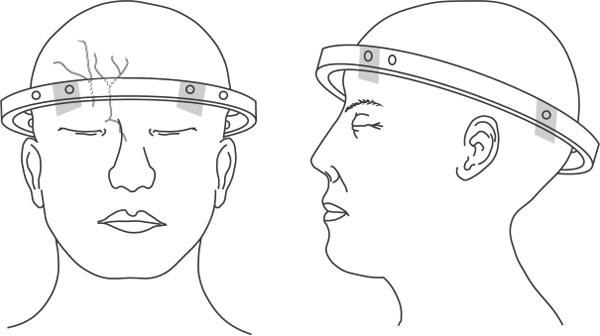
11 Key Points 1. Closed traction reduction is indicated in the setting of cervical fracture, subluxation, or dislocation that causes malalignment and canal compromise in an awake patient capable of giving a reliable neurological exam throughout the process. It is contraindicated in obtunded patients or any patients who have a distracting injury, or patients with skull fractures that preclude placement of tongs or a halo. 2. Stainless steel Gardner-Wells tongs should be utilized for high-weight reductions; reduction using a halo ring should only be performed when low weights will be required. 3. The initial traction weight should be only 5 lb to evaluate for unrecognized atlantooccipital dissociation. Weight is then increased by 10 lb increments added about every 10 minutes (to allow for ligamentotaxis). Serial lateral radiographs and neurological exams are performed after every increase in weight. 4. Once reduced, the cervical spine should be stabilized with either continued traction of ∼ 20 lb or application of a halo vest until definitive surgical fixation is performed. Cervical facet dislocations result from a flexion-distraction mechanism applied to the spine and are due to traumatic failure of the posterior ligamentous construct (facet capsules, interspinous ligament, supraspinous ligament) under tension. Injuries may be purely ligamentous in nature or may be associated with fractures of the articular processes. Bilateral injuries result from a pure flexion-distraction force, whereas unilateral injuries involve flexion-distraction with an accompanying rotational force. Radiographically, unilateral dislocation can be distinguished from bilateral dislocation by an offset of the spinous processes from midline on the anteroposterior cervical radiograph. On the lateral film, the relative rotation of the facet joints above and below the level of injury manifests as the so-called bow tie sign, in which both the right and left facets at a given level can be seen distinctly, as compared with nonrotated levels where the facets are superimposed. Typically, anterolisthesis at the level of injury is less than 25% of the vertebral body anteroposterior diameter. Bilateral facet dislocations, on the other hand, typically result in at least 50% anterior translation. Bilateral perched facets (not fully dislocated) demonstrate relatively large posterior distraction and focal kyphosis of the vertebral endplates. On axial computed tomographic (CT) scans, dislocated facets have a characteristic appearance, with reversal of the normal alignment of the facet joints such that the rounded portions of the articular processes are opposed, rather than the flat articular surfaces (“reverse hamburger bun sign”). Perched facets may manifest on axial CT images as the so-called naked facet sign, in which one articular surface is visualized by itself without its associated counterpart. Cervical facet dislocations frequently present with complete or incomplete spinal cord injuries and represent a situation that requires urgent or emergent decompression. In most cases, once the dislocation is reduced, the local spinal cord compression is alleviated. Whether this emergent reduction is performed via closed or open technique, pre– or post–magnetic resonance imaging (MRI), is still a matter of great debate.1–4 What follows is a technical description of the procedure for closed traction reduction of cervical facet dislocations. Closed reduction can be safely and expeditiously performed in most situations. It requires the application of either Gardner-Wells tongs or a halo ring to the patient’s skull and the use of sequentially increasing traction to distract the dislocated segments and gradually unlock them, allowing reduction of the dislocation. Although weights of up to 140 lb may be safely applied to Gardner-Wells tongs, most manufacturers suggest no more than 35 to 40 lb of traction be applied through a halo ring.5 One of the reasons for this has to do with the pin design and placement. The cranial pins of Gardner-Wells tongs are angled slightly superiorly, which allows them to insert into the skull in a manner allowing greater resistance to longitudinally applied forces. Halo rings, on the other hand, are designed to provide stability in axial, sagittal, and coronal planes but are not designed to resist significant longitudinally applied forces. The angle of insertion of halo cranial pins is perpendicular to the surface of the skull; thus they have decreased pullout strength. In addition, most modern halo devices utilize a carbon fiber ring and titanium pins, which have decreased resistance to pullout compared with stainless steel. Recently, carbon fiber Gardner-Wells tongs have become available that are MRI compatible. Unfortunately, the carbon fiber tongs combined with titanium pins have a certain amount of flexibility or plastic deformity, much more so than stainless steel tongs, and can therefore tolerate lower weights before the stress causes the tongs to bend and the pins to partially disengage, potentially ripping through the patient’s scalp.6 Carbon fiber tongs with titanium can support only ∼ 50–70 lb of force. Any application of a halo ring or carbon fiber tongs requires review the manufacturer’s guidelines for weight tolerance. After reduction, the cervical spine must be stabilized until there is definitive surgical fixation. If surgical fixation is to be performed shortly after reduction, the patient may remain in light traction until surgery. If surgery is to be delayed, or if further studies (e.g., MRI) are to be performed, the patient may be stabilized in a halo orthosis in the interim. For injuries that are amenable to reduction under lighter traction (facet fracture-dislocations, perched facets) it is easiest to apply the halo ring initially and utilize it for the reduction. It may then be locked into the vest. In other cases, such as pure facet dislocations, the need for greater traction will require the use of tongs. In these situations, the halo ring and vest may be applied after reduction is achieved. Closed traction reduction is indicated in the setting of cervical fracture, subluxation, or dislocation that causes malalignment and canal compromise.5,7 Application of a halo ring or Gardner-Wells tongs is contraindicated in patients with skull fractures. In addition, closed reduction may only be performed in an awake patient capable of giving a reliable neurological exam throughout the process. Therefore it is contraindicated in obtunded patients or any patients who have a distracting injury. The technique for applying the halo ring is no different in the setting of cervical dislocation than when it is applied for other purposes. All materials should be gathered at the bedside before starting. This includes material for skin preparation (razor, Betadine, etc.), local anesthetic, all parts of the halo (ring, vest, posts, connectors), and the torque wrenches required for assembly. Several sizes of ring and vest should be available because an ill-fitting vest provides little stability. The patient should be placed on a firm mattress (RotoRest bed, KCI, San Antonio, TX, or a Jackson table, Mizuho OSI, Union City, CA). The patient is carefully logrolled, maintaining cervical precautions, and the posterior half of the vest, with vertical bars attached, is placed behind the patient. During a reduction, placement of a rolled towel between the patient’s shoulder blades, posterior to the vest, can aid in allowing cervical extension if needed. The approximate locations for pin placement are identified, shaved, and prepped. The ring is positioned just inferior to the equator of the skull, leaving at least 1 to 1.5 cm of clearance above the ears. Most halo devices include plastic or rubber pads, which can be placed through screw holes in the ring to aid in positioning. The anterior pin location is over the lateral eyebrow, avoiding the more medially located supraorbital and supratrochlear nerves and the temporal artery laterally (Fig. 11.1).7 Posterior pin placement should be just posterior to the ear, avoiding the mastoid. The underlying skin and subcutaneous tissue are infiltrated with local anesthetic. This is most easily performed by placing the needle through the selected pin hole in the ring. The underlying periosteum should also be anesthetized. The pins are inserted through the selected holes and advanced through the skin until fingertight. A small stab incision at the pin site may be helpful in patients with unusually tough skin or if blunt-tipped pins are utilized. Next, the pins are sequentially tightened to the required torque. This is best accomplished by tightening opposite corners at the same time (e.g., anterior right and posterior left, then switching). Required torque varies based on the manufacturer but is usually 6 or 8 inch-pounds. When the anterior pins are being placed, it is imperative that patients tightly close their eyes or that the surgeon pulls the eyelids down. Failure to do so may allow soft tissue to be trapped by the pin such that the eyelid may be unable to fully close. Fig. 11.1 Placement of the halo ring is just inferior to the equator of the skull, leaving ∼ 1 to 1.5 cm above the ears. Anterior pins are placed over the lateral eyebrow, avoiding the supraorbital and supratrochlear nerves medially. Posterior pins are placed just posterior to the ear, avoiding the mastoid.
Halo Application and Closed Skeletal Reduction of Cervical Dislocations
 Application of a Halo Ring
Application of a Halo Ring
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


