Common
Gastritis (erosive due to NSAIDs)
Esophagitis
Peptic ulcer disease
Esophagogastric varices with or without portal hypertensive gastropathy
Gastroesophageal mucosal tears
Cancer (carcinoma, lymphoma, polyps)
Dieulafoy lesions (active arterial bleeding or an adherent clot on an underlying vessel in the absence of an ulcer)
Rare
Infections (CMV, herpes, Candida)
GERD
Aortoenteric fistula
Blood dyscrasia
Vasculitis
Hemorrhagic telangiectasia
Pancreatic cancer
Uremia
• Other causes. Blood dyscrasias, vasculitis, connective tissue diseases (CTDs), and hereditary hemorrhagic telangiectasia (Osler–Rendu–Weber disease) may rarely be the cause of UGI bleeding. Hematobilia occurs secondary to trauma, injury, or vascular malformations of the liver or biliary tree. Aortoduodenal fistulas and large ectatic submucosal arteries (Dieulafoy lesion) or arteriovenous malformation (AVMs) may cause massive hemorrhage. Gastroesophageal reflux disease (GERD), cancer, and infections such as cytomegalovirus (CMV), herpes, or Candida may cause UGI bleeding but more usually cause chronic blood loss. Rarely, large hiatal hernias may cause blood loss as a result of linear mucosal tears. Even more rarely, gastric cancer, lymphoma, polyps, and other tumors of the stomach or small intestine may cause UGI bleeding.
DIAGNOSIS
Clinical Presentation
Clinical presentation depends on the location, source, and acuity of the bleed.2
• Acute UGI bleeding often presents with bloody vomiting. Blood from a recent bleed is usually bright red. Bleeding from varices is usually abrupt and massive. Melena (black, tarry, malodorous stools) usually is the result of UGI bleeding or lesions of the small intestine if GI transit time is prolonged. Melena can be seen with variable degrees of blood loss, being seen with as little as 50 mL of blood. Hematochezia (maroon or bright red blood per rectum can be the presenting symptom in a small proportion of cases of UGI bleeding. A history of alcohol abuse, cigarette smoking, or NSAID use may often exist. In these cases, bleeding is typically brisk and may be accompanied by hemodynamic instability.
• Chronic or unrecognized UGI bleeding may present with pallor, dizziness, dyspnea, iron deficiency anemia, or occult blood in stool.
• Physiologic responses to UGI bleeding
• In acute UGI bleeding, the physiologic response depends on the rate and extent of hemorrhage.
Blood loss less than 500 mL is usually asymptomatic, except in elderly patients with coronary artery or chronic lung disease.
• Rapid blood loss results in decreased cardiac output reflex, and orthostatic hypotension indicating a reduction in blood volume of more than 20%. Lightheadedness, confusion, nausea, sweating, fainting, and thirst are commonly associated with symptoms.
• When blood loss approaches 40% of blood volume, shock occurs, with tachycardia, hypotension, pallor, and cold clammy extremities.
• Initial hemoglobin levels do not give a useful estimate of the volume of hemorrhage in the acute setting, and levels may be normal despite significant blood loss.
• Chronic blood loss may be asymptomatic or present with signs and symptoms of anemia, hyponatremia, and hypoalbuminemia as a result of retention of hypotonic fluid to replenish intravascular volume.
History and Physical Examination
These identify the cause in only 50% of cases.
• Prior history of PUD or dyspepsia may suggest ulcer bleeding. A history of medication (NSAIDS, clopidogrel, and anticoagulants) and alcohol use should be elicited. Symptoms of cirrhosis may suggest variceal bleeding. Bleeding from other sources (e.g., frequent nosebleeds, bruising) may suggest a coagulopathy. Patients with renal disease, aortic stenosis, and hereditary hemorrhagic telangiectasia are more likely to have angiodysplasia. Odynophagia, dysphagia, or gastric reflux may occur in patients with esophageal ulcer. Retching or violent coughing may occur prior to bleeding in patients with Mallory–Weiss tears.3
• Examination. Epigastric tenderness is suggestive of PUD. Hepatosplenomegaly may occur in liver disease or malignancy. A rectal examination may reveal melena, but stool may be normal in patients with minimal or recent bleeding.
• Laboratory studies. If blood loss is rapid, the hematocrit may not reflect the magnitude of loss because equilibration with hemodilution requires 8 hours. Initial laboratory tests should include a complete blood count, serum chemistries, liver tests, and coagulation studies. The blood urea nitrogen may be elevated due to blood protein breakdown to urea by intestinal bacteria and reduced glomerular filtration rate. A ratio of blood urea nitrogen to serum creatinine of greater than 20 is predictive of a bleed coming from an upper GI source.
TREATMENT
Always begins with resuscitation, restoration of intravascular volume, correction of hemoglobin loss, and treatment of pathophysiologic changes.
• Resuscitation. Vital signs should be monitored frequently and fluid replaced rapidly. Intravenous access using two wide-bore cannulae should be gained. Crystalloids (normal saline or Ringer solution) or fresh frozen plasma (especially in patients with coagulopathy) should be used until blood is available. Military antishock trousers may be required to correct shock. For unstable cardiac patients, central venous or pulmonary wedge pressures should be measured, with a goal of keeping blood pressure and pulse stable and maintaining urinary output at more than 40 mL per hour. Blood transfusions should be initiated if hemoglobin is <7 g per dL with a goal of maintaining a level of ≥9 g per dL. Blood replacement is especially important in elderly patients and those intolerant of hypoxia (coronary artery disease, pulmonary disease). Intravenous proton pump inhibitor therapy may reduce the risk for rebleeding when endoscopy is also performed. Transfusing patients with suspected variceal bleeding to hemoglobin >10 g per dL should be avoided as it can precipitate worsening of the bleeding.
• Gastric lavage through a nasogastric (NG) tube can localize bleeding proximal to the ligament of Treitz. NG suction removes gastric fluid, blood, and swallowed air and can control nausea and vomiting. It is helpful when patients are suspected to have ongoing bleeding and who may benefit from early endoscopy. It has, however, been shown to be ineffective in achieving hemostasis and is no longer recommended as a first-line intervention. The presence of blood or “coffee-grounds” on NG aspiration confirms an UGI source, whereas a clear aspirate reduces the likelihood of an UGI source. If endoscopy is to be scheduled in the next several hours, then NG placement is not necessary.
Specific Therapeutic Interventions
Peptic Ulcer Bleeding
• Medications: Antacids should be with pantoprazole or omeprazole. Prokinetics such as erythromycin or metoclopramide are effective in facilitating gastric emptying, allowing better visualization at endoscopy. If H. pylori infection is diagnosed, treatment with regimens that include a protein pump inhibitor/bismuth, amoxicillin/clarithromycin/tetracycline, and metronidazole are usually effective (see Chapter 11.1).4
• Endoscopy is the diagnostic modality of choice for acute upper GI bleeding and once a bleeding lesion has been identified, therapeutic interventions under direct visualization can achieve hemostasis and prevent recurrent bleeding in most patients. Risks of endoscopy include aspiration, adverse reaction to conscious sedation, perforation, and causing bleeding.
• Laser photocoagulation and electrocautery under direct endoscopic visualization may rapidly control active ulcer bleeding.
• Infusion of epinephrine in quadrants around the bleeding point and then into the bleeding vessel achieves hemostasis in 95% of cases (if endoscopic hemostasis fails). Fibrin glue and human thrombin may be the most effective injection materials.
• Mechanical devices “endoclips” may be an option for major bleeding ulcers, especially for arterial tears.
• Surgery is indicated if hemorrhage is brisk or sustained for longer than 6 to 12 hours, or if shock is not controlled by resuscitation. Patients with rapidly bleeding or recurring gastric ulcers may be surgical candidates. Surgery usually involves underrunning the ulcer and pyloroplasty.
Gastritis and Gastric Erosions
Antacids and H2 receptor blockers reduce the incidence of hemorrhage from stress ulcers. Misoprostol is effective in preventing gastritis due to NSAIDs. Sucralfate and proton pump inhibitors are also effective for patients with prior UGI bleeding who require continued NSAIDs. Laser and electrocautery under direct visualization may control persistent bleeding.
Variceal Bleeding
Only 50% of patients with variceal hemorrhage stop bleeding spontaneously; however, following cessation of acute bleeding, there is a high risk of recurrent hemorrhage.5 Variceal bleeding may be completely controlled by endoscopic injection of a sclerosing agent, thrombin, epinephrine, or other agents. Noninvasive pharmacologic treatment aimed at causing splanchnic vasoconstriction and thus reducing portal pressure (vasopressin, somatostatin, propranolol). In patients with suspected variceal bleeding, octreotide is given by intravenous bolus of 20 to 50 mcg, followed by continuous infusion at rate of 25 to 50 mcg per hour. Thermal modalities or mechanical (banding, sewing, hemoclips, and endoloop) techniques often effectively control bleeding. Acute bleeding may be abated by balloon occlusion with a Sengstaken–Blakemore tube followed by definitive therapy within 48 hours. Antibiotic prophylaxis with intravenous ciprofloxacin or cephalexin should be instituted in any patient with cirrhosis and GI hemorrhage. Recurrent bleeding may be prevented by periodic endoscopic sclerotherapy. Propranolol given twice daily (at a dose that reduces the heart rate by 25%) decreases portal pressure, although the response is nonuniform.
Arteriovenous Malformations
When actively bleeding, AVMs are best treated with electrocautery. Mallory–Weiss tears usually stop bleeding spontaneously but may require cautery or injection therapy.
Interventions. Esophagogastroduodenoscopy (EGD) has replaced barium studies for diagnosing UGI bleeding because of its greater accuracy and the potential for therapeutic interventions.6
• In stable patients, EGD is usually indicated to locate the bleeding source, arrest hemorrhage, and make a definitive diagnosis. Early endoscopy (within 24 hours) is usually recommended for most patients with acute UGI bleeding.
• Persistent UGI hemorrhage is an indication for immediate EGD. If bleeding is heavy, the source may not be identified. Patients with cirrhosis should have EGD because there may be more than one source of hemorrhage. Patients with visible bleeding vessels or varices are candidates for endoscopic treatment.
• Angiography. If bleeding continues and EGD fails to reveal the source, angiography may be useful in diagnosing bleeding from varices, vascular ectasias, and aneurysms. Angiography may also be useful in the management of esophageal varices and Mallory–Weiss tears and in the embolization of bleeding ulcers or tumors in patients who are not surgical candidates.
• Colonoscopy is generally required for patients with melena and a negative upper endoscopy.
SPECIAL CONSIDERATIONS
Bleeding from varices has a high recurrence rate and mortality (50% to 70%). Peptic ulcers with visible vessels have a rate of rebleeding of up to 50%. Other prognostic indicators include severity of the initial bleed, hemodynamic instability, hemoglobin <10 g per dL, active bleeding at the time of endoscopy, age (older patients have a higher mortality), concomitant disease, ulcer diameter greater than 2 cm, and the requirement for emergency surgery.7 The risk of rebleeding is reduced by treating H. pylori, prescribing proton pump inhibitors, co-treating patients who are prescribed NSAIDs with a proton pump inhibitor, prescribing β-blockers for patients with varices, and consideration of using somatostatin or octreotide.
REFERENCES
1. Esrailain E, Gralnek IM. Nonvariceal gastrointestinal bleeding: epidemiology and diagnosis. Gastroenterol Clin North Am 2005;34:589.
2. Rockney DL. Major causes of upper gastrointestinal bleeding in adults. http://www.uptodate.com/contents/major-causes-of-upper-gastrointestinal-bleeding-in-adults? Updated August 14, 2013.
3. Saltzman JR. Approach to acute upper gastrointestinal bleeding in adults. http://www.uptodate.com/contents/approach-to-acute-upper-gastrointestinal-bleeding-in-adults? Updated October 03, 2014.
4. Saltzman JR. Overview of the treatment of bleeding peptic ulcers. http://www.uptodate.com/contents/overview-of-the-treatment-of-bleeding-peptic-ulcers? Updated October 03, 2014.
5. Bajaj JS, Sangual AJ. Management of acute variceal hemorrhage. www.uptodate.com. 2014.
6. Barkun AN, Bardou M, Kuipers RJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 2010;152:101–113.
7. Srygley FD, Geradao CJ, Tran T, et al. Does this patient have a severe upper gastrointestinal bleed. JAMA 2012;307:1072–1079.
| Cholelithiasis and Cholecystitis |
ASYMPTOMATIC CHOLELITHIASIS
Background
Definition
• Asymptomatic gallstones are those discovered incidentally by abdominal imaging (ultrasonography [US] or computed tomography [CT]) being performed for unrelated symptoms or diseases. Patients will have no symptoms attributable to the presence of cholelithiasis.
Anatomy
• The gallbladder is an elongated pear-shaped sac (7 to 10 cm long, 2.5 to 3.5 cm wide) that stores and concentrates bile and releases it in response to a meal.
• A moderately distended gallbladder can contain 50 to 60 mL of bile, but may become much larger (300 mL) with pathological processes.
• The gallbladder is lined by simple columnar epithelium that is responsible for the active absorption of water used to concentrate bile.
Epidemiology
• The prevalence of asymptomatic gall stones varies with age, sex, race, and ethnicity. Screening ultrasound studies of select populations suggests an overall incidence of 5% to 21%.1,2 Overall rates are higher in females, individuals in the seventh decade of life and in individuals of Hispanic descent (as compared to white, black, or Asian).3
Pathophysiology
• Conjugated bile salts, lecithin, and cholesterol comprise 80% to 95% of solids dissolved in bile.
• Cholesterol solubility depends on the relative concentration of cholesterol, bile salts, and phospholipids.
• Imbalances in these concentrations result in precipitation of cholesterol crystals, which, over time, results in gallstone formation.
• Gallstones may occur due to high biliary cholesterol concentration, defective formation of micelles, cholesterol crystal nucleation factor excess (e.g., calcium), deficiency of anti-nucleating factors (e.g., lecithin), delayed gallbladder emptying, or excessive biliary excretion of bile (hemolytic anemia).4
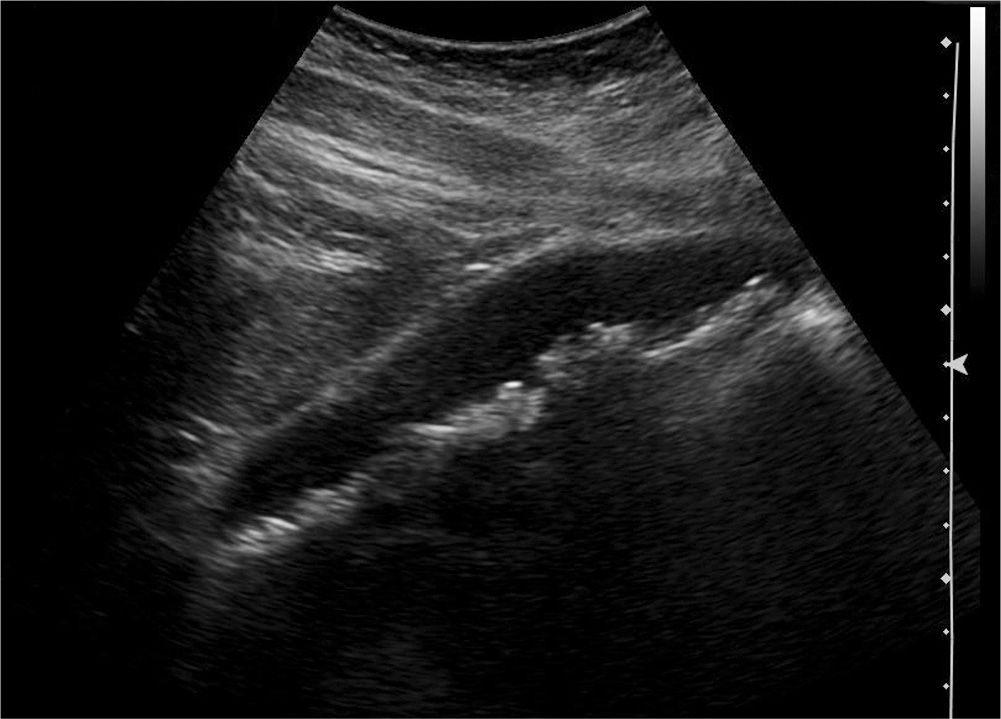
Figure 11.4-1. Longitudinal ultrasound view of the gallbladder demonstrating multiple dependent hyperechoic structures with posterior shadowing artifact consistent with multiple small gallstones.
Diagnosis
Clinical Presentation
• Asymptomatic gallstones are usually discovered incidentally on abdominal imaging (x-ray, US, or CT) or at the time of surgery for nonbiliary tract disease.
History
• Unremarkable, except for the risk factors noted above.
Physical Examination
• Generally unremarkable; however, stigmata of associated diseases may be found (cirrhosis, obesity, anemia, diabetes, etc.).
Laboratory Studies
• Generally unremarkable; however, abnormalities of associated diseases may be found (e.g., anemia from hemolysis).
Imaging
• Abdominal US, CT scan, or x-ray demonstrates gallstones (Figure 11.4-1).
Monitoring
• The majority of patients with asymptomatic cholelithiasis can be managed expectantly, no additional testing or follow-up is warranted.5
• Only 1% to 4% becomes symptomatic each year.6
• 60% to 70% of patients will never develop symptoms.5
Treatment
Medications
• Medical therapy for gallstones with oral bile acid therapy is generally not recommended for asymptomatic patients.
Protocol
• Recommendations for the treatment of gallstones have been developed by the Society for Surgery of the Alimentary Tract (http://www.ssat.com/cgi-bin/chole7.cgi) and by the Society of American Gastrointestinal and Endoscopic Surgeons (http://www.sages.org/publications/guidelines/guidelines-for-the-clinical-application-of-laparoscopic-biliary-tract-surgery/).
Surgery
• Prophylactic cholecystectomy is not indicated for asymptomatic patients, including patients with hemolytic anemia, patients undergoing bariatric surgery, and those with comorbid conditions (diabetes, cirrhosis, hemolytic anemia).
• Surgical referral is appropriate once symptoms begin, as recurrent symptoms develop in 70% to 80%.5 Biliary colic is the presenting symptom in the majority of patients (see Symptomatic Cholelithiasis below).
• Complications (acute cholecystitis, cholangitis, and pancreatitis) generally occur after symptom onset; these are uncommonly the initial presenting symptom.
• Cholecystectomy for asymptomatic patients with a calcified (“porcelain”) gallbladder or with gallstones larger than 3 cm should be considered due to a higher risk of gall bladder cancer in these patients.
Counseling
• Patients should be reassured that no surgery is indicated for asymptomatic cholelithiasis.
• Patients should be advised to seek medical care if they develop symptoms of acute cholecystitis, cholangitis, or pancreatitis (see below).
Patient Education
• American Academy of Family Physicians: http://familydoctor.org/familydoctor/en/diseases-conditions/gallstones.html
• American Gastroenterological Association: http://www.gastro.org/patient-center/digestive-conditions/gallstones
• National Institutes of Health, National Digestive Diseases Information Clearinghouse: http://digestive.niddk.nih.gov/ddiseases/pubs/gallstones/index.aspx
SYMPTOMATIC CHOLELITHIASIS
General Principles
Definition
• The term symptomatic cholelithiasis is applied to gallstones to which patient symptoms can be attributed. Although this definition is somewhat simplistic, determining whether a patient’s foregut symptoms are the result of gallstones or alternate pathophysiology (e.g., peptic ulcer disease, reflux esophagitis, gastroparesis, etc.) can be challenging.
Epidemiology
• As noted above, the majority of patients with cholelithiasis have no symptoms; however, the 15-year cumulative probability of developing symptoms (biliary colic or other complications) is 18% of initially asymptomatic patients.5 Patients with symptomatic cholelithiasis are at a higher risk for developing gallstone-related complications (acute cholecystitis, biliary pancreatitis) than those without symptoms.7
• Patients with symptomatic cholelithiasis follow one of the following three clinical courses:
1. Resolution of symptoms is seen in >50% of patients in one study, and is facilitated by avoiding exacerbating factors (i.e., fatty foods).8
2. Symptoms may persist or worsen.
3. Patients may develop gallstone-related complications, including choledocholithiasis, acute cholelithiasis, cholangitis, and acute biliary pancreatitis. Acute cholecystitis is the most common severe complication of gallstones, developing in 1% to 3% of patients with symptomatic cholelithiasis per year.9
Pathophysiology
• Pain related to gallstones typically occurs when a stone transiently obstructs the infundibulum–cystic duct junction, resulting in a partial obstruction of the gallbladder.
• Cholecystokinin-induced gallbladder emptying is inhibited, and contraction in the setting of an obstruction results in pain from significant increases in pressure within the gallbladder.
Diagnosis
Clinical Presentation
• The classic description of biliary colic is sudden onset right upper quadrant (RUQ) or epigastric pain that radiates to the back or right shoulder.
• Pain typically lasts less than 1 hour, and is commonly associated with nausea, vomiting, and diaphoresis.
• Pain is usually described as an intense dull pressure and is less commonly identified as true colic (sharp, intermittent, or spasmodic pain).
• Pain usually occurs postprandial (especially meals with high fat content) or at night.
History
• Patients may have a known history of asymptomatic cholelithiasis or may present with biliary colic as their initial presenting symptom of cholelithiasis.
Physical Examination
• Generally unremarkable; however, stigmata of associated diseases may be found. Patients may have residual RUQ pain on palpation.
• Fever or tachycardia suggests the development of complicated gallstone disease.
Laboratory Studies
• Generally unremarkable; however, abnormalities of associated diseases may be found (e.g., anemia from hemolysis).
• Leukocytosis, transaminitis, or elevations in amylase and lipase suggest the development of complicated gallstone disease.
Imaging
• Ultrasound has an 84% sensitivity and a 99% specificity for detecting gallstones and is the diagnostic test of choice for diagnosing gallstones and their complications (Figure 11.4-1).10
Monitoring
• Patients with symptomatic cholelithiasis should be referred to a surgeon for consideration of elective cholecystectomy.
• Patients who elect to undergo observation of their symptomatic cholelithiasis (rather than surgery) require no additional monitoring or testing in the absence of new or changing symptoms.
Pathologic Findings
• Gallstones will be seen on pathologic examination of the gallbladder (Figure 11.4-2). Pathological alterations of the gallbladder itself, including chronic inflammation and wall thickening, may also be noted.
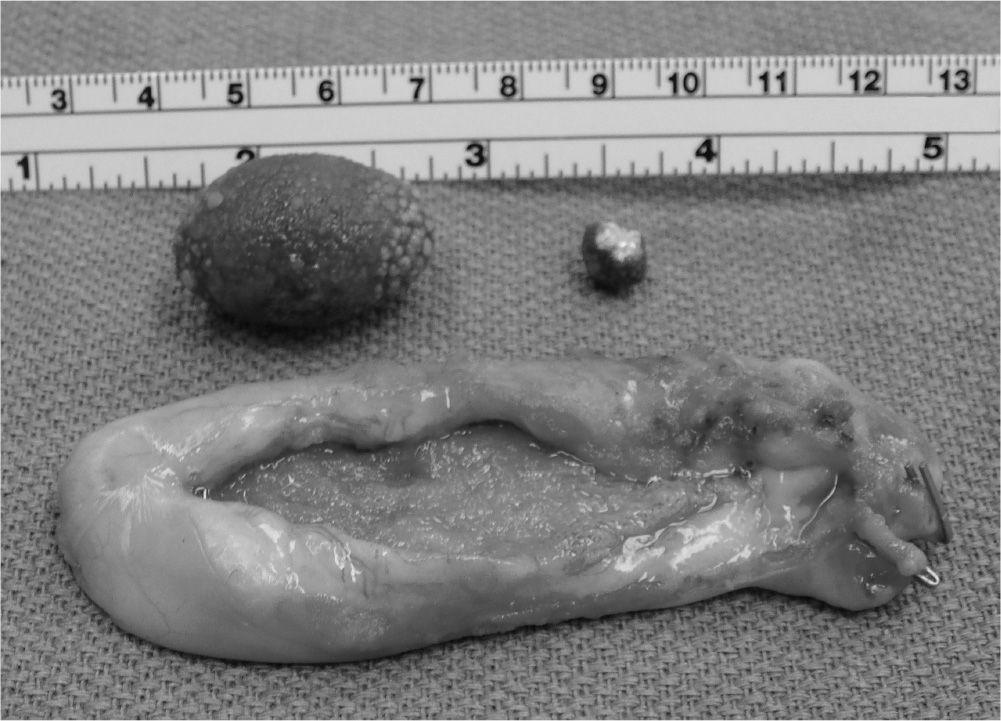
Figure 11.4-2. Operative photo of a large and a small gallstone from a patient with postprandial biliary colic undergoing cholecystectomy. The opened gallbladder with a thickened wall is in the foreground.
Differential Diagnosis
• The differential diagnosis of symptomatic cholelithiasis should include any upper abdominal and foregut disease, including gastroesophageal reflux, peptic ulcer disease, pancreatitis, complicated gallstone disease, and hepatitis. Small bowel and colon pathology (such as irritable bowel or inflammatory bowel disorders) should also be considered.
Treatment
Medications
• Pain management
• Nonsteroidal anti-inflammatory drugs (NSAIDs) have a proven benefit in alleviating pain associated with gallstones.11
• Oral ibuprofen or intravenous (IV) ketorolac can be utilized in the chronic and acute setting settings, respectively.
• Narcotics are also utilized in the management of symptomatic cholelithiasis.
• Oral oxycodone or IV morphine can be utilized in the chronic and acute settings, respectively.
• Dissolution therapy
• Oral bile salt therapy with ursodeoxycholic acid works best on pure cholesterol stones. The presence of calcium (and calcium salts) within the stones limits the effectiveness of dissolution therapy.
• Oral dissolution therapy works best with:
• Patients with minimal symptoms, small, non-calcified stones (<1 cm) and an otherwise normal functioning gallbladder.12
Surgery
• Laparoscopic cholecystectomy is recommended for patients with symptomatic cholelithiasis.
• Newer methods of laparoscopic surgery, including robotic assisted laparoscopy, single-incision laparoscopy or natural orifice (transvaginal) surgery, may be offered to select patients.
• Open cholecystectomy may be necessary in some patients due to previous surgical history or due to problems encountered during an attempted laparoscopic cholecystectomy.
Results
• 92% of patients with symptomatic cholelithiasis will have resolution of their symptoms following cholecystectomy.13
• Patients with atypical gallstone symptoms (gas bloat, belching, lower abdominal pain) are less likely to have complete symptom resolution.
Counseling
• The decision to perform surgery for symptomatic cholelithiasis depends on the degree of symptoms, the patient’s surgical risk (age, body mass index, comorbid conditions, and past surgical history), and their willingness to tolerate risk.
• Risk of surgical complications from cholecystectomy (∼2%, one time).
• Risk of developing an acute gallstone-related problem (∼3% per year) that may require a more complex series of procedures.
Special Considerations
• Expectant observation, dietary modification, or medical dissolution therapy may be recommended for patients who are poor surgical candidates.
• Pregnant patients with symptomatic cholelithiasis are generally managed expectantly unless their symptoms are severe or result in failure to gain weight as the pregnancy progresses. In these cases, elective cholecystectomy should be performed during the second trimester.
Patient Education
• Society of American Gastrointestinal and Endoscopic Surgeons: http://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-gallbladder-removal-cholecystectomy-from-sages/
ACUTE CHOLECYSTITIS
General Principles
Definition
• Sudden onset inflammation and infection resulting from complete obstruction of gallbladder emptying.
Epidemiology
• Develops in 1% to 3% of patients with symptomatic cholelithiasis per year.9
Pathophysiology
• Obstruction of the cystic duct with a gallstone results in acute inflammation and infection of the gallbladder.
Etiology
• Obstruction of the cystic duct results in gallbladder distention and bile stasis. Propagation of a cytokine cascade furthers the inflammatory process. Some (but not all) patients develop an infection within the gallbladder itself, typically with enteric organisms.
Diagnosis
Clinical Presentation
• Patients complain of fever and RUQ or epigastric pain radiating to the back or shoulder. They may have associated nausea, vomiting, and diaphoresis. Pain may be more intense and longer (hours) in duration than prior bouts of biliary colic.
History
• The majority of patients will have a history of symptomatic cholelithiasis (although a formal diagnosis may or may not have been made).
Physical Examination
• A wide variety of findings may be present depending on the degree of the systemic inflammatory response.
• Fever, tachycardia, and focal RUQ peritoneal signs are common findings.
• Hypotension and diffuse peritoneal signs suggest sepsis from a severe infection (gangrene or perforation of the gallbladder).
• Cessation of inspiration during palpation over the gallbladder (Murphy’s sign) is sensitive (97%) but not specific (48%) for acute cholecystitis.14
Laboratory Studies
• Leukocytosis with a left shifted differential is common.
• Mild transaminitis, hyperbilirubinemia, and alkaline phosphatase elevations are common and non-specific.
Imaging
• US will demonstrate gallstones, gallbladder wall edema and thickening (>4 mm), and pericholicystic fluid. The sonographer may also elicit a “sonographic Murphy’s sign” during the examination.
• Scintigraphy using 99mTc-hepatic iminodiacetic acid (HIDA) scan is utilized when the diagnosis is not clear following US. In acute cholecystitis, the gallbladder will not be visualized because radiotracer will not enter it due to cystic duct obstruction.
• Many patients have a CT scan performed, although this is generally unnecessary unless it is being used to evaluate for alternative pathologic diagnoses. The scan may demonstrate pericholicystic fluid, inflammatory stranding, gallbladder wall thickening, and possibly gallstones (Figure 11.4-3).
Monitoring
• Acute cholecystitis warrants urgent medical treatment. Patients should be referred to an acute care facility for diagnostic studies, medical management, and surgical consultation.
Pathologic Findings
• Gallstones, gallbladder wall thickening, edema, inflammation, and ischemia are all common pathologic findings on gallbladder specimens.
Differential Diagnosis
• Perforated viscus, acute appendicitis, cholangitis, hepatitis, acute pancreatitis, pelvic inflammatory disease (with peri-hepatitis), and diverticulitis should all be in the differential diagnosis of acute cholecystitis.
Treatment
Medications
• Narcotic pain medications are the preferred mode of analgesia.
• While there are data to suggest that NSAIDs may reduce the inflammatory reaction, many of these agents (e.g., ketorolac) increase the bleeding risk during operative intervention, and therefore should be avoided.

Figure 11.4-3. CT scan of a patient with acute cholecystitis. There is fluid and stranding surrounding the gallbladder (arrow) with gallbladder wall thickening.
• Broad-spectrum penicillins or cephalosporins are the empiric antibiotics of choice and have been shown to reduce septic complications.15
Surgery
• Laparoscopic cholecystectomy remains the procedure of choice for acute cholecystitis, although the risk for conversion to an open procedure is somewhat higher in the setting of an acute inflammatory response.
Results
• Mortality following cholecystectomy for acute infection is 0.5%, whereas morbidity ranges from 5% to 20%.16
Special Considerations
• Patients who are unfit surgical candidates should undergo percutaneous decompression of the gallbladder with a cholecystostomy tube, which may be placed under local anesthesia only.
• Pregnant patients with acute cholecystitis should undergo cholecystectomy.
CHRONIC CHOLECYSTITIS
General Principles
Defined
• Recurrent inflammatory process involving the gallbladder.16
Epidemiology
• Approximately 25% of persons with gallstones eventually develop chronic cholecystitis, although most remain asymptomatic.2
Pathophysiology
• Subepithelial fibrosis and mononuclear cell infiltrate with resultant scarring and dysfunction of the gallbladder.16
Etiology
• Thought to be intermittent obstruction of the cystic duct by gallstone.16
Diagnosis
Clinical Presentation
• Many times asymptomatic or with radiographic evidence of gallstones.
History
• Episodic RUQ pain with radiation to the back or right scapula. Nausea and vomiting associated 60% to 70% of the time.16
• Episodes lasting 1 to 5 hours distinguishing it from acute cholecystitis.
• May be associated with pain after meals, dyspepsia, flatulence, and fatty food intolerance although this is less specific for gallbladder disease.17
• Patient feels well between attacks.
Physical Examination
• Usually a normal physical examination when not having attacks.
• May have mild RUQ tenderness.
Laboratory Studies
• Liver function test is typically normal in asymptomatic disease.
Imaging
• US—study of choice due to its high sensitive (95% to 98%) for gallstones.
• Abdominal radiographs are less helpful; only 10% to 15% of gallstones will be calcified enough to be identified.
• CT—only 50% of gallstones are identified due to the fact that most are isodense with bile.16
Differential Diagnosis
• Acute cholecystitis, asymptomatic cholelithiasis, peptic ulcer disease, biliary dyskinesia, pancreatitis, acute hepatitis, appendicitis, hepatic abscess, acute renal pathology, right-sided pneumonia, myocardial infarction
Treatment
Medications
• Dissolution therapy can be considered in nonsurgical candidates or patients who refuse surgery.
• Bile acid salts may provide dissolution (as described above).
• 40% to 60% success after 12 to 24 months with carefully selected patients.
• 25% to 50% will recur within 5 years. Therefore, should consider maintenance therapy.17
Surgery
• Elective laparoscopic cholecystectomy is the treatment of choice.
Results
• Mortality <0.3% in the United States.
• <10% of patients with complications.
• 90% will be symptom free following surgery.13
Special Considerations
• Persistent RUQ pain, chills, or fevers suggestive of choledocholithiasis, cholangitis, or other biliary diseases.
• Pregnancy with chronic cholecystitis is managed conservatively until delivery unless severe metabolic changes or symptomatology exist.
• Patients with chronic cholecystitis undergoing other surgical procedures should have consideration given to concomitant cholecystectomy if appropriate.
ACALCULOUS CHOLECYSTITIS
General Principles
Definition
• Acute or chronic signs and symptoms of biliary colic or cholecystitis in the absence of gallstones.
Epidemiology
• A slim minority (<1%) of patients with presentation of cholecystitis.
Pathophysiology
• Unclear for acute acalculous cholecystitis but appears that gallbladder stasis and progression to ischemia can play a causative role and course typically complicated with gangrene, perforation, and peritonitis.16
• Association with critically ill individuals who have had major surgeries, trauma, and burns, or who have required long-term parenteral nutrition.16
• Chronic acalculous cholecystitis may be associated with biliary dyskinesia.16
Diagnosis
Clinical Presentation
• Acute acalculous cholecystitis—acute RUQ pain and fever almost exclusively in a critically ill patient.
• Chronic acalculous cholecystitis—intermittent biliary colic (RUQ pain, food intolerance, and nausea).
• Presentation may be severely delayed due to the critical illness of the patient or due to atypical symptoms.
Physical Examination
• Fever.
• RUQ pain may be difficult to elicit in the critically ill patient.
• May be normal in chronic acalculous cholecystitis.
Laboratory Studies
• Leukocytosis.
• Could have complicated picture with associated critical illness.
• Abnormal metabolic studies and coagulation panel in septic shock and multiorgan failure.
• May be normal in chronic acalculous cholecystitis.
Imaging
• US and CT findings with gallbladder wall thickening and pericholecystic fluid in the absence of gallstones.16
• HIDA scan has a controversial roll in chronic acalculous cholecystitis, but an ejection fraction <35% at 20 minutes felt to be abnormal.16
Treatment
Medication
• Same as for acute calculous cholecystitis.
• Recognized high incidence of gangrene and empyema (>50%) warrants broad-spectrum antibiotic coverage.16
Surgery
• Cholecystectomy is warranted for a high suspicion or confirmed diagnosis.
• Timing of surgery is highly dependent on clinical scenario of a critical ill patient.
• Cholecystostomy tube should be placed in patients unfit for surgical cholecystectomy.
Results
• Mortality for acute acalculous cholecystitis is high at 40% typically because of concomitant disease as well as the delayed diagnosis of gallbladder infection.16
CHOLEDOCHOLITHIASIS
General Principles
Definition
• The presence of a gallstone within the biliary tree (e.g., common bile duct [CBD], common hepatic duct, etc.)
Anatomy
• The CBD is formed by the junction of the common hepatic duct and cystic duct. It is 3 to 4 cm in length passing commonly through the pancreas to its insertion into the second portion of the duodenum. Its diameter is 5 to 13 mm.18
Epidemiology
• Incidence of CBD stones seen before or during cholecystectomy is approximately 12%.19 Fifteen percent of CBD stones are found in combination with gallstones.20 It is felt that 73% will pass spontaneously.20
Pathophysiology
• Stones can become obstructive in the lower end of the CBD and the tapered portion within the pancreas and ampulla. A ball-valve mechanism can also occur where the stone falls back into the CBD after failing to pass.19
• Complete or partial obstruction can cause accumulation of bacteria, ischemia, and necrosis. Infection can lead to as ascending cholangitis. Ischemia and necrosis lead to chronic stricture formation.
Diagnosis
History and Clinical Presentation
• RUQ pain or biliary colic radiating to the back or scapula.19
• More commonly can be found silent or at the time of cholecystectomy.
• Patients can present with complications such as obstructive jaundice, pancreatitis, or ascending cholangitis. Presentation can be biliary pain (steady, increasing, >4 to 6 hours, right scapular radiation), jaundice, and fevers. Progression to mental status changes and hypotension may represent acute suppurative cholangitis.19
• Predictors of CBD stone: cholangitis, ultrasound findings (stone, CBD dilation), jaundice, hyperbilirubinemia, elevated alkaline phosphatase, pancreatitis, cholecystitis, elevated amylase, or lipase.21
Physical Examination
• Typically normal unless complication. Depending on the complication, patients could present with fevers, hypotension, tachycardia, jaundice, RUQ pain, epigastric pain, pruritus, tea-colored urine, and acholic stools.
Laboratory Studies
• Elevated serum bilirubin, alkaline phosphatase, transaminases, and γ-glutamyl transpeptidase. Because liver function assays can be elevated in a variety of diseases, the positive predictive value of these tests is overall low, but the negative predictive value of normal tests is high and is useful to exclude choledocholithiasis.
• Leukocytosis.
• Positive blood cultures are possible in cholangitis.
• Elevated pancreatic enzymes in suspected biliary pancreatitis.
• Urine bilirubin.
Imaging
• Ultrasound—23% to 80% detected depending on body habitus and operator experience.22
• CT—75% sensitivity for showing CBD stones with obstruction.23
• Endoscopic ultrasound—93% sensitive and 97% specific.24
• MRI cholangiopancreatography is 95% sensitive and 89% specific for choledocholithiasis.25
Surgical Diagnostic Procedures
• Intraoperative cholangiography (IOC) is useful for diagnosing CBD stones in patients undergoing cholecystectomy. It has a high sensitivity and specificity, but is highly operator dependent.
• Endoscopic retrograde cholangiopancreatography (ERCP) is uncommonly used solely as a diagnostic tool for choledocholithiasis due to the risk of post-ERCP pancreatitis.
Treatment
Medication
• No medical treatment regimens recommended specifically for the treatment of choledocholithiasis.
• Medical management of symptomatic CBD stone revolves around clinical scenario.
• Pain management—IV opioid analgesics.
• Preoperative—NPO, IV fluids, electrolyte correction, anticoagulant recognition, and management.
• Cholangitis—broad-spectrum antibiotics with coverage for Enterobacteriaceae (68%), Enterococci (14%), Bacteroides (10%), and Clostridium (7%); anti-pseudomonal penicillin β-lactamase inhibitor (e.g., piperacillin/tazobactam); or in life-threatening scenarios carbapenems.26
Surgery
• The mode of stone removal depends on when the stone is discovered.
• If choledocholithiasis is identified before or after cholecystectomy, ERCP is generally considered the therapeutic procedure of choice (Figure 11.4-4).
• If choledocholithiasis is identified on an IOC, treatment will depend on surgeon’s preference, clinical scenario, and health care facility resources.
• Options include laparoscopic or open CBD exploration (transcystic or via a choledochotomy) or an ERCP performed intraoperatively or postoperatively.
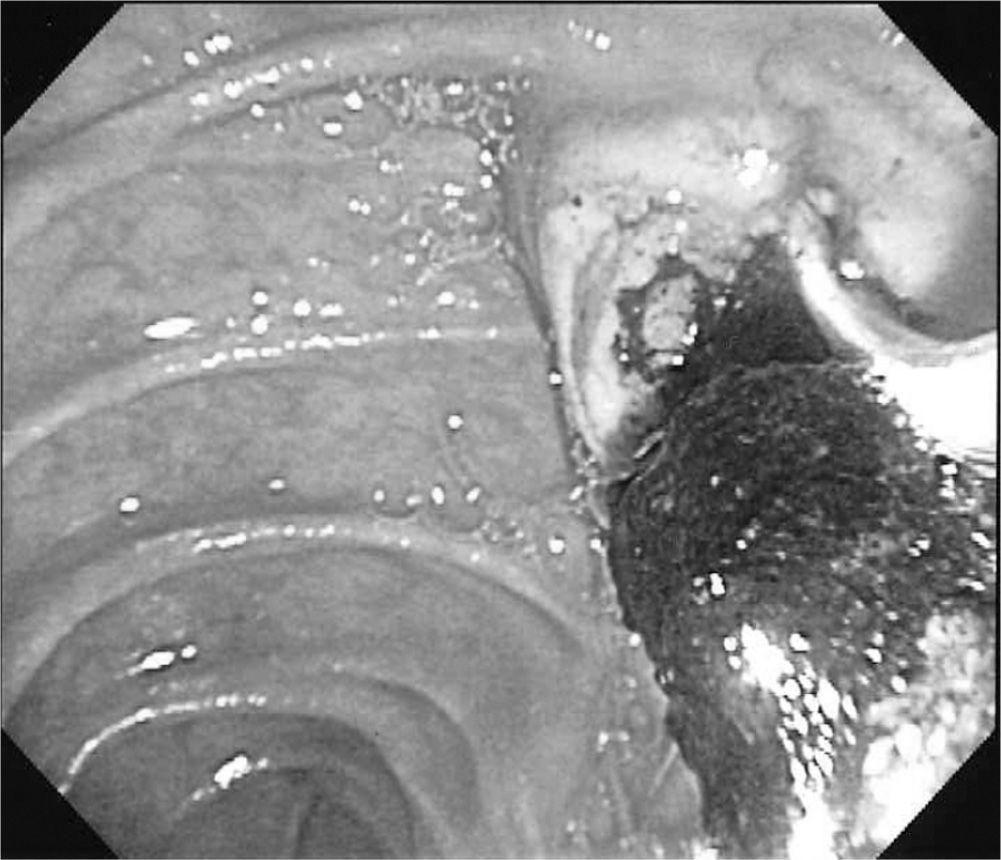
Figure 11.4-4. Endoscopic view of balloon extraction of common bile duct stone extraction from the ampulla of Vater during ERCP.
Special Considerations
• Mortality rate of cholangitis in association with CBD stones is 2% to 5%.16
• CBD stones account for 50% of all cases of pancreatitis.16
REFERENCES
1. Barbara L, Sama C, Morselli Labate AM, et al. A population study on the prevalence of gallstone disease: the Sirmione Study. Hepatology 1987;7:913–917.
2. Glambek I, Kvaale G, Arnesjö B, et al. Prevalence of gallstones in a Norwegian population. Scand J Gastroenterol 1987;22:1089–1098.
3. Everhart JE, Khare M, Hill M, et al. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 1999;117:632–639.
4. Venneman NG, Erpecum K. Pathogenesis of gallstones. Gastroenterol Clin N Am 2010;39:171–183.
5. Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med 1982;307:798–800.
6. Beckingham IJ. Gallstone disease. BMJ 2001;322:91–94.
7. Friedman GD, Raviola CA, Fireman B. Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol 1989;42:127–136.
8. Festi D, Reggiani ML, Attili AF, et al. Natural history of gallstone disease: Expectant management or active treatment? Results from a population-based cohort study. J Gastroenterol Hepatol 2010;25:719–724.
9. Friedman GD. Natural history of asymptomatic and symptomatic gallstones. Am J Surg 1993;165:399–404.
10. Shea JA, Berlin JA, Escarce JJ, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med 1994;154:2573–2581.
11. Colli A, Conte D, Valle SD, et al. Meta-analysis: nonsteroidal anti-inflammatory drugs in biliary colic. Aliment Pharmacol Ther 2012;35:1370–1378.
12. Tomida S, Abei M, Yamaguchi T, et al. Long-term ursodeoxycholic acid therapy is associated with reduced risk of biliary pain and acute cholecystitis in patients with gallbladder stones: a cohort analysis. Hepatology 1999;30:6–13.
13. Berger MY, Olde Hartman TC, Bohnen AM. Abdominal symptoms: do they disappear after cholecystectomy? Surg Endosc 2003;17:1723–1728.
14. Singer AJ, McCracken G, Henry MC, et al. Correlation among clinical, laboratory, and hepatobiliary scanning findings in patients with suspected acute cholecystitis. Ann Emerg Med 1996;28:267–272.
15. Indar A, Beckingham I. Acute cholecystitis. BMJ 2002;325:639–643.
16. Pitt H, Ahrendt S, Nakeeb A. Calculous biliary disease. In: Mulholland M, Lillemoe K, Doherty G, et al., eds. Greenfield’s surgery-principles and practice. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:960–980.
17. Vincent E. Cholelithiasis and cholecystitis. In: Paulman P, Paulman A, Harrison J, eds. Taylor’s manual of family medicine. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:373–380.
18. Strasberg S. Hepatic, biliary, and pancreatic anatomy. In: Garden O, Parks R, eds. Hepatobiliary and pancreatic surgery. 5th ed. Edinburgh: Saunders Elsevier; 2014:17–38.
19. Nathanson L. Gallstones. In: Garden O, Parks R, eds. Hepatobiliary and pancreatic surgery. 5th ed. Edinburgh: Saunders Elsevier; 2014:174–195.
20. Bellows C, Berger D, Crass R. Management of gallstones. Am Fam Physician 2005;72:637–642.
21. Abboud BA, Malet PF, Berlin JA, et al. Predictors of common bile duct stones prior to cholecystectomy: a meta-analysis. Gastrointest Endosc 1996;44:450.
22. Lindsel DR. Ultrasound imaging of pancreas and biliary tract. Lancet 1990;335:390–393.
23. Baroll RL. Common bile duct stones. Reassessment of criteria for CT diagnosis. Radiology 1987;162:419–424.
24. Prat F, Amouyal G, Amouyal P, et al. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common bile duct lithiasis. Lancet 1996;347:75–79.
25. Hochwalk SN, Dobransky M, Rofsky NM, et al. Magnetic resonance cholangiopancreatography accurately predicts the presence or absence of choledocholithiasis. J Gastrointest Surg 1998;2:573–579.
26. Chambers H, Gilbert D, Eliopoulos G, et al. The sanford guide of antimicrobial therapy v.3.09. 43rd ed. In-App Subscription. Accessed February 28, 2014.
|
GENERAL PRINCIPLES
Definition
Hepatitis is defined as inflammation of the liver and can be caused by many etiologies. This chapter explores viral causes of hepatitis, which can cause both acute and chronic liver diseases. Differentiation of the exact viral cause is essential in the management of viral hepatitis, since each virus varies significantly in its mode of transmission, prevention, treatment, and clinical course.
Epidemiology and Classification
Hepatitis A
The hepatitis A virus (HAV) is a ribonucleic acid (RNA) enveloped picornavirus that has greatly declined in incidence to less than 10% of viral hepatitis infections since the introduction of progressive U.S. vaccine recommendations in 1996. The virus is spread via the fecal–oral route, and the average incubation period is 28 days (range, 15 to 50 days). As many as 70% of children under 6 years of age may be asymptomatic with a minority of young children presenting with jaundice. Adults and older children, on the other hand, are typically symptomatic, with approximately 70% presenting with jaundice. HAV infection is a self-limited disease with symptom resolution typically in 2 months without progression to chronic infection.
The virus is shed in the stool and primarily spread by contaminated water or food, personal contact, and drug use. Sexual contact, particularly in men who have sex with men (MSM), can also transmit the virus. The incidence rate of hepatitis A infection is 0.4 cases per 100,000 persons and accounted for an estimated 2,800 new infections in 2011.1 Rates of infection are slightly higher in Hispanics and Asian/Pacific Islanders, but men and women have similar rates. Although travel, household contacts, daycare centers, and intravenous drug use are risk factors for infection, over half of reported infections report no risk behaviors or exposures for hepatitis A during the 2 to 6 weeks prior to infection.
Hepatitis B
Hepatitis B virus (HBV) is a DNA double-stranded hepadnavirus that is present in blood and other bodily fluids. HPV is very efficiently transmitted via contact with infected serum, with needle-stick exposures to HBV-contaminated needles, resulting in disease in 6% to 24% of cases.2 Relatively resilient, HBV can survive for up to 7 days outside of a human host.3 The incubation period for HBV is typically 2 to 3 months (range of 6 weeks to 6 months), which can then result in acute, symptomatic illness in 30% to 50% of all individuals. However, children younger than 5 years and immunosuppressed persons are more likely to be asymptomatic.3 Risk of progression from acute to chronic infection is typically inversely proportional to age with the greatest risk occurring in infants at 90%; likewise, the risk of chronic infection after acute infection reduces to about 5% in individuals over 5 years of age.3
Since the implementation of a national vaccination program for HBV in the 1990s, the incidence of acute HBV infection in the United States has significantly declined. Specifically, reported annual incidence of acute HBV dropped from 11.5 cases per 100,000 population in 1985 to 1.6 cases per 100,000 population in 2006.3,4 At a 98% reduction, the decline was highest for those under 15 years old, for whom universal infant vaccination or childhood catch-up vaccination was recommended.4 Notwithstanding this success in primary prevention, the burden of chronic infection with HBV still affects an estimated 800,000 to 1.4 million members of the United States.3 Prior to HBV vaccination, about 30% to 40% of these cases occurred through maternal–fetal transmission, particularly in women of Asian descent where disease prevalence is high. In the United States, estimated annual deaths due to chronic HBV from associated liver diseases such as failure, cirrhosis, and hepatocellular cancer range from 2,000 to 4,000 deaths per year.3 For acute infection, case fatality rates in the United States are approximately 1% due to fulminant hepatic failure.4
Hepatitis C
Approximately 3.2 million persons in the United States are chronically infected with the hepatitis C virus (HCV), making it the most common blood-borne infection in the nation. Prevalence is highest at 3.25% in those of the “baby boomer generation” born between 1945 and 1965, which accounts for three-fourths of all HCV infections and 73% of HCV-associated mortality.5 Those with additional risk factors and higher prevalence also include those with a history of intravenous drug use, 20 or more lifetime sexual partners, blood transfusion before 1992, men, non-Hispanic blacks, and prison inmates. Fifty-seven percent of patients aged 20 to 59 years who had ever used injection drugs were found to have antibodies to HCV, making it the greatest predictor of risk.6 However, over half of patients infected with HCV are unaware of their infection and have never been tested for HCV.7
Sixty to 70% of persons newly infected with the HCV are typically asymptomatic or have mild symptoms that do not prompt them to seek medical attention, making reporting of acute HCV infections and risk for chronic infection, which develops in 75% to 85% of acutely infected persons, challenging. The incidence of HCV infection increased steadily in the 1980s with a peak incidence of 380,000.8 Subsequently, the incidence has declined as HCV was identified in 1988 and sensitive blood screening was developed and implemented in 1992. According to the Centers for Disease Control and Prevention1 in 2011, there were 1,229 reported cases of acute HCV, representing an estimated 16,500 (7,200 to 43,400) actual acute cases.1 This is a 45% increase in 2011 compared with 2010 after 6 years of little change in incidence. The increase is attributed to increase HCV infections among adolescents and young adults with risk factors that include persons who have used injection drugs or opioids, are white, and live in nonurban areas. Unfortunately, lack of diagnosis, linkage to care, and treatment for those that are chronically infected allow for continued transmission of HCV and continued morbidity and mortality due to hepatitis C infection. By 2007, HCV infection superseded human immunodeficiency virus (HIV) as a cause of death in the United States, and HCV infection is currently the number one cause for liver transplantation.9
The HCV is most efficiently transmitted though percutaneous exposure to blood, with transfusion of unscreened blood or use of injection drugs presenting the greatest risk. Infection can also occur less commonly via occupational, perinatal, and sexual transmission. Healthcare workers are at particular occupational risk, with a 1.8% risk of HCV infection after a needle injury10 and greatest risk with deep injuries and procedures, which involve placement of a hollow-bore needle in the source patient’s vein or artery. The risk of maternal–fetal vertical transmission has been estimated to be 4.3% in mothers with HCV RNA present, with a higher rate of 19.4% in HIV-coinfected mothers.11 Method of delivery and breast feeding has not been shown to affect risk.
Sexual transmission has traditionally been thought to be rare. However, persons with multiple sex partners, MSM, or those who are coinfected with HIV are at higher risk for sexual transmission.12,13 Therefore, sexual transmission of HCV can occur but is much less efficient than by the percutaneous route.
Hepatitis D
Dependent on the viral mechanisms of HBV to replicate, the hepatitis D virus (HDV) infection must have requisite HBV coinfection. HDV interferes with HBV replication, making viral burden of HBV typically less. In the United States, HDV infection is predominantly in those receiving multiple blood products and users of intravenous drugs; however, HDV is endemic in the Mediterranean, Asia, and the Pacific islands. Approximately 5% of HBsAg-positive individuals are coinfected with HDV.14 HDV complicates HBV disease and can lead to earlier disease progression and a more complicated clinical course.
Hepatitis E
Hepatitis E virus (HEV) is a single-stranded RNA virus transmitted via fecal–oral transmission that typically causes only acute liver inflammation; however, immunosuppressed persons may have difficulty with clearance. To date, chronic HEV infection has been shown only in developing countries in persons who are immunosuppressed from solid organ transplantation.15 This disease is typically most prevalent in Asia, Africa, Middle East, and Central America. Incubation times vary from 15 to 60 days postexposure (mean of 40 days). Serologic evidence of exposure in the United States may be around 21%, and reasons why clinically meaningful symptomatic infection is not more frequently recognized are unclear.16
Other Viral Etiologies of Hepatitis
Multiple other viruses can cause liver inflammation as part of a broader viral syndrome and can be classified as non-hepatotropic, meaning they do not have particular predilection for hepatic tissue. Some alternative viral etiologies include herpes-type viruses such as Epstein–Barr virus (EBV), cytomegalovirus (CMV), varicella zoster virus (HZV), and herpes simplex. Other alternative viral etiologies include flaviviruses such as yellow fever virus and Dengue fever virus; non-polio enteroviruses such as cocksackie and echovirus; filioviruses including Ebola virus and Marburg virus; adenoviruses; Parvovirus B19; severe acute respiratory syndrome (SARS) virus; influenza virus; measles; rubella; and others. Only several of these warrant special attention.
Of the herpes viruses, EBV typically causes a syndrome referred to as mononucleosis, common in adolescents, which can cause hepatosplenomegaly with rash, fatigue, and exudative pharyngitis. Diagnosis is confirmed with predominance of atypical lymphocytes on complete blood count and the presence of heterophile antibodies. CMV can cause a similar syndrome that is heterophile-negative and plays an important role in hepatitis post-solid-organ transplant, where the immunosuppressant medications allow CMV infection to not infrequently cause acute/chronic graft injury and dysfunction. For instance, in liver transplant patients, antivirals and immunoglobulin may help prevent organ failure during CMV hepatitis of a liver graft. CMV infections in transplant recipients may be primary—CMV-seronegative patients receiving donor organ from CMV-seropositive patients—or secondary—CMV-positive recipients with reactivation after immunosuppression. Superinfection is also possible where reinfection occurs in CMV-seropositive recipients.
DIAGNOSIS
History
Initial evaluation of persons with suspected viral hepatitis infection should include a thorough discussion about ethnicity, country of birth, occupation, travel, close contacts, potential food or water exposures, and past and future high risk behaviors. Particular focus should be placed on drug use, receipt of blood products or an organ transplant before 1992, history of incarceration, previous sexually transmitted infections, HIV testing, and sexual practices. Prior or present symptoms of acute or chronic liver disease such as fever, fatigue, anorexia, abdominal pain, nausea, vomiting, dark urine, clay-colored stools, jaundice, rash, or arthralgias should be obtained. Acute infection may be asymptomatic depending on the viral etiology and age of the patient. Chronic infection is initially asymptomatic; but, as cirrhosis and subsequent liver failure develops, symptoms may include malaise, weight loss, abdominal swelling, jaundice, pruritus, bruising, bleeding, edema, or confusion. In addition, patients should be screened for alcohol use and questioned regarding hepatotoxic drugs or supplements. Those being considered for treatment should also have a thorough psychological evaluation and assessment for cardiopulmonary disease as well as other comorbidities.
Physical Examination
During a comprehensive physical examination, particular attention for signs of acute or chronic HCV infection would include a detailed skin examination looking for jaundice, nail changes, ecchymosis, petechiae, palmar erythema, or spider hemangiomata, which are typically found on the chest or shoulders. Men should be examined for gynecomastia or hypogonadism. During the abdominal examination, it is important to detect the signs of portal hypertension such as hepatic or splenic enlargement, epigastric venous hum, ascites, or caput medusa with a rectal examination to detect rectal varices. Neurological examination would focus on determination of asterixis or altered mental status.
Laboratory and Imaging
Hepatitis A
The diagnosis of acute hepatitis A viral infection is confirmed by serum immunoglobulin M (IgM) anti-HAV testing, which has high sensitivity and specificity. Anti-HAV IgM is typically positive once symptoms develop and remain positive for up to 6 months. A false-positive result, prior immunity, or asymptomatic infection may be diagnosed in the setting of a patient without typical symptoms of acute hepatitis A infection with a positive anti-HAV IgM result. Serum immunoglobulin G (IgG) anti-HAV is present several weeks after the onset of acute infection and typically remains present indefinitely. Prior immunization or infection can be measured by total anti-HAV (IgM and IgG). Stool or serum detection is not commonly used in clinical practice for the detection of HAV.
Less specific serum laboratory findings include elevated transaminase levels, total and direct bilirubin, and alkaline phosphatase. The alanine transaminase (ALT) level is typically higher than the aspartate transaminase (AST) level, with transaminase levels in the several hundred to several thousand U per L range. Transaminase levels peak in elevation before the peak in bilirubin levels, which often rises above 10 mg per dL. Imaging is not routinely required in the absence of atypical features or other medical risk factors.
Hepatitis B
According to the United States Preventative Services Task Force (USPSTF), screening for HBV is most highly supported in pregnant women, where treatment of infants with neonatal HBV vaccination and hepatitis B immune globulin significantly reduces the rates of infant chronic infection.17 Screening is also recommended by the Centers for Disease Control and Prevention (CDC) for infants who are born to HBsAg positive; persons born in countries with HBsAg seropositivity ≥2%; unvaccinated, U.S.-born persons with a parent born in countries with HBsAg seropositivity rates ≥8%; persons infected with HIV; MSM; users of intravenous drugs; household, needle-sharing, or sexual contacts of persons who are HBsAg positive; persons initiating hemodialysis; persons undergoing evaluation for immunosuppressive therapy prior to treatment; donors of biologic material; persons whose blood or bodily fluids are the source of exposures that may have indications for postexposure prophylaxis; and persons with AST/ALT elevation of uncertain cause.3 Screening is performed by measurement of HPV surface antigen (HBsAg), HPV surface antibody (HBsAb), and HBV core antibody (HBcAb).
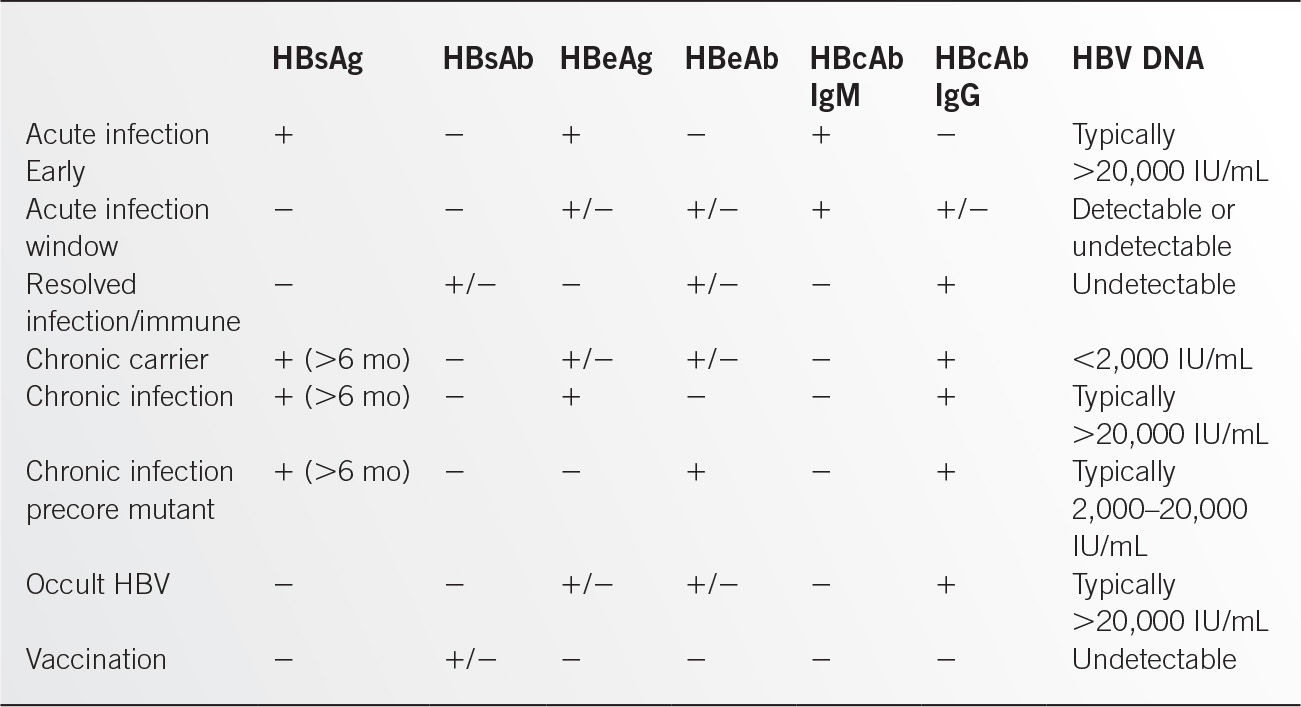
For acute hepatitis B infections, HBsAg, HBV envelope antigen (HBeAg), and HBcAb IgM are initially positive and then gradually sero-convert to HBV surface antibody (HBsAb), HBV envelope antibody (HBeAb), and HBV core immunoglobulin G antibody (HBcAb IgG). In addition to these serologic markers of infection, sensitive polymerase chain reaction (PCR) analysis of serum, and in some cases hepatic tissue via biopsy, can detect levels of HBV DNA. Hepatitis B serology is summarized in Table 11.5-1. HBsAg is indicative of current, active infection and, other than detection of HBV DNA, is the first serologic test to become positive after exposure. Evidenced by HBsAb, immunity can be gained either through vaccination or through resolved prior exposure and resolution of acute infection. HBcAb IgM is present early in acute infection and remains positive during the window period of seroconversion when HBsAg and HBsAb may be not detected. Because HBcAb can only be gained through exposure to HBV, it can identify patients who have been exposed to virus in the past and can help differentiate immunity of vaccination from immunity of resolved infection. HBeAg is an important test in those infected with HBV, since HBeAg is associated with replication and degree of infectivity and positively correlates with HBV DNA levels.
HBV disease surveillance involves monitoring of patients with established infection for development of cirrhosis and liver failure as well as periodic screening for hepatocellular carcinoma (HCC) in those at increased risk. Confirmed HBsAg-positive patients should undergo surveillance testing for HBeAg, viral DNA levels, and alanine aminotransferase (ALT) levels, and occasionally biopsy to identify HBeAg-negative infections and to determine prognosis, disease surveillance schedules, and indications for treatment. Additional testing involves monitoring of complete blood counts, prothrombin and partial thromboplastin times, and other liver function tests. Those persons at increased risk for HCC include persons who have family history of HCC, who are of Asian or African descent, who are older, and who have known cirrhosis. Estimates suggest that 15% to 40% of cases of chronic HBV infection develop hepatic complications.
To screen for HCC, ultrasound is more sensitive and specific than serum α-fetoprotein levels and is considered the test of choice for surveillance of HCC. Clinicians may choose to add α-fetoprotein levels to ultrasound if there are concerns about the interpretation or the validity of this operator-dependent test; additionally, where ultrasound is not locally available or when cost is prohibitive, α-fetoprotein is an acceptable alternative to ultrasonography. Frequency of monitoring is recommended to be every 6 to 12 months. Although HCC surveillance is a standard of care in management of HBV hepatitis, a Cochrane review of this practice found insufficient evidence to support its use to reduce mortality.18
Hepatitis C
In 2012, the Centers for Disease Control and Prevention (CDC) released the recommendation that persons born between 1945 and 1965 should be offered a test at least once for HCV infection regardless of HCV risk factors. The USPSTF in 2013 agreed to the same recommendation based on reliable available testing, benefits of detection and early intervention, and the prevalence of undiagnosed HCV infection in the “baby boomer” age group. These new screening recommendations are a change from the 1998 CDC guidelines, which only recommended testing for those with HCV risk factors. Risk-based screening of persons not born between 1945 and 1965 should be considered in intranasal drug users, those on long-term dialysis, those with unregulated tattoos, recipients of transfusions or organ transplants before July 1992, recipients of clotting-factor concentrates before 1987, and those that were ever incarcerated. Screening should also be considered for patients with unexplained elevated ALT levels. Annual HCV screening should be considered among persons who inject drugs and HIV-infected MSM.
Antibodies to the HCV (anti-HCV) testing are recommended for initial screening. FDA-approved tests for anti-HCV, which detect antibodies to HCV-encoded antigen, include laboratory-based enzyme immunoassays (EIAs) and a point-of-care immunoassay that can be done at home. The average time to detection of anti-HCV after exposure is 8 to 9 weeks, with >97% of persons testing positive 6 months after exposure. A positive anti-HCV test indicates current or past HCV infection or a false-positive result and should be confirmed with quantitative PCR testing for HCV RNA. HCV RNA can be detected in blood within 1 to 3 weeks after exposure, and may be the only positive test in those who are immunocompromised (e.g., those receiving chronic hemodialysis).
Acute hepatitis C can be distinguished from chronic hepatitis C infection based on testing both anti-HCV and HCV RNA. Acute hepatitis C infection is highly likely if HCV RNA is positive with negative anti-HCV. In chronic hepatitis C, both tests will remain positive. Acute HCV infection does not progress to chronic infection in 15% to 25% of cases and would result in positive anti-HCV and negative HCV RNA testing. A false-positive anti-HCV result is most likely in persons with no risk factors, and repeat HCV RNA testing 6 months later can be used to confirm the absence of chronic infection if suspicion is high.
Once the diagnosis of current HCV infection is made, additional laboratory testing can be helpful to guide treatment. A quantitative HCV RNA test provides a baseline from which to measure response to treatment, but it is neither an accurate measurement of duration of infection nor a predictor of progression to cirrhosis. The HCV genotype test is critical for determination of the optimal treatment regimen, duration, and likelihood of response. The HCV comes in six genotypes, with additional subtypes, that vary in prevalence by region. Genotype 1, which is the hardest to treat, is the most common in the United States and comprises 60% to 70% of HCV infections in this area. Genotypes 2 and 3 are also present in the United States with genotypes 4, 5, and 6 being rare. Before treatment, testing of renal function, hepatic synthetic function (bilirubin, prothrombin time, and albumin), a complete blood count, thyroid-stimulating hormone, and serum aminotransferases are also necessary as a baseline to monitor drug toxicities and to assess readiness for treatment.
Unfortunately, the quantitative HCV RNA viral level, HCV genotype nor the degree of aminotransferase level elevation is able to fully describe or predict the degree of liver damage, the development of HCC, or the progression to cirrhosis in an individual infected with the HCV. Approximately 30% of patients with chronic hepatitis C have persistently normal serum ALT levels, which often predict less risk for development of cirrhosis, but up to 29% of patients with normal ALT levels can have late-stage cirrhosis.19 Ultrasound can be useful for evaluation of the liver parenchyma, to screen for carcinoma, and look for extrahepatic manifestations of cirrhosis, but also cannot always determine the degree of fibrosis or presence of cirrhosis. CT is not routinely used since it is not significantly better than ultrasonography and adds radiation and contrast exposure. Liver biopsy, which is invasive and not without risk, remains the gold standard for determining the degree of liver fibrosis, which is useful in the decisions to proceed with treatment. Subsequently, noninvasive serologic (e.g., aspartate aminotransferase to platelet ration [APRI], Fibrotest/FiroSure, Hepascore) and radiologic tests (e.g., ultrasound elastography, magnetic resonance elastography) continue to be developed for use individually or in combination to better predict the degree of fibrosis.
Differential Diagnosis
The differential diagnosis of patients presenting with symptoms or signs of liver disease or mildly elevated liver enzymes, which may be the only initial laboratory finding in chronic infections, is very broad and may include other viral and nonviral infectious causes, alcoholic hepatitis, nonalcoholic steatohepatitis, autoimmune hepatitis, cholangitis, cirrhosis, drug-induced liver injury, hemochromatosis, hereditary metabolic disorders (e.g., Wilson disease, α1-antitrypsin deficiency), and HCC.
TREATMENT
Medications/Immunizations
Hepatitis A
Since hepatitis A viral infection is a self-limited disease, the treatment is supportive with a minority of patients requiring hospitalization or progressing to fulminant hepatic failure. In 2011, 43% of patients with reported hepatitis A infection required hospitalization and 0.7% died.1 Hepatic failure and death is more common in those with advanced age and chronic hepatitis C infection,20 although in the United States only approximately 3% of cases of acute liver failure between 1998 and 2007 were due to HAV.21
Immunization against the HAV has been extremely effective along with handwashing, water treatment and proper food handling at preventing the spread of hepatitis A infection. Initial 1996 Centers for Disease Control and Prevention (CDC) recommendations for vaccination targeted those at highest risk for disease transmission: international travelers, illicit drug users, MSM, persons with chronic liver disease, those with clotting-factor disorders, persons with occupational risk for infection, and children in areas with high rates of hepatitis A infection. The CDC’s Advisory Committee on Immunization Practices (ACIP) expanded these recommendations in 2006 to include all children starting at 12 months of age.
HAV vaccination, which is an inactivated vaccine, is recommended in two doses spread a minimum of 6 months apart, with a higher adult dose for those greater than 18 years of age. Vaccination is approved only for those 12 months of age or older and may be given to those who are immunocompromised. Postvaccination testing is not generally recommended since the vaccine is highly effective.
Postexposure prophylaxis for hepatitis A is also an effective treatment strategy to minimize the spread during outbreaks. Initially, intravenous immune globulin (IVIG) was the only method for the protection of exposed individuals. However, in 2007, the CDC updated their recommendations to include the use of a single dose of HAV vaccine within 2 weeks after exposure for those healthy persons aged 1 to 40 years.22 Vaccination is typically preferred in this group due to ease of administration, long-term protection, and equivalent efficacy to IVIG.23 Infants under 12 months of age, older persons, those who are immunocompromised, and persons with chronic liver disease should be given IVIG prior to travel to an endemic area or after exposure. Postexposure prophylaxis is needed only for close personal contacts (e.g., household and sex contacts, persons sharing illicit drugs, and child-care center staff, attendees and attendees’ household members) of those with confirmed hepatitis A infection.
Hepatitis B
Primary prevention of HBV through immunization plays an important role in population management of disease. The CDC recommends standard immunization schedule for all children under 18 years old with three-dose series at 0, 1, and 6 months. For adults, immunization is recommended for those at highest risk of contracting the virus or of having complications—healthcare workers, those at risk for sexual exposure, others at risk of needle exposure to HBsAg-positive individuals, HIV-positive individuals, intravenous drug uses, close personal/household contacts of those with HBV infection, those with end-stage renal disease or otherwise considering dialysis, those other chronic liver diseases, and those traveling to countries with endemicity >2%. Immunity postvaccination may be indefinite with immunological memory persisting even after HBsAb levels are no longer detectable.24 Postexposure prophylaxis is indicated for infants born to HBsAg-positive mothers; for persons, including healthcare workers, recently exposed to a needle of serum from an HBsAg-positive individual; or for persons with recent sexual exposure to an HBsAg-positive partner. Postexposure prophylaxis involves vaccination of all unvaccinated individuals and intramuscular administration of one dose of hepatitis B immune globulin at a dose of 0.06 mL per kg of body mass.
For chronic HBV infection, the main goals of treatment are to reduce viremia and to preserve liver function because chronic infection is not universally curable. The paragon of all treatment outcomes, delayed HBsAg seroconversion is only rarely achieved. Secondary goals of therapy are seroconversion of HBeAg and reduction of HBV DNA levels. Integral to evaluating risk of progression, testing is indicated for HIV and HCV coinfection for all patients and for HDV only in intravenous drug users in persons from countries with high HDV prevalence. All patients with HBV should also be vaccinated for HAV.
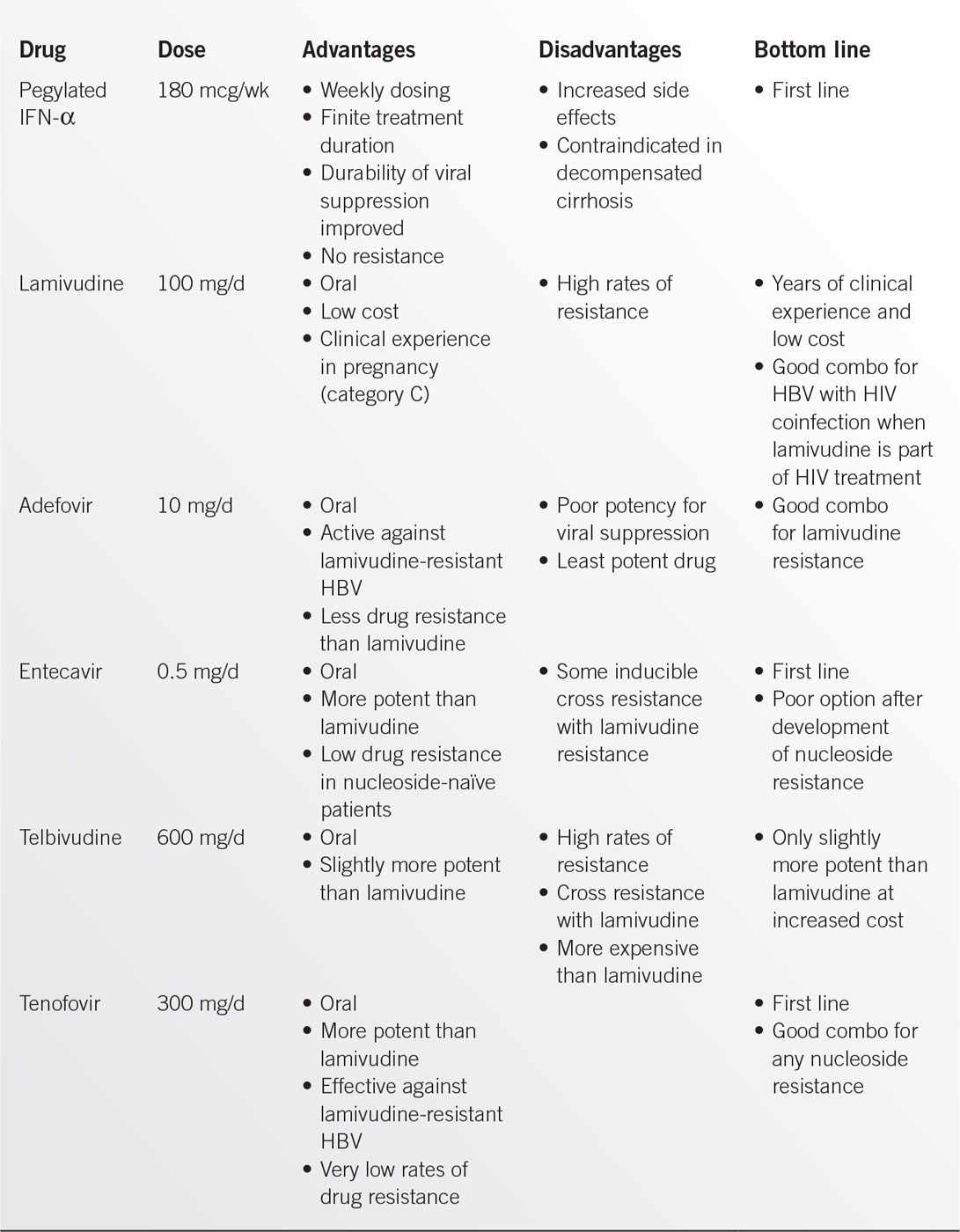
General hepatitis B treatment recommendations include treatment of persons with high levels of HBV DNA in HBeAg-negative infection, active hepatitis ascertained either by very high ALT levels or by biopsy if treatment indications are equivocal, and compensated or decompensated cirrhosis. Management options for chronic HBV include pegylated interferon α-2A (pegIFN), which maintains the best long-term response rates, as well as five other oral antiviral agents that inhibit viral reverse transcriptase. Table 11.5-2 summarizes these available treatment options. Treatment duration with pegIFN lasts 6 to 12 months with monitoring ALT and aspartate aminotransferase for response as well as monitoring complete blood counts. Lamivudine, adefovir, entecavir, tenofovir, and telbivudine comprise the available oral options. Recommended first-line treatment options are for pegIFN, entecavir, and tenofovir.25 Drug treatment typically is no more likely to result in seroconversion than no treatment when ALT levels are less than two times the upper limit of normal (ULN).25 Treatment is generally indicated due to much greater increased risk of liver disease and progression when HBeAg-negative patients with confirmation of sustained, active hepatitis through documentation of elevated ALT levels (>2× ULN) and with HBV DNA greater than 20,000 IU per mL.
Hepatitis C
With acute management of hepatitis C being supportive for the few symptomatic patients who seek medical care during acute infection, treatment of hepatitis C is focused on prevention of liver damage and cirrhosis. Historically, it has been challenging to accurately predict who is at greatest risk for progression to cirrhosis and who would most benefit from treatment, which has not been universally curative nor without risk. Predictors of greater likelihood of treatment response include genotypes 2 and 3, baseline viral load <800,000 IU per mL, Caucasian race, IL28B polymorphisms, and treatment adherence. Proper patient selection with an individualized patient-centered approach has been essential to care.
Historically, the backbone of hepatitis C treatment has been pegylated interferon-α (IFN-α), which is given in a weekly injection, and ribavirin, which is given orally, for 24 to 48 weeks for most patients. These agents inhibit HCV replication. This drug regimen has provided cure rates of 20% to 80% depending on genotype and other host factors. Adverse effects from interferon and ribavirin are common, limiting completion of therapy. A majority of patients develop flu-like symptoms with other common side effects such as anemia, neutropenia, thrombocytopenia, rash, hair loss, thyroid dysfunction, and significant depression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree