23
High Radial Nerve Palsy
Kevin D. Plancher
History and Clinical Presentation
A 31-year-old right hand dominant construction worker fell from a scaffold and sustained a middle to distal third humerus fracture. He came to the emergency room 1 year ago with pain and an inability to perform wrist extension and finger and thumb extension. At that time the emergency room physician placed the patient in a sling and told him to follow up with an orthopedic surgeon. One year, 4 months later, after unsuccessful restoration of his hand and wrist function, the patient comes in, concerned because he is unable to perform any radial nerve function with the hand and wrist.
Physical Examination
The patient has shoulder range of motion of 0 to 165 degrees of forward flexion. External rotation is to 45 degrees. Elbow range of motion is from 0 to 125 degrees. Active wrist flexion is to 50 degrees. Although passively wrist extension is full with a supple joint, active wrist range of motion is not present. Digital range of motion was tested, and the patient was able to flex all digits and the thumb interphalangeal (IP) joint. He could not extend his fingers beyond an M2 grade (Fig. 23–1). There was numbness noted over the dorsal aspect of the thumb and hand. The ulnar and median innervated muscles were tested and found to be intact. All tendons, including radial innervated, were found to be present and working (tenodesis effect).
Diagnostic Studies
Posterior anterior, lateral, and oblique radiographs were taken of the wrist and forearm and showed no bony abnormalities. Anterior, posterior, and lateral views of the humerus were taken and showed a well-healed middle to distal one-third shaft humerus fracture with an intramedullary rod in place with acceptable alignment. An electromyogram (EMG) was originally obtained 4 months after the injury and revealed absent brachioradialis action potentials. The patient had a new EMG showing no change in response to the brachioradialis, as well as no response to the extensor digitorum communis, extensor pollicis longus, as well as to the extensor carpi radialis brevis (ECRB).
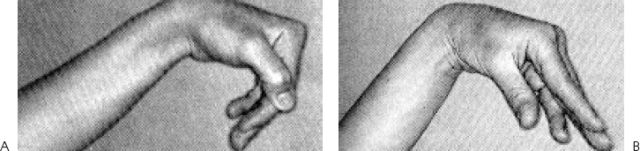
Figure 23–1. (A,B) Clinical photos of a drop wrist with inability to extend metacarpophalangeal (MP) joints due to a radial nerve palsy.
PEARLS
- The Jones/Tsuge/Boyd modified transfer for high radial nerve palsy preserves power grip because it does not use the flexor digitorum superficialis and leaves the flexor carpi ulnaris intact.
- This transfer (Jones/Tsuge/ Boyd) provides independent EPL function.
- In a patient who needs a strong grip but does not need individual finger extension, the use of flexor carpi radialis is often selected for digital extension.
PITFALLS
- The Jones/Tsuge/Boyd modified transfer for high radial nerve palsy requires the presence of a palmaris longus and two fully functional wrist flexors.
- The Jones/Tsuge/Boyd transfer does not provide independent finger extension.
- The Jones/Tsuge/Boyd modified transfer may cause mild ulnar deviation of the wrist.
Differential Diagnosis
Tendon laceration extensor pollicis longus (EPL)
Tendon laceration ECRB, extensor carpi radialis longus (ECRL)
Radial nerve palsy
Mixed nerve palsy
Diagnosis
High Radial Nerve Palsy
The physical examination and diagnostic studies necessitated a discussion about a high radial nerve palsy without any good prognosis for recovery.
Radial nerve injuries that occur in the proximal one third of the forearm result in a low radial nerve palsy (Fig. 23–2). Low radial nerve palsies are characterized by loss of thumb extension, abduction, and finger extension, and by lack of grasp. The level of injury can also be diagnosed by the “hanging of the wrist.” If the wrist is straight, the level is above the elbow. If the wrist is extended but radial deviated (ECRL intact), the level of injury is below the elbow.
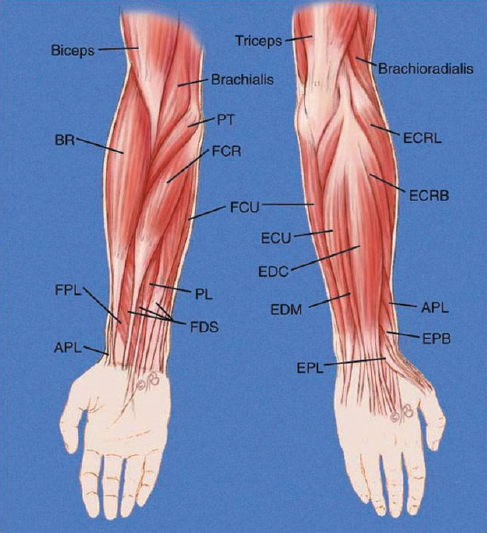
The radial nerve originates on the posterior cord of the brachial plexus, just above the axilla. The nerve passes posteriorly and laterally in close approximation to the humerus throughout its course. The nerve is protected by the long and lateral heads of the triceps. Fractures, such as a displaced spiral oblique fracture, can severely damage the nerve in this area. The sensory branch of the radial nerve becomes subcutaneous underneath the brachioradialis in the distal forearm. The radial nerve provides motor branches to the triceps, brachioradialis, and supinator, and the wrist, finger, and thumb extensors (Fig. 23–3). The radial nerve provides sensory innervation to the posterior and inferolateral arm, posterior forearm, and dorsal radial wrist and hand.
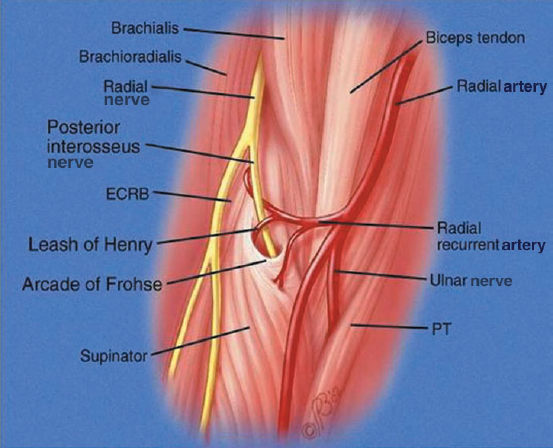
Figure 23–2. Anatomy of radial nerve as it crosses the elbow to branch into the posterior interosseus nerve (PIN).