Hallux Limitus and Hallux Rigidus
Thomas J. Chang
Craig A. Camasta
Hallux limitus and hallux rigidus are diagnostic terms that describe a painful, acquired, arthritic condition of the first metatarsophalangeal joint that is characterized by inadequate sagittal plane mobility of the hallux. Aside from hallux valgus, no other condition affecting this joint has received more attention in surgical journals and texts (1). Dorsal bunion (2), hallux flexus (3), hallux equinus (4), hallux limitus (5), hallux rigidus (6), hallux dolorosus (7), and metatarsus primus elevatus (8) are all terms that have been used to describe this condition. The natural history appears to be multifactorial, and various associated factors have been implicated in the origin, but repetitive trauma to the joint is a universally accepted causative factor (3,9, 10, 11, 12).
Hallux limitus and hallux rigidus are clinical terms that are vaguely differentiated, based on the degree of joint immobility and arthritis, with no clearly defined clinical or diagnostic benchmark that separates the two terms. In general, hallux limitus is a precursor state in the progression to hallux rigidus (11,13). Hallux rigidus is the end-stage form of arthritis that approaches bony ankylosis of the first metatarsophalangeal joint. More specifically, the primary factor that differentiates hallux limitus from hallux rigidus in most circumstances is sesamoid mobility. Hallux rigidus is most often characterized by functional ankylosis of the sesamoids to the plantar surface of the first metatarsal.
Lapidus first categorized hallux rigidus based on four etiologic factors: hallux rigidus, paralytic deformities (flaccid and spastic), congenital clubfoot, and severe congenital talipes planovalgus (2). Root et al. attributed hallux limitus to a long first metatarsal, hypermobility of the first ray, immobilization of the first ray, metatarsus primus elevatus, degenerative joint disease, and trauma (14). Nilsonne categorized primary hallux rigidus as developing in adolescent patients with localized degenerative changes and characterized secondary hallux rigidus as a long-standing effect of osteoarthritis (15). Several authors have proposed osteochondritis dissecans as a causative factor (16,17), whereas others believe that hallux limitus precedes osteochondral damage (18).
Investigators have implied that normal gait requires 65 to 75 degrees of dorsiflexion at the first metatarsophalangeal joint (14,19,20). This observation was based on studies of total range of motion, by measuring excursion limits of dorsiflexion and plantarflexion (21). However, Hetherington et al. found that the mean range of motion of the first metatarsophalangeal joint during the contact phase of gait was 31.54 degrees in 12 disease-free patients (22). This is less than half of what was previously reported as “essential” for normal function. Therefore, some discrepancy may exist between the total range of motion at the first metatarsophalangeal joint and the actual range required for normal ambulation. In addition, the required range of motion is likely to vary among patients and with different activity patterns.
CLINICAL FEATURES
Pain is the most frequent symptom in patients with hallux limitus and hallux rigidus, although various compensatory findings accompany arthritic symptoms of the first metatarsophalangeal joint. Whereas hallux valgus is often more painful with shoe pressure, hallux limitus and hallux rigidus may be equally painful when the patient is unshod as well, although certain shoes may create strain on the joint, depending on the patient’s activity (1). Pain in the arthritic first metatarsophalangeal joint is aggravated by activity and footwear that stress-loads and results in impingement of the dorsal aspect of the joint. The degree of discomfort usually is correlated with the level of activity, and it progressively increases throughout the day. With time, a dorsal exostosis typically develops at the first metatarsal head such that direct shoe pressure may exacerbate the pain or may lead to hyperkeratosis. In addition, nerve impingement secondary to chronic pressure can result in paresthesias that radiate distally to the dorsal hallux.
Stiffness of the great toe results in alteration of gait that can transfer load to adjacent joints and can thereby affect the position and function of the foot. Therefore, some patients with hallux limitus may not initially complain of pain
at the first metatarsophalangeal joint if compensatory mechanisms have developed to reduce stress at this level. Associated findings may include pain or pressure-induced hyperkeratoses adjacent to bony prominences, second metatarsophalangeal joint (11), lateral column (23), and plantar aspect of the hallux interphalangeal joint (Fig. 1). In particular, one may note a hyperextension or increased dorsiflexion at the hallux interphalangeal joint as the body attempts to achieve the necessary dorsiflexory motion at this level. The skin beneath the first metatarsophalangeal joint is usually spared weight-bearing pressure, and it is often supple, with little evidence of hyperkeratosis (2).
at the first metatarsophalangeal joint if compensatory mechanisms have developed to reduce stress at this level. Associated findings may include pain or pressure-induced hyperkeratoses adjacent to bony prominences, second metatarsophalangeal joint (11), lateral column (23), and plantar aspect of the hallux interphalangeal joint (Fig. 1). In particular, one may note a hyperextension or increased dorsiflexion at the hallux interphalangeal joint as the body attempts to achieve the necessary dorsiflexory motion at this level. The skin beneath the first metatarsophalangeal joint is usually spared weight-bearing pressure, and it is often supple, with little evidence of hyperkeratosis (2).
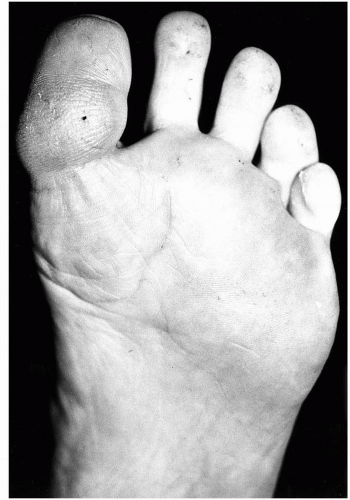 FIG. 1. Pressure-induced hyperkeratosis (tyloma) of the plantar aspect of the hallux interphalangeal joint. This is a common finding in patients with hallux limitus. |
Dannanberg discussed several compensatory mechanisms seen with hallux limitus, including the following: “Lowering of the medial longitudinal arch of the foot is related to the inability of the hallux to extend” (24). If dorsiflexion of the hallux is not sufficient, then retrograde pressure may be directed along the medial osseous structures and soft tissues. Dorsally, compressive forces predominate, whereas plantarly, distraction stresses are evident. Arthritic symptoms may develop at the metatarsocuneiform level initially. Plantar joint pain, plantar fasciitis, or arch strain may be other associated complaints. Conversely, these are conditions may possibly indicate an initial medial column instability, which leads to secondary hallux limitus. Each of these conditions tends to perpetuate the other.
Gait variations have also been described in conjunction with hallux limitus (24). Forefoot inversion provides two potential means of compensation. If sufficient weight-bearing stress to the first metatarsal is relieved, the peroneus longus may be able to achieve a relative functional superiority and appropriately plantarflex and stabilize the metatarsal. Forefoot inversion may also allow the patient to complete toe off by rolling weight off the lateral metatarsals and eliminating the medial column from weight transfer. The same lateral transfer of weight may be accomplished by adducting the foot.
Depending on the degree of compensation required, the symptoms of hallux limitus may range from diffuse lesser metatarsalgia to more discrete symptoms plantar to the fifth metatarsal head. At times, the hyperkeratosis may be located beneath the fourth metatarsal head if the fifth ray is hypermobile. Other findings may include a heloma molle in the fourth web area or complaints of lateral subtalar, lateral ankle, or lateral knee pain.
Another compensatory mechanism is premature lift off. The normal stance weight transfer from heel to metatarsal head to toes is bypassed as the hallux automatically avoids dorsiflexion. Consequently, the toes are lifted off the ground before the metatarsal heads, a process that disrupts efficient energy flow and contributes to digital contractures.
The final means of compensation for hallux limitus is seen most commonly in the geriatric population and consists of vertical toe off with an apropulsive gait. This is an inefficient gait pattern, which results in increased muscular output, fatigue and an increased ratio of double to single limb support.
Examination of the patient’s shoes may reveal a distinct wear pattern that reflects the long-standing nature of this condition (11). Because of restricted motion within the first metatarsophalangeal joint, pressure is transferred to the hallux interphalangeal joint. The typical shoe wear pattern in patients with hallux limitus or rigidus may be concentrated beneath the second metatarsophalangeal joint and hallux interphalangeal joint (Fig. 2). One may see an accentuated oblique angulation at the shoe break that reflects the altered position of the foot in propulsion (3,11,23).
Numerous different means of assessing first metatarsophalangeal joint mobility have been described, and techniques may vary among examiners. This situation makes comparison of data in studies and in the clinical setting difficult in some instances. Care should be taken to assess the first metatarsophalangeal joint independent of the interphalangeal joint, which may be hyperextended or mobile as a result of compensation for metatarsophalangeal immobility. Regardless of the technique employed, evaluating the range of motion in both a relaxed and a loaded manner may prove helpful in more accurately assessing the functional capacities of the first metatarsophalangeal joint. In some patients, limitation of joint mobility is noted only in the loaded or functioning position, whereas the same evaluation in the relaxed position may demonstrate good range of motion. This entity, termed functional hallux limitus (24), often precedes the fixed limitation of mobility or arthritic findings that characterize the advanced forms of hallux limitus and rigidus. Symptoms with functional hallux limitus may be the same
or similar to those in patients with more fixed limitation of motion. Therefore, if the patient possesses functional hallux limitus, a cursory evaluation may lead the examiner to believe that mobility of the first metatarsophalangeal joint is adequate or normal, when instead there is a problematic limitation of motion during gait.
or similar to those in patients with more fixed limitation of motion. Therefore, if the patient possesses functional hallux limitus, a cursory evaluation may lead the examiner to believe that mobility of the first metatarsophalangeal joint is adequate or normal, when instead there is a problematic limitation of motion during gait.
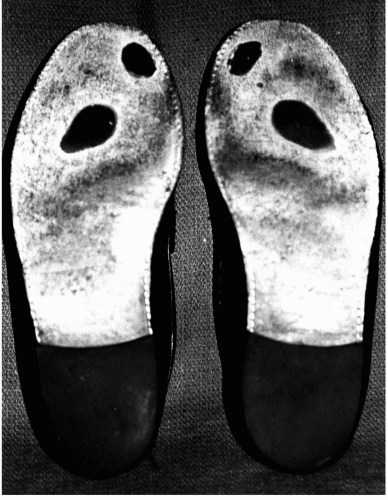 FIG. 2. Shoe wear pattern in an asymptomatic patient with hallux limitus. Note the weight transfer from the second metatarsophalangeal joint to the hallux interphalangeal joint. |
Stance and gait observations may reveal several characteristic findings common to hallux limitus and hallux rigidus. In stance, the hallux may be plantarflexed relative to the first metatarsal, thus accentuating the dorsal prominence of the first metatarsal head (dorsal bunion) (Fig. 3). In gait, the point of ground contact through the first ray may be the interphalangeal joint of the hallux, which hyperextends to accommodate propulsion (2,11).
ETIOLOGY
Pes Valgus Deformity
The most commonly associated condition encountered with hallux limitus or rigidus is flexible pes planovalgus deformity (8,25,26), which is characterized by hypermobility of the first ray (9). The flexible pes valgus undergoes compensation in all planes of motion, and the predominant plane of compensation determine whether a patient will develop an associated hallux valgus or hallux limitus or rigidus deformity. Transverse and frontal plane compensation predisposes to the development of a hallux valgus deformity, whereas sagittal plane compensation predisposes to the development of a hallux limitus or rigidus deformity. Repetitive contracture of the flexor hallucis brevis muscle, in an attempt to stabilize the medial column, leads to plantarflexion of the proximal phalanx on the first metatarsal. In open-chain kinetics, range of motion of the first metatarsophalangeal joint is initially unrestricted, whereas the “loaded” weight-bearing closed-chain kinetic motion is restricted in the direction of dorsiflexion. Initially, the reduction in motion is appreciated only in the functional attitude, that being with weight bearing or simulated weight bearing. If one evaluates the range of motion of the first metatarsophalangeal joint at this stage in a non-weight-bearing, relaxed position, then full pain-free mobility is typically present. However, if the foot is loaded and the motion is evaluated, a reduction in mobility will be noted, indicative of the early contracture of the plantar tissues. This condition was termed functional hallux limitus by Dannanberg (24). Patients may present with symptoms consistent with hallux limitus, yet without gross changes in the joint or surrounding osseous structures and with an apparently normal range of motion on initial evaluation.
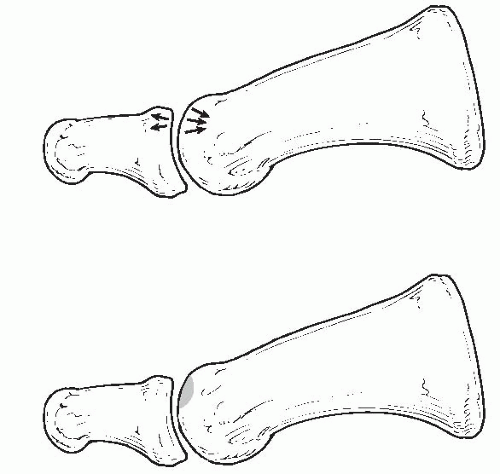
As the condition persists, adaptive changes occur within the joint, and arthrosis results from repetitive impingement of the two adjacent articular surfaces. This observation has been termed flexor stabilization of the hallux and is analogous to a flexor stabilization hammer toe, both of which can coexist in the same patient (27). In this description of hallux limitus or rigidus, the distal phalanx is relatively dorsiflexed on the proximal phalanx, whereas the proximal phalanx is relatively plantarflexed on the first metatarsal. Analogous osseous positions occur in a lesser digit hammer toe, with the proximal phalanx of the hallux corresponding to the middle phalanx of a lesser digit and the first metatarsal corresponding to the proximal phalanx of a lesser digit.
Length Pattern Aberrations
Several associations have been made between hallux limitus or rigidus and the length of the osseous segments that
make up the first ray and its relation to the lesser tarsus. A long first metatarsal may lead to excessive loading of the joint and eventual adaptive or degenerative changes (12,15,26,28). Paradoxically, a short first metatarsal may also serve as an indirect source of hallux limitus (29,30). Patients with a short first metatarsal may experience lesser metatarsalgia and may “grip” the ground with the hallux in an attempt to reduce the symptoms in the lateral forefoot. Over time, this hyperactivity of the flexor hallucis brevis may lead to adaptive contracture and eventual loss of motion. Likewise, any condition that creates lesser metatarsalgia may similarly lead to a hallux limitus regardless of the length of the first metatarsal. Retrograde pressure from a long proximal phalanx against the first metatarsophalangeal joint has also been proposed as another cause of hallux limitus (31).
make up the first ray and its relation to the lesser tarsus. A long first metatarsal may lead to excessive loading of the joint and eventual adaptive or degenerative changes (12,15,26,28). Paradoxically, a short first metatarsal may also serve as an indirect source of hallux limitus (29,30). Patients with a short first metatarsal may experience lesser metatarsalgia and may “grip” the ground with the hallux in an attempt to reduce the symptoms in the lateral forefoot. Over time, this hyperactivity of the flexor hallucis brevis may lead to adaptive contracture and eventual loss of motion. Likewise, any condition that creates lesser metatarsalgia may similarly lead to a hallux limitus regardless of the length of the first metatarsal. Retrograde pressure from a long proximal phalanx against the first metatarsophalangeal joint has also been proposed as another cause of hallux limitus (31).
Uncompensated Varus Deformity
Uncompensated frontal plane inversion, regardless of the level of occurrence, prevents the forefoot from contacting the ground in midstance and propulsion. Varus deformities can occur at any level, including the knee, leg, ankle, rearfoot, or forefoot. Sagittal plane elevation of the medial column prevents the first metatarsal head from bearing full weight, and compensation occurs within the first metatarsophalangeal joint through plantarflexion of the proximal phalanx on the first metatarsal (8). The hallux thereby assumes a position of equinus (hallux equinus) relative to the first metatarsal (27). Contracture of the flexor hallucis brevis muscle allows the hallux to contact the ground and to bear weight through the hallux interphalangeal joint (2). Over time, the first metatarsophalangeal joint becomes fixed in equinus, and arthrosis follows, as previously described.
A varus deformity leading to hallux limitus or rigidus can occur in congenital conditions such as a forefoot varus, uncompensated or partially compensated rearfoot varus, or residual clubfoot, in acquired conditions such as a tarsal coalition or peroneal spastic flatfoot, or after a malpositioned proximal fusion, the most common of which includes ankle, pantalar, subtalar, or triple arthrodesis (32).
Postsurgical Complications
Malunion of a first metatarsal osteotomy, most commonly seen after bunion surgery, can lead to sagittal plane elevation or excessive shortening of the first metatarsal bone (33). This condition most commonly occurs after displacement of a proximal metatarsal osteotomy (Fig. 4). However, it can also be observed in distal metaphyseal osteotomies (Fig. 5). In essence, postoperative metatarsus primus elevatus is a localized form of forefoot varus that occurs within the architectural structure of the first metatarsal bone.
Hallux limitus can also occur after hallux abducto valgus surgery. Limited motion may ensue after any reconstructive procedure involving a joint, and limited dorsiflexion can occur after bunion surgery in the absence of any specific untoward events, depending on the degree of capsular adhesions and scarring. Other factors that contribute to hallux limitus or rigidus formation after bunion surgery may include infection, avascular necrosis, displacement or migration of the internal fixation, and various host-dependent factors such as increased age, history of hypertrophic or keloid scar formation, or one of the many connective tissue diseases.
Trauma and Arthrosis
Injuries to the first metatarsal or first metatarsophalangeal joint can predispose to hallux limitus or rigidus. Malunited fractures of the first metatarsal bone with sagittal plane elevatus lead to findings similar to those associated with the iatrogenic type of metatarsus primus elevatus (Fig. 6), whereas intraarticular fracture-dislocations of the first metatarsophalangeal joint can result in traumatic arthritis (Fig. 7). Bingold (11) described fragmentation and bony sclerosis of the basal epiphysis of the proximal phalanx in adolescent patients with painful hallux rigidus and related this to stubbing or crushing injuries of the hallux and poor fitting footwear. Various acquired arthritic conditions, including gout,
psoriatic arthritis, and rheumatoid arthritis, have been implicated (34).
psoriatic arthritis, and rheumatoid arthritis, have been implicated (34).
 FIG. 5. Iatrogenic hallux limitus with intrinsic metatarsus primus elevatus after displacement of a distal metaphyseal osteotomy. |
Osteochondritis Dissecans
Hallux limitus or rigidus has been associated with traumatic defects in the articular cartilage of the first metatarsophalangeal joint. Adolescent hallux limitus or rigidus has been attributed to osteochondritis dissecans of the first metatarsal head (16,17,35); however, adult cases of osteochondritis have been reported with and without a history of trauma (18,36). Whether hallux limitus is a predisposing factor in osteochondral injury remains a topic of debate, although the presence of this injury has been suggested to occur before the onset of pain (11,18).
Osteochondral Fractures
Osteochondral fractures of the first metatarsophalangeal joint occur most frequently on the dorsal distal central aspect of the first metatarsal head, opposite the surface on the base of the proximal phalanx. Impingement of these two opposing joint surfaces creates an impaction of the metatarsal head, and convergence of these forces leads to fracture of the subchondral bone plate, which propagates into the subchondral bone. Disruption of the blood supply to this portion of bone leads to avascular necrosis and subsequent arthrosis of the remainder of the joint. Pain occurs directly from edema within the bone and secondarily throughout the joint from effusion of synovial fluid.
Paralytic Deformities
Lapidus identified three types of paralytic deformities (flaccid or spastic) in which muscular imbalance is accompanied by the formation of a dorsal bunion (2). One such condition was defined as “weakness of the peronei with a strong tibialis anterior and strong flexors of the big toe.” The description of this condition focused on the varus position of the foot and the inability of the medial column to contact the ground. The tibialis anterior tendon maintains the varus position of the foot, whereas the flexors of the hallux contract to purchase the weight-bearing surface. The varus position is the primary deforming force. Iatrogenic dorsal bunions have been described as postoperative sequelae after transfer of the peroneus longus tendon into the tibialis anterior in patients with poliomyelitis (37), a finding lending support to this theory.
The second condition was defined as “weak dorsiflexors of the foot and toes with strong plantarflexors of the big toe and strong calf muscles.” This describes a situation whereby the forces of plantarflexion serve as the primary deforming force, with dorsiflexion of the first metatarsal occurring secondarily to the effect of the hallux on the medial column of the foot. Dorsal bunions have been described after transfer of the extensor hallucis longus into the distal first metatarsal head in which weakening of the extensor tendon allowed the flexor tendons to predominate at the first metatarsophalangeal joint (38).
The third condition was defined as “calcaneus deformity with active plantarflexors of the big toe.” In this category of deformities, the flexor hallucis longus is recruited as an accessory plantarflexor of the foot and thereby leads to hallux equinus and a dorsal bunion.
Goldner described hallux flexus in cerebral palsy and paralytic
patients that resulted from a weak extensor hallucis longus, overpowering tibialis anterior tendon, and spasticity of the flexor hallucis longus or brevis tendon (38). This condition leads to an underlapping of the hallux, as compared with the overlapping hallux that is a frequent component of hallux valgus.
patients that resulted from a weak extensor hallucis longus, overpowering tibialis anterior tendon, and spasticity of the flexor hallucis longus or brevis tendon (38). This condition leads to an underlapping of the hallux, as compared with the overlapping hallux that is a frequent component of hallux valgus.
Other Factors
The presence of a distal pseudoepiphysis at the first metatarsal head has also been associated with subsequent hallux limitus or rigidus (31,39). Classically, a squared articular surface has also been believed to render a patient susceptible to hallux limitus in the presence of mechanical imbalance (40).
ROLE OF THE PLANTAR STRUCTURES: THE NATURAL HISTORY OF ARTHROSIS
Several layers of structures within the plantar arch of the foot influence the function of the first metatarsophalangeal joint, both directly and passively. The flexor hallucis longus has a passive but influential role on first metatarsophalangeal joint function. Recruitment of long flexor function in weight bearing and propulsion locks the interphalangeal joint against ground reactive forces and transfers tension to the proximal metatarsophalangeal joint. The effect on the metatarsophalangeal joint is plantarflexory, with the proximal phalanx assuming an equinus position in relation to the first metatarsal. Plantarflexion of the proximal phalanx creates a dorsiflexory effect on the first metatarsal through retrograde buckling (2). Therefore, forceful contracture of the flexor hallucis longus leads to clawing of the hallux at both the interphalangeal and metatarsophalangeal joints in open-chain kinetics and to true hammering in closed-chain kinetic function.
The plantar fascia has a passive role in restricting motion about the first metatarsophalangeal joint. The distal interdigitations of the medial band of the plantar fascia insert into the base of the digits and create a windlass mechanism, such that dorsiflexion of the digits creates tension on the plantar fascia. In addition to aiding in resupination of the rearfoot during propulsion, the plantar fascia assists in loading the metatarsophalangeal joints. Secondary contracture of the plantar fascia can occur in hallux limitus or rigidus, and it has been addressed surgically as an adjunct to other procedures for this condition (3). The effect of plantar fascia release on first metatarsophalangeal joint mobility has been investigated. Measurements taken before and after fasciotomy demonstrate that on average, dorsiflexion increases by 10 degrees, whereas plantarflexion is not affected (Goecker R, Harton F. Effect of plantar fasciotomy on first metatarsophalangeal joint mobility. Personal communication, 1999).
The flexor hallucis brevis muscle inserts into the sesamoid apparatus and is an important stabilizing influence on the first metatarsophalangeal joint. Many authors have drawn attention to the role of this muscle in the development and propagation of plantar contracture in hallux rigidus. Some have attributed spasm of the flexor hallucis brevis as a causative factor in the development of this process (9,11,12,26), whereas others have recognized the late effects of contracture as a secondary finding (2). Watson Jones advocated a surgical release of the plantar intrinsic musculature as an isolated early procedure in selected cases devoid of significant arthrosis (41). Although controversy exists on the order of events in the natural history of this condition, it is generally well accepted that contracture of the flexor hallucis brevis muscle compounds the degenerative process within the first metatarsophalangeal joint.
Sesamoid degeneration and immobility have been recognized as associated findings in hallux limitus and hallux rigidus (25,42,43). In hallux limitus, sesamoid immobility is less pronounced, and open-chain kinetic range of motion often reveals near-normal joint mobility. However, the “loaded” or weight-bearing joint with hallux limitus typically demonstrates limited dorsiflexion. With hallux rigidus, sesamoid immobility is more clinically significant, because of restriction in both dorsiflexion and plantarflexion, both in open-chain and closed-chain kinetics.
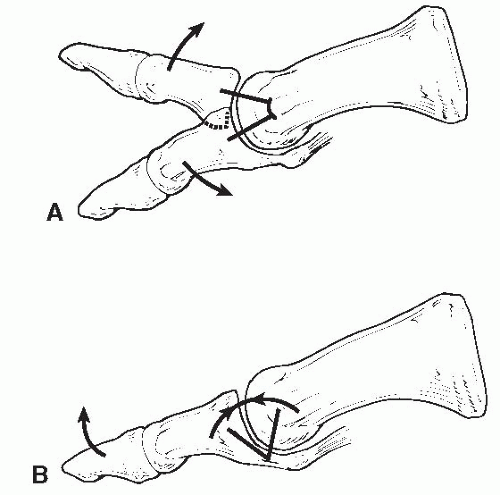
Immobility of the sesamoids, through contracture of the flexor hallucis brevis muscle, prevents gliding of the metatarsal head over the sesamoid apparatus in propulsion (11). The normal axis of rotation is changed from the central aspect of the first metatarsal head (Fig. 8A) to the plantarflexor plate and sesamoid apparatus (44). In this manner, the normal gliding motion is converted to a hinge, with the axis of
rotation occurring outside the joint (Fig. 8B). Hetherington et al. identified four instant centers of rotation of the first metatarsophalangeal joint that occur in closed-chain kinetics (22): “As dorsiflexion begins, there is a rolling initially followed by a sliding, which accompanies first metatarsal plantarflexion. Compression occurs as the joint reaches its end range of motion” and “The final center demonstrates a vector entering the proximal phalanx of the hallux, the characteristic of a compressive force at the end range of motion.” These findings support the theory that sesamoid immobility influences the range of motion in patients with hallux limitus such that they function entirely at the fourth instant center of rotation suggested by Hetherington et al., a center characterized by compressive forces. The identified location of this center of rotation is dorsally, where impingement occurs between the metatarsal head and phalangeal base. Thereafter, the dorsiflexory moment of action about the first metatarsophalangeal joint results in dorsal impingement between the metatarsal head and proximal phalangeal base. Repetitive dorsal impingement leads to an eccentric concentration of pressure on the dorsal articular cartilage, which gradually erodes and fibrillates (17), thereby exposing the underlying subchondral bone plate. Loss of functional articular cartilage initiates the cascade of changes that results in arthrosis (11).
rotation occurring outside the joint (Fig. 8B). Hetherington et al. identified four instant centers of rotation of the first metatarsophalangeal joint that occur in closed-chain kinetics (22): “As dorsiflexion begins, there is a rolling initially followed by a sliding, which accompanies first metatarsal plantarflexion. Compression occurs as the joint reaches its end range of motion” and “The final center demonstrates a vector entering the proximal phalanx of the hallux, the characteristic of a compressive force at the end range of motion.” These findings support the theory that sesamoid immobility influences the range of motion in patients with hallux limitus such that they function entirely at the fourth instant center of rotation suggested by Hetherington et al., a center characterized by compressive forces. The identified location of this center of rotation is dorsally, where impingement occurs between the metatarsal head and phalangeal base. Thereafter, the dorsiflexory moment of action about the first metatarsophalangeal joint results in dorsal impingement between the metatarsal head and proximal phalangeal base. Repetitive dorsal impingement leads to an eccentric concentration of pressure on the dorsal articular cartilage, which gradually erodes and fibrillates (17), thereby exposing the underlying subchondral bone plate. Loss of functional articular cartilage initiates the cascade of changes that results in arthrosis (11).
Osseous impingement erodes the dorsal articular surfaces on the opposing sides of the metatarsophalangeal joint. Loss of functional cartilage stimulates dorsal osteophyte formation in an attempt to increase the surface area of the joint and thereby dissipates the same force over a larger contact surface. Pain can often occur as a late finding, after a significant degree of articular degeneration has already occurred. Splinting and guarding of the joint secondary to pain lead to further adaptive contracture of the plantar structures. Flattening of the joint surfaces further limits motion as the body attempts to restrict painful motion within the joint. Bony ankylosis, the hallmark of hallux rigidus, is the end result of this cyclic cascade—restricted motion, articular degeneration, osteophyte formation, pain, splinting and adaptive contracture, articular flattening, and finally bony ankylosis. Watson Jones (41) proposed and Jack (9) supported this theory, having identified three sequential stages: spasm of the short flexors, secondary contracture of plantar structures, and subsequent osteoarthritis. These investigators believed that the arthrosis of hallux rigidus was identical to that occurring in any joint with osteoarthritis.
Clinical evidence of this theory of cyclic events is apparent through surgical dissection of an arthritic first metatarsophalangeal joint. Synovial membrane thickening is most pronounced at the dorsal half of the joint. Articular erosion is more severe on the dorsal surface of the joint (11,17), because the inferior one-half of the metatarsophalangeal joint is relatively spared early in the arthritic process (9,45). Cupping of the proximal phalangeal base around the metatarsal head is common, as is furrowing of the sagittal groove on the plantar metatarsal head where the sesamoids articulate. Flexor plate and sesamoid immobility is a consistent surgical finding in hallux rigidus.
Microtrauma Versus Macrotrauma
Establishing a direct cause and effect between hallux limitus and arthrosis is difficult to document, because most asymptomatic patients do not seek treatment. Once the cyclic cascade of events is under way, few will argue the relationship between joint immobility and degenerative changes. Most authors agree that both acute trauma and chronic trauma are influential in the development of hallux rigidus (9,17,45). Two distinct groups of patients appear to be afflicted with hallux rigidus: adolescents and middle-aged patients. A higher correlation with osteochondral defects is noted in adolescent patients, whereas adults are more likely to suffer from gradual progressive arthritis.
In effect, hallux rigidus appears to occur by two parallel methods. In both cases, a predisposition to hallux limitus exists, typically in the form of pes planovalgus. In one instance, a macrotraumatic event (stubbing injury, rapidly increased demand) exceeds the capacity of the osseous structures to accommodate dorsal compression, and a fatigue fracture occurs in the metatarsal head (Fig. 9). This lesion is always on the side of the metatarsal head (not the proximal phalanx) because of convergence of compressive forces on the convex surface (18,27) (Fig. 10). The second form of hallux rigidus occurs as a gradual microtraumatic event, in
which repetitive dorsal impingement erodes the dorsal articular surface, but the forces occur gradually so the subchondral bone has a chance to hypertrophy instead of fracture. This is typically the case in the adult form of this condition, because radiographic subchondral sclerosis and osteopetrotic bone are typically encountered at the time of surgery. Regardless of the cause, the cyclic events of adaptive contracture and arthrosis occur in a similar fashion and are identical to osteoarthritis or traumatic arthritis observed elsewhere throughout the body.
which repetitive dorsal impingement erodes the dorsal articular surface, but the forces occur gradually so the subchondral bone has a chance to hypertrophy instead of fracture. This is typically the case in the adult form of this condition, because radiographic subchondral sclerosis and osteopetrotic bone are typically encountered at the time of surgery. Regardless of the cause, the cyclic events of adaptive contracture and arthrosis occur in a similar fashion and are identical to osteoarthritis or traumatic arthritis observed elsewhere throughout the body.
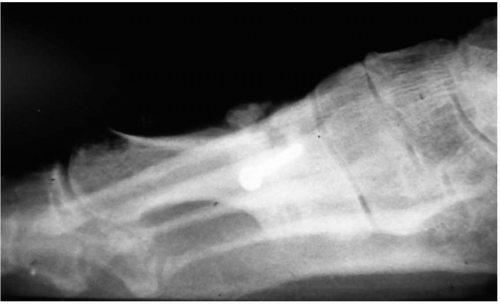
 FIG. 9. Osteochondritis dissecans of the first metatarsal head occurs on the dorsal one-third of the articular surface, centrally from medial to lateral. |
Hallux Equinus Versus Metatarsus Primus Elevatus
Controversy exists regarding the order of events in the progression of hallux limitus to hallux rigidus. Elevation of the medial column may be either primary or secondary to the influence of the hallux. Hallux equinus can occur primarily, or it may be secondary to a forefoot or rearfoot varus deformity. With an uncompensated varus, metatarsus primus elevatus is present initially, and hallux equinus occurs as a compensation (2). In the hypermobile flatfoot or spastic deformities, the hallux equinus occurs first (9), and it secondarily elevates the first metatarsal in the sagittal plane (32). Clinical and radiologic examinations help to determine whether the hallux equinus or metatarsus primus elevatus is the primary deformity.
Observation of stance and gait at times demonstrate the compensatory muscular contraction of the hallux in midstance and propulsion. Range of motion of the subtalar, midtarsal, and tarsometatarsal joints reveals the level of hypermobility or joint immobility, as well as each joint’s neutral position. Manual loading of the forefoot through the first and fifth metatarsophalangeal joints pronates the rearfoot and allows for observation of the sagittal position of the first ray in relation to the lesser metatarsus. In a patient with a forefoot varus deformity, one will not be able to plantarflex the first ray to a plane that is parallel to the fifth metatarsal. A forefoot supinatus deformity is characterized by the ability of the first ray to plantarflex, but only through rearfoot pronation.
Another clinical method of assessing metatarsus primus elevatus is through use of a forefoot block test (27). In this test, the patient bears weight while the digits are suspended off the weight-bearing surface. A step, book, or other platform serves to allow the patient’s entire foot to bear weight from the heel to the metatarsal heads, without the digits’ contacting the ground. The influence of the hallux on metatarsus primus elevatus is thus eliminated as the rearfoot and forefoot pronate and allow the first ray to gain contact with the ground. If no difference in the sagittal position of the first metatarsal occurs when comparing normal weight bearing with the forefoot block test, then the foot either has a varus deformity or the forefoot is being maintained in an inverted position because of a long-standing contracture of the tibialis anterior tendon. If the tendon is in spasm, the foot may resist pronation initially, but the spasm can be broken by volitional contraction of the peroneus longus tendon.
Radiologic Examination
Standard pedal radiographic examination is used to help assess the type and severity of hallux limitus and hallux rigidus. Hallux limitus or rigidus may appear radiographically similar to osteoarthritis or traumatic arthritis in other joints, depending on the severity and stage of the process. However, specific findings are unique to the first metatarsophalangeal joint. Nonspecific findings include joint space narrowing, osteophytic lipping, joint flattening, joint enlargement, sclerosis of the subchondral bone plate, subchondral cyst formation, and intraarticular fragmentation (e.g., loose bodies, joint mice). Findings specific to the first metatarsophalangeal joint include the following: accentuation of the sesamoidal grooves on the dorsoplantar radiograph, actually a cupping of the metatarsal head around the base of the proximal phalanx; lateral and dorsal spurring; metatarsalsesamoid arthrosis; sesamoid hypertrophy and elongation; and proximal sesamoid migration (27).
Classification systems for the radiographic findings have been described as a means to characterize the degree of deformity. Although differences of opinion exist regarding treatment for each stage, the general consensus is that advanced degenerative disease correlates with less satisfactory surgical outcomes regardless of the surgical procedure or grading system that was used to assess the condition of the joint (46, 47, 48, 49).
Grading scales have been proposed to characterize the severity of deformity based on radiographic findings. Osteoarthritis may be graded as follows (50):
Grade I: Small osteophytes
Grade II: Definite osteophytes in the presence of an unimpaired joint space.
Grade III: Extensive loss of joint space in the presence of sclerosis of subchondral bone.
Within the first metatarsophalangeal joint, Regnauld described the following (13):
Grade I: Functional limitation of dorsiflexion, mild dorsal spurring, pain derived from dorsal hypertrophy, no structural sesamoid disease.
Grade II: Broadening and flattening of metatarsal head and base of proximal phalanx, joint space narrowing, structural first ray elevatus, osteochondral defect, sesamoid hypertrophy.
Grade III: Severe loss of joint space, extensive dorsal, medial, and lateral spurring, osteochondral defects of metatarsal head and/or proximal phalanx, with or without joint mice, extensive sesamoid hypertrophy and loss of joint space, near ankylosis.
Hanft et al. further characterized these findings, with subcategories to include osteochondral defects and subchondral cysts (47):
Grade I: Metatarsus primus elevatus, mild dorsal spurring, and sclerosis.
Grade II: Elements of grade I, plus broadening and flattening of the joint, decreased joint space, dorsal and lateral osteophytes.
Grade IIB: Elements of grade II, plus osteochondral defect, loose bodies, and subchondral cyst formation.
Grade III: Elements of grade II, plus severe flattening of the joint, sesamoid hypertrophy, minimal joint space, severe dorsal and lateral spurring, and osteophyte formation.
Grade IIIB: Elements of grade III, plus osteochondral defects, loose bodies, and subchondral cyst formation.
Sesamoid degeneration and elongation indicate sesamoid immobility and likewise correlate to the degree of arthrosis of the metatarsophalangeal joint. Chronic traction and tension on the sesamoid apparatus from adaptive contracture of the intrinsic muscles may lead to bony proliferation at the proximal and distal margins of the sesamoids (13,42), much like that of insertional enthesiopathies seen elsewhere in the lower extremity (inferior and posterior calcaneal spur) (Fig. 11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree