Chapter 49 General Principles of Arthroscopy
Instruments and Equipment
Arthroscope
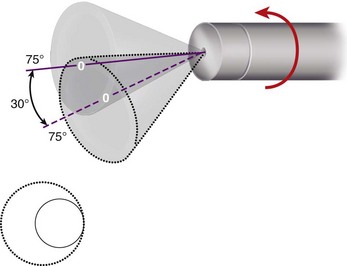
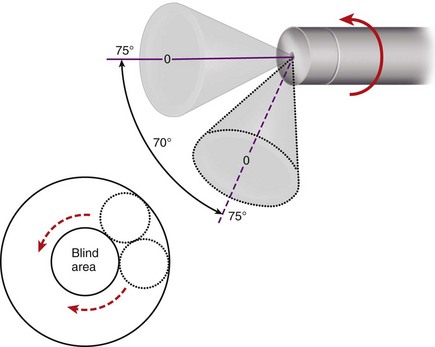
Field of view refers to the viewing angle encompassed by the lens and varies according to the type of arthroscope. The 1.9-mm scope has a 65-degree field of view; the 2.7-mm scope, a 90-degree field of view; and the 4.0-mm scope, a 115-degree field of view. Wider viewing angles make orientation by the observer much easier. Rotation of the forward oblique viewing (25- and 30-degree) arthroscopes allows a much larger area of the joint to be observed (Fig. 49-1). Rotation of 70-degree arthroscopes produces an extremely large field of view but may create a central blind area directly in front of the scope (Fig. 49-2).
Accessory Instruments
Many new instruments have been redesigned for use in advanced shoulder procedures. Instruments to pass, retrieve, and tie sutures have greatly advanced soft tissue repair procedures of the capsule, labrum, and rotator cuff (Fig. 49-3).
Probe
The probe is perhaps the most used and important diagnostic instrument after the arthroscope. The probe has become known over the years as “the extension of the arthroscopist’s finger.” It is used in both diagnostic and operative arthroscopy and is the safest instrument that one can use in learning triangulation techniques (Fig. 49-4). The probe is essential for palpating intraarticular structures and in planning the approach to a surgical procedure. A tactile sensation soon develops regarding what is normal and what is abnormal. It is better to “see and feel” rather than to just “see” alone. The probe can be used to feel the consistency of a structure, such as the articular cartilage; to determine the depth of chondromalacic areas; to identify and palpate loose structures within the joint, such as tears of the menisci; to maneuver loose bodies into more accessible grasping positions; to palpate the anterior cruciate ligament and determine the tension in the ligamentous and synovial structures within the joint; to retract structures within the joint for exposure; to elevate a meniscus so that its undersurface can be viewed; and to probe the fossae and recesses, such as the popliteal hiatus within the joint. Most probes are right angled with a tip size of 3 to 4 mm, and this known size of the hook can be used to measure the size of intraarticular lesions. Magnification occurs with the arthroscope, and the closer the arthroscope, the greater the magnification. Care should be taken in using the tip of the probe, and much of the palpation with the probe within the joint is actually done with the elbow of the probe rather than the tip or toe of the instrument.
Scissors
Arthroscopic scissors are 3 to 4 mm in diameter and are available in both small and large sizes. The jaws of the scissors may be straight or hooked (Fig. 49-5). The hooked scissors are preferred because the configuration of the jaws tends to hook the tissue and pull it between the cutting edges of the scissors, rather than pushing the material away from the jaws, which can occur with the straight scissors. Optional accessory scissors designs include right and left curved scissors and angled cutting scissors. The difference between these two designs is based on the location of the angulation. The shank of the curved scissors is gently curved to accommodate right and left positioning, whereas the angled scissors, usually with a rotating type of jaw mechanism, actually cut at an angle to the shaft of the scissors. These accessory designs are useful in detaching difficult-to-reach meniscal fragments.
Basket Forceps
The basket or punch biopsy forceps is one of the most commonly used operative arthroscopic instruments (see Fig. 49-5). The standard basket forceps has an open base that permits each punch or bite of tissue to drop free within the joint and does not require the instrument to be removed from the joint and cleaned with each bite. Small fragments of tissue that drop free within the joint through the open-floor punch or basket forceps can be irrigated out or subsequently removed from the joint by suction. This instrument is available in 3- to 5-mm sizes with a straight or curved shaft. It is useful in trimming the peripheral rim of the meniscus, or it can be used instead of scissors to cut across meniscal or other tissue. Wide, low-profile baskets are excellent for meniscal work. The configuration of the jaws of the basket forceps may be straight or hooked; again, the hooked configuration is preferred. Baskets are available in an assortment of angles, including 30, 45, and 90 degrees, which are especially useful for trimming the anterior portions of the meniscus. They also are available in 15-degree down-biting and 15-degree up-biting curves to make it easier to get around the femoral condyle during resection of the posterior meniscal horn. As with other arthroscopic instruments, the proper technique is to make small bites to avoid excessive pressure on the joints and pins of the instrument and to prevent frequent breakage.
Grasping Forceps
Grasping forceps (see Fig. 49-5) are useful to retrieve material from the joint, such as loose bodies or synovium, or to place meniscal flaps and other tissues under tension while cutting with a second instrument. Most grasping forceps have some type of ratchet closure on the handle to secure the tissue within the jaws. The jaws of the grasping forceps may be of single- or double-action design and may have regular serrated interdigitating teeth or one or two sharp teeth to better secure the grasped tissue. The double-action grasping forceps, both jaws of which open, are especially preferred for securing an osteocartilaginous loose body because the single-action types frequently allow it to slip from between the jaws.
Motorized Shaving Systems
The motorized shaving systems are all basically of similar design, consisting of an outer, hollow sheath and an inner, hollow rotating cannula with corresponding windows (Fig. 49-6). The window of the inner sheath functions as a two-edged, cylindrical blade that spins within the outer hollow tube. Suction through the cylinder brings the fragments of soft tissue into the window, and as the blade rotates, the fragments are amputated, sucked to the outside, and collected in a suction trap. Numerous cutting tips have been developed for specific situations and functions. The diameter of the cutting tip usually is 3 to 5.5 mm, and many of the tips have variable sizes to allow access to smaller or tighter joints. Special blades have been designed for meniscal cutting or trimming, for synovial resection, and for shaving of articular cartilage. Special burrs and abraders have been designed for arthroscopic acromioplasty and anterior cruciate ligament reconstructions. Most systems use a foot pedal to control the motor and allow for variable speed and direction. Reversing the rotation of the cutting blade intermittently often improves cutting efficiency and minimizes clogging with debris. Motorized shavers have been developed for small joints with a 2-mm shaver and burr.
Implants
Meniscal repair devices, of varying designs and materials, allow an all-inside meniscal repair without the need for arthroscopic knot-tying, accessory portals, or incisions. The first generation meniscal repair devices were solid flexible devices placed across the tear to hold the meniscal fragments in place. Today’s fourth-generation devices are low profile, have a suture tension construct, and provide much greater fixation strength. The techniques for use of specific meniscal repair devices are discussed in Chapters 45 and 51.
Miscellaneous Equipment
As arthroscopic surgery procedures have advanced to more joints, additional instruments have been developed. “Switching sticks” are simple rods placed through the cannula to maintain the portal while the cannula is exchanged. A dilator is used prior to exchange for a larger operating cannula. The Wissinger rod was designed to assist in establishing a portal on the opposite side of a joint from a previously established portal. Traction devices have been developed for use in the shoulder, elbow, and ankle for better exposure (see Chapters 50 and 52). There also has been an explosion of procedure-specific instruments, many of which are described in the pertinent operative sections in Chapters 50 to 52.
Irrigation Systems
Usually, two 5-L plastic bags of lactated Ringer solution, interconnected with a Y-connector, are suspended for use with the arthroscopic pump (Fig. 49-7). Once the inflow and outflow cannulas are established, the joint is lavaged until the fluid is clear. When a pump is not used, joint distention is increased by elevating the fluid bag, using a large-diameter tubing, or decreasing the size and number of outflow portals. For each foot of elevation of the solution bag above the level of the joint, 22 mm Hg of pressure is produced. The bag usually is placed 3 to 4 feet above the level of the joint, thus producing approximately 66 to 88 mm Hg of pressure. Arthroscopic pumps should be used carefully, and the tightness of muscle compartments and soft tissue spaces, such as the popliteal fossa, should be monitored closely. Pump pressures should be varied according to the joint being treated and the type of pump being used. When a pressure inflow system is used, joint distention pressures in the knee generally should be 60 to 80 mm Hg. Vision and hemostasis in the shoulder usually are best when the distention pressure is maintained approximately 30 mm Hg below the systolic blood pressure. In healthy patients, hypotensive anesthesia may be used to reduce systolic pressure to approximately 100 mm Hg, at which level pump pressure of 70 to 80 mm Hg usually provides safe distention and clear vision. Olszewski et al., in a prospective, double-blinded, randomized study, found that the addition of epinephrine (1 mg per liter of saline) significantly increased visibility and reduced the need for tourniquet inflation by 50% compared with the placebo group of patients who had not received epinephrine. In patients with hypertension or cardiac problems, we forgo the use of epinephrine. Karaoglu et al. also found that adding a small amount of epinephrine (50 mg/10 mL) to the local anesthetic mixture just before portal site injection improved arthroscopic viewing.