoot motion limitation and higher nonunion rate. As such, fusion procedures usually involve ST and TN fusion or triple (ST, TN, and CC) fusion (Fig. 5).

Fig. 5
Attempted isolated TN fusion that resulted in a nonunion (a) that was successfully revised with a combined TN and ST fusion (b)
In the setting of stage 3 PTTD, a TN and ST fusion without violation of the CC joint may be employed. In many cases additional midfoot correction is required to obtain a plantigrade foot (Fig. 6).

Fig. 6
The radiographic appearance of the patient in Fig. 4 with collapse of the medial arch and subtalar DJD noted on CT (a). Postoperative radiograph demonstrating restoration of the arch and additional 1 TMT fusion that was required to create a plantigrade foot (b)
A triple arthrodesis is an effective strategy to treat pan hindfoot arthritis and deformity and is typically required for any congenital deformity.
Subtalar bone block arthrodesis is an effective option to treat post-traumatic arthritis secondary to a calcaneus fracture with loss of height. This operation is only indicated if the patient has ankle impingement (pain or limited dorsiflexion). The higher risk of nonunion and technical difficulty is why this should not be performed if the patient is asymptomatic in the ankle.
Tibiotalocalcaneal (TTC) fusion is an option for subtalar arthritis with associated tibiotalar arthritis or if there is a concern for bone stock and fixation as may seen in neuroarthropathy or sever osteonecrosis.
Complications
Wound complications: Higher in a lateral approach for subtalar joint in severe pes planus deformity and bone block arthrodesis s/p calcaneus fractures.
Nonunion risk factors: prior ankle arthrodesis, isolated TN fusion, and smoking
Malunion: Resultant malposition of foot and abnormal joint loading. Post-traumatic talar neck fractures with varus require a triple arthrodesis to prevent persistent cavovarus deformity.
Adjacent joint arthritis: The ankle is most common.
Bibliography
1.
Anand P, Nunley JA, DeOrio JK. Single-incision medial approach for double arthrodesis of hindfoot in posterior tibialis tendon dysfunction. Foot Ankle Int. 2013;34(3):338–44.
2.
Herscovici D, Sammarco GJ, Sammarco VJ, Scaduto JM. Pantalar arthrodesis for post-traumatic arthritis and diabetic neuroarthropathy of the ankle and hindfoot. Foot Ankle Int. 2011;32(6):581–8.
3.
Radnay CS, Clare MP, Sanders RW. Subtalar fusion after displaced intra-articular calcaneal fractures: does initial operative treatment matter? J Bone Joint Surg Am. 2009;91(3):541–6.
4.
Rammelt S, Zwipp H. Corrective arthrodeses and osteotomies for post-traumatic hindfoot malalignment: indications, techniques, results. Int Orthop. 2013;37(9):1707–17.
5.
Rammelt S, Pyrc J, Agren PH, Hartsock LA, Cronier P, Friscia DA, et al. Tibiotalocalcaneal fusion using the hindfoot arthrodesis nail: a multicenter study. Foot Ankle Int. 2013;34(9):1245–55.
2 Ankle Instability
Take-Home Message
The lateral ligamentous complex is most commonly involved (ATFL > CFL > PTFL).
Nonoperative management is the first-line treatment for all acute injuries → therapy (peroneal strengthening and proprioception) and functional bracing.
Surgical reconstruction indicated for persistent instability → Anatomic repair is most appropriate first-line treatment (Brostrom-Gould).
Concomitant hindfoot varus may require lateral slide/closing wedge calcaneal osteotomy.
Introduction
Acute injuries → Traumatic injury to the lateral ligamentous complex presenting with pain, swelling, and ecchymosis.
Chronic instability → Repeated episodes of “giving way” or recurrent ankle sprains without significant trauma.
These symptoms can be debilitating to athletes, and recurrent ankle sprains are felt to be an etiologic factor for ankle arthritis.
Etiology
Injury and incompetence of the ligamentous structures (most commonly laterally)
Certain factors put patient at risk for ankle instability:
Mechanical: varus hindfoot alignment, generalized ligamentous laxity
Functional: muscle weakness (peroneal tendons), impaired proprioception, and impaired neuromuscular control
Suggested mechanism of injury → inverted, plantar flexed foot with an internally rotated hindfoot, and an externally rotated leg
Can lead to chronic instability
Pathophysiology
Ankle Joint Stability
Lateral ligamentous structures: most commonly involved (medial side rarely injured). Always compare to contralateral lower extremity.
Anterior talofibular ligament (ATFL) (Fig. 7) → most commonly injured → once injured, causes stress on the remaining ligaments; tested by anterior drawer test (Fig. 8). Also assessed with inversion in plantarflexion.

Fig. 7
Intraoperative photograph of the ATFL (white arrow)
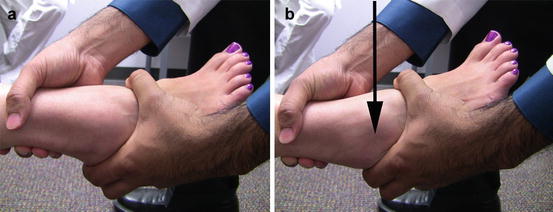
Fig. 8
To perform the anterior drawer test, ne hand stabilizes the anterior distal tibia, while the other is cupped around the posterior calcaneus (a). The heel is translated anteriorly with respect to the tibia, and any subluxation should be noted (b). Note the sulcus that is created over the anterolateral ankle with an unstable ankle (arrow)
Calcaneofibular ligament (CFL) (Fig. 9) → second most commonly injured; tested by talar tilt stress (inversion test) in dorsiflexion (Fig. 10)
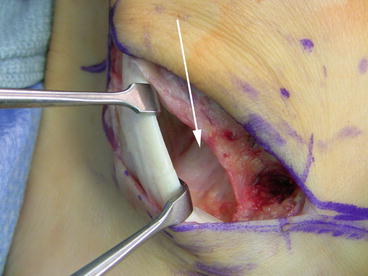
Fig. 9
Intraoperative photograph of the CFL (white arrow). Note how the fibers become taught with dorsiflexion of the ankle

Fig. 10
Inversion stress test in a patient with severe laxity of the CFL
Posterior talofibular ligament (PTFL)
Can check joint hyperlaxity by calculating the Beighton score. Signs of ligamentous laxity should be evaluated using the Beighton scoring system. Out of a possible nine points, four points indicates a generalized ligamentous laxity.
5th finger metacarpophalangeal joint extension past 90° (bilateral, 2 points)
Thumb to volar forearm (bilateral, 2 points)
Hyperextension of the elbow (bilateral, 2 points)
Hyperextension of the knee (bilateral, 2 points)
Hands flat on floor with forward trunk flexion (1 point)
Radiography
Standard weight-bearing anteroposterior, lateral, and mortise views to assess avulsion fractures, arthritis, or osteochondral lesions. A common finding is anterior tibial osteophytes in patient with chronic instability; this must be addressed at the time of surgical intervention (Fig. 11).
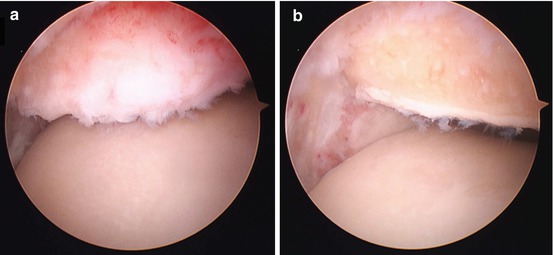
Fig. 11
Anterior osteophytes are identified by their prominence relative to the remaining tibia and by the lack of cartilage inferior to the bone (a). After excision of the osteophyte, the normal articular surface is easily seen (b)
Anterior drawer stress x-ray and talar tilt views are helpful in cases of suspected ankle instability. Absolute values for normal talar tilt vary widely; however, the talar tilt is less the 15° in 95 % of patients (Fig. 12).
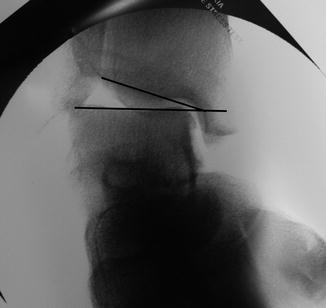
Fig. 12
Varus stress radiograph of a patient with significant talar tilt >15°
MRI → Not required to make the diagnosis of an acute injury. May consider to evaluate for OCLT or syndesmotic injury if appropriate clinical suspicion is given. Recommended in the setting of chronic instability with ankle pain to evaluate for intra-articular pathology (OCLT, loose body, anterior tibial osteophyte, synovitis) given the high incidence of concomitant intra-articular pathology (Figs. 13 and 14).

Fig. 13
Large adhesion in a patient that obliterates the anterolateral aspect of the ankle
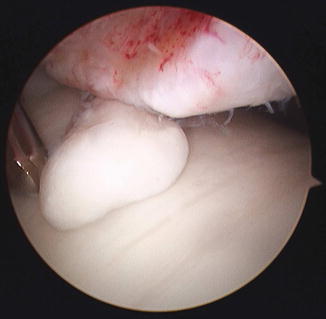
Fig. 14
Loose bodies can be the source of instability in patients who have functional instability without any mechanical laxity. Arthroscopic excision of the loose body is critical in order to relieve the symptoms
Classification
Malliaropoulos classification of acute ankle sprains (Table 1)
Table 1
Malliaropoulos classification of acute ankle sprains
Grade
I
II
III
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access




