Chapter 18 Great-Toe Disorders
Introduction
Clanton and Ford1 found that foot injuries rank third behind ankle and knee injuries as the most common time-loss injury among university athletes. Of these foot injuries, a large proportion were sprains of the forefoot and, more specifically, the hallux MTP joint. In our practice, we have seen a number of professional athletes with a broad range of injuries to the great toe and base this chapter on our experiences.
Anatomy
To the surgeon responsible for the care of athletes with great-toe injuries, knowledge of the anatomy of the hallux MTP joint is paramount. In the simplest of terms, the motion of the joint consists of rolling, sliding, and compression. More specifically, the morphology of this joint allows for plantarflexion and dorsiflexion but very limited abduction and adduction. The fact that there is more than one center of motion contradicts the theory of a simple, hinged joint. Instead, the joint is a dynamic acetabulum or “hammock,” as described by Kelikian.2 The joint articulation provides little of the overall stability because of the shallow, glenoid-like cavity of the proximal phalanx. Most of the stability comes instead from the capsular-ligamentous-sesamoid complex, which is described in detail later.
There are two sets of ligaments that contribute to the stability of the metatarsal (MT) head as it articulates with the proximal phalanx: the medial and lateral collateral ligaments and the metatarsosesamoid suspensory ligaments.3 The fan-shaped medial collateral ligament is composed of the medial MTP ligament and the medial metatarsosesamoid ligament (Fig. 18-1). The lateral collateral ligament is structured in a similar fashion.3
Figure 18-1 Medial diagrammatic representation of first metatarsophalangeal joint.
From Adelaar RS, editor: Disorders of the great toe, Rosemont, IL, 1997, American Academy of Orthopaedic Surgeons.
In addition to the collateral ligaments, the strong, fibrous plantar plate (see Fig. 18-1) also affords structural support. The capsular ligamentous complex of the hallux MTP joint actually is a confluence of structures including the plantar plate, collateral ligaments, the flexor hallucis brevis, the adductor hallucis, and abductor hallucis tendons. This plantar plate is attached firmly to the base of the proximal phalanx and only loosely attached at the MT neck through the capsule.4
The split tendon of the flexor hallucis brevis runs along the plantar aspect of the hallux and envelops the sesamoids before inserting at the base of the proximal phalanx as the capsular-ligamentous complex (see Fig. 18-1). The two sesamoids are united by a thick, intersesamoid ligament and maintain the course of the FHL tendon. Adding to the stability of the hallux MTP joint are three other intrinsic muscles of the great toe. The extensor hallucis brevis originates at the fascia overlying the sinus tarsi and runs obliquely to attach into the extensor mechanism on the dorsum of the MTP joint. It functions primarily as an extensor of the hallux MTP joint. On the plantar aspect, the abductor and adductor hallucis tendons insert on the medial and lateral aspects of the hallux MTP joint, respectively. These tendons blend into the capsular-ligamentous complex, as well as the sesamoids, to provide additional structural support (Fig. 18-2).5
Biomechanics
The hallux MTP joint lies in an intricate balance of opposing tendons and ligaments. The anatomy outlined previously, especially with regard to the plantar plate, is important when considering the biomechanical demands placed on the first MTP joint. During normal gait, the great toe typically supports twice the load of the lesser toes and accommodates forces reaching 40% to 60% of body weight.6 During athletic activity, including jogging and running, the peak forces may approach two to three times body weight, and the forces increase to eightfold when a running jump is performed.7
The range of motion (ROM) in the normal foot has been studied extensively; it is noted to be highly variable and to decrease with aging. In the resting position, the first MTP joint is in a mean resting position of 16 degrees of dorsiflexion. The passive arc of motion was noted by Joseph to be from 3 to 43 degrees of plantarflexion and from 40 to 100 degrees of dorsiflexion.8 The mean passive MTP joint dorsiflexion during push-off was 84 degrees. One study found that at least 60 degrees of dorsiflexion is considered normal in barefoot walking on a level surface.9 Athletes may accommodate up to 50% reduction in MTP joint motion resulting from acute injury to the plantar plate or hallux rigidus by various gait adjustments such as foot/leg external rotation, shortened stride, and increased ankle, knee, or hip motion.4 In addition, a stiff-soled shoe is capable of decreasing MTP joint dorsiflexion to 25 to 30 degrees without significantly affecting gait.9
The effects on the push-off power of the great toe following sesamoidectomy have been studied in vitro by Aper et al.10 They confirmed the importance of this seemingly insignificant bone to the function of the toe, particularly in the athlete, in whom even a small loss of power will affect overall performance. The study noted that the isolated excision of the tibial sesamoid equated to an 11% loss of flexor power, there was 19% loss for a fibular sesamoidectomy, and 32% when both are excised.10
Specific Entities of the Great Toe
Hallux rigidus
Hallux rigidus is defined as a localized degeneration of the hallux MTP joint. It was first described as hallux flexus in 1887 by Davies-Colley.11 In his first description of this condition, he discussed a plantarflexed posture of phalanx relative to MT head. The actual term “hallux rigidus” was coined by Cotterill in 1888 and remains the most common term used today.12 Numerous papers have theorized the etiology and pathophysiology of hallux rigidus. One such theory is that of metatarsus elevatus, a term describing the dorsiflexed posture of the first ray in relationship to the foot and the subsequent plantarflexed posture of the hallux. This has been discussed by many authors, but the most current data indicate that the elevated posture of the first MT improves after dorsal decompression of the hallux MTP joint.13–16 Overuse and repetitive dorsiflexion forces, such as those occurring in a runner or kicker, may lead to chondral lesions and other occult injuries17 or to osteochondritis dissecans.2,18,19 It also may result as a sequelae to a turf-toe injury. Anatomic abnormalities that may lead to hallux rigidus include the flat or pronated foot,15,20,21 a long first MT or hallux,21 and a flat MT head.22 To this time the true potential etiologies for the development of hallux rigidus remain in question.
Clinical grading from mild to severe (or I, II, and III) has been proposed by many authors. Grading depends on the severity of disease and is based on ROM, pain or crepitus with motion, the size of the dorsal osteophyte on the MT head, the presence of sesamoid involvement, and the radiographic alignment of the hallux (on anterior-posterior [AP] and lateral views). A radiographic classification scheme was created by Hattrup and Johnson in 1988.23 Their grade 1 is considered mild; the joint space is maintained and there is minimal spurring. Grade 2 is moderate disease in which the joint space is narrow, bony proliferation is present on the MT head and phalanx, and there is subchondral sclerosis and/or cyst formation. Grade 3 is the severe type, with significant joint space narrowing and extensive bony proliferation that involves the entire periphery and includes loose bodies, a dorsal ossicle, or subchondral cyst formation. A more recent grading scheme, proposed by Coughlin and Shurnas,24 combines objective and subjective clinical data with radiographic findings (Grades 0 to 4). Treatment recommendations are made on the basis of grade severity.
Nonoperative treatment options include the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and shoewear modifications. Shoes of adequate size and a more full-fitted toe box or increased depth are helpful and can be modified further with a balloon patch over bony prominences. Turf-toe inserts (Springlite, Otto Bock, Minneapolis, MN) that limit dorsiflexion and subsequent dorsal impingement are potentially useful but may limit performance in the elite runner. Rigid rocker soles function in the same manner as semirigid inserts and, although helpful in the general population, are not popular with the athlete because of the increased weight and excessive stiffness. Orthotic devices can unload the hallux MTP joint, but one must remember to increase the shoe size to accommodate for it. Taping techniques can limit dorsiflexion and provide pain relief. Application is the same as that for turf-toe; however, skin problems such as blistering can occur. Steroid injections must be given judiciously and perhaps only for “big game” situations. Repeated injections may accelerate the degenerative process.25
The technique has been described and popularized by Mann and Clanton.26 Their preference is a dorsal longitudinal incision centered over the hallux MTP joint. The joint capsule is incised on either side of the extensor hallucis longus (EHL) tendon and a complete synovectomy is performed. The joint is plantarflexed to permit inspection of the sesamoid articulation. Hamilton27 recommends mobilizing the sesamoids by blunt dissection, for they often are anchored by adhesions and limit dorsiflexion even after removal of impinging osteophytes. The amount of bone to be removed from the MT head is dictated by the size of the dorsal exostosis and the degree of articular cartilage destruction. If degeneration of articular cartilage is not significant and the main problem is the dorsal exostosis, then 20% to 30% of the dorsal aspect of the MT head is removed along with the exostosis (see Fig. 18-2).
We have modified the cheilectomy technique through a medial approach. This allows for plantar debridement and release of plantar capsule and adhesions, thus improving dorsiflexion. In addition, the incision avoids the EHL tendon and the potential for tenodesis secondary to scar formation while still providing access to lateral osteophytes. We recommend a two-cut technique to avoid excessive resection of the MT head (Fig. 18-3). The first cut of the saw includes the dorsal exostosis and is made flush with the dorsal diaphysis. The subsequent cut removes the amount of articular surface necessary to achieve the desired dorsiflexion while eliminating the risk of excessive head removal that may jeopardize later arthrodesis.
Hamilton27 describes “radical cheilectomy” similar to the cheilectomy of Mann but also removing the dorsal portion of the base of the proximal phalanx, matching the resection performed on the MT head. This modification serves as an option for dancers with end-stage disease and is similar to the Valenti28,29 procedure described later in this chapter.
A number of authors have provided their results of cheilectomy. Mann and Clanton26 found that 22 of 31 patients had complete relief, 6 of 31 achieved considerable relief, and ROM increased an average of 20 degrees in 23 of 31 feet. Hattrup and Johnson30 reported that 53.4% were satisfactory and 27.6% unsatisfactory. Their failure rate increased from 15% with grade I radiographic changes to 37.5% with grade III changes. They concluded that cheilectomy is the procedure of choice in patients with hallux rigidus and grade I changes. Graves’31 experience showed little improvement in motion and stated that satisfaction with cheilectomy was more likely if the patient and the physician had reasonable expectations regarding outcome. He recommended careful patient selection. Myerson agreed that the procedure improves pain, not motion. Easley et al.32 reported on 57 patients (75 feet) with greater than 3-year follow-up (average 63 months). Their cheilectomy was performed via a medial approach by a single surgeon. American Orthopaedic Foot and Ankle Society (AOFAS) scores were 45 preoperative, 85 postoperative, and 90% satisfied. The average dorsiflexion improved from 19 degrees preoperative to 39 degrees postoperative. The majority of patients had worsening of radiographic arthritis, but this did not correlate with symptoms. Three patients eventually required an arthrodesis.
Phalangeal osteotomy has been advocated as a useful surgical adjuvant to a cheilectomy. This technique was first proposed by Bonney and Macnab in 1952.13 Kessel and Bonney19 described its use in 10 adolescents in 1958. Moberg is the name most commonly associated with the procedure, after his case series reported in 1979.33 The procedure involves a dorsal closing wedge osteotomy of the proximal third of the proximal phalanx. It relies on the principle that the arc of motion of the hallux MTP joint is translated to plantar aspect of head, thereby increasing functional motion. Basically it creates pseudodorsiflexion, which in turn places less stress on the hallux with push-off. Adequate plantarflexion of the joint is a prerequisite. Thomas and Smith34 also found that the procedure appeared to provide dorsal joint space decompression, as well, further relieving stress from the arthritic joint (Fig. 18-4).

Figure 18-4 Space created by dorsiflexion osteotomy of the proximal phalanx.
From Thomas PJ, Smith RWL: Foot Ankle Int 20:4, 1999.
The indications for performing a Moberg osteotomy on the proximal phalanx includes grade I or II hallux rigidus, adolescent hallux rigidus, and the running athlete, perhaps regardless of grade. Most authors now recommend combining the procedure with a dorsal cheilectomy.32,34,35
The technique can be performed through a medial or dorsal incision, extending distally from the incision used for the cheilectomy of the hallux MTP joint. It is important to protect the dorsomedial and plantar medial cutaneous nerves to limit paresthesia and the potential for neuritis or neuroma. Longitudinal reflection of soft tissues at the proximal third of the phalanx is performed, maintaining capsular insertion. The FHL and EHL tendons are protected as a dorsal closing wedge osteotomy is performed with a microsagittal saw approximately 3 to 5 mm distal to the MTP joint. In the adolescent, it is necessary to avoid the physis. Intraoperative fluoroscopy can be useful in confirming proper position of the osteotomy. The plantar cortex is maintained to allow for a “greenstick” effect with manual closure of the osteotomy. Generally 2 to 6 mm of dorsal cortex should be removed, with the actual amount determined by the degree of joint stiffness and amount of plantarflexion of the hallux available. The goal is to obtain 20 to 30 degrees of dorsiflexion relative to the first MT axis. The osteotomy should be stabilized with a suture, K-wire, screw, or staple. If combined with a cheilectomy, stable, internal fixation is mandatory to allow for the initiation of early motion (Fig. 18-5, A and B).
Published results of the proximal phalanx osteotomy include Moberg’s review of older individuals at short follow-up. Eight patients were noted to have satisfactory results. Citron and Neil36 evaluated 10 feet in 8 patients with 22-year follow-up (minimum 10 years) and identified 5 symptom free, others with progression of degenerative joint disease (DJD), and one requiring arthrodesis. The average postoperative motion was 43 degrees, 22 degrees being dorsiflexion, with late loss of plantarflexion noted. Asymptomatic compensatory hallux IP flexion contracture often was present. They felt that this osteotomy represented an especially good option in the adolescent. Thomas and Smith34 performed the osteotomy with a dorsal cheilectomy in 27 feet, 20 patients. At a follow-up average of 5.2 years, there was a 100% union rate, the average dorsiflexion increased 7 degrees, and 96% of patients were satisfied or satisfied with reservation.
Resection arthroplasty, like that of a Keller, is reserved for the older individual. Capsular interposition is a modification of this procedure devised by Hamilton.37,38 In this procedure the proximal 5 to 10 mm of proximal phalanx is resected, followed by transection of the extensor hallucis brevis (EHB) tendon and dorsal capsule. This dorsal soft-tissue complex then is advanced to the plantar complex. Some authors release the flexor hallucis brevis (FHB) tendon from the base of the phalanx and suture this to the dorsal capsule. Temporary pin fixation is not necessary (Fig. 18-6, A and B). Our own experience with the procedure has noted good relief of pain from dorsal impingement and joint degeneration but a concerning loss of push-off strength. Similarly, the Valenti28,29 procedure is a salvage technique in which an angled resection on both sides of the joint is performed, preserving the plantar complex and overall length. The result is a “hinge” effect at the level of the joint (Fig. 18-7).
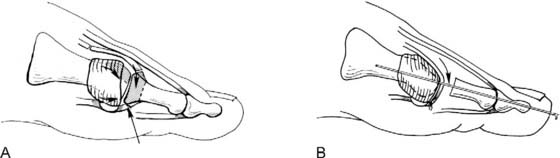
Figure 18-6 (A) Interposition arthroplasty as described by Hamilton. (B) Pin fixation is not necessary.
From Hamilton WG, Hubbard CE: Foot Ankle Clin 5:663, 2000.

Figure 18-7 Resection of the dorsal metatarsal head as well as dorsal proximal phalanx.
From Coughlin MJ, Mann RA, editors: Surgery of the foot and ankle, ed 7, St Louis, 1999, Mosby-Year Book.
Most recently, an “anchovy” interposition of the hallux MTP joint has been performed in those individuals failing a cheilectomy but needing to maintain hallux MTP motion. Conical resection on both sides of the joint is followed by insertion of a semitendinosus allograft rolled into an “anchovy.” We have used this technique on three patients, one a professional football player, with good short-term results. Coughlin and Shurnas39 recently reported on their experience with this technique in seven patients with excellent results. This case series demonstrates that this is a good surgical option in patients who otherwise would be treated with MTP arthrodesis.
Arthroscopic intervention for disorders of the hallux MTP joint has received some attention over recent years. It has been shown to be more of a diagnostic modality than a therapeutic one but may be a reasonable option for the removal of small dorsal osteophytes or loose bodies. It also may be used for debridement of an osteochondral defect on the MT head but is not indicated in advanced hallux rigidus. Van Dijk et al.40 performed a prospective study with 24 athletes and found that it was not favorable for hallux rigidus because of “scar fibrosis.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree