Free Functional Muscle Transfers
CASE PRESENTATION
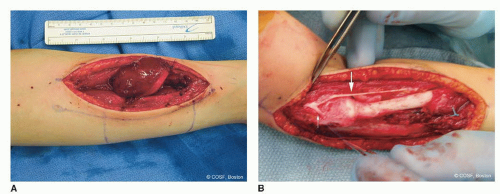
An 18-month-old female presented with an extensile mass of the extensor compartment of her dominant forearm. Her lesion is known by magnetic resonance imaging (MRI) to abut but not involve the posterior interosseous nerve (PIN). There was no bony involvement, and the mass did not extend through the interosseous ligament into the volar compartment. Biopsy confirmed the suspected diagnosis of malignancy, revealing a grade II synovial sarcoma with X:18 translocation. There was no regional node involvement or metastasis by radiographic staging (stage IIA). The patient underwent a primary resection of the extensor carpi radialis brevis and longus, supinator, and a portion of the brachioradialis (Figure 45-1). The PIN was resected beyond the bifurcation of the radial nerve motor and sensory nerves.
CLINICAL QUESTIONS
What are the indications for functional free muscle transfer?
Which muscles are used most often and why?
What are the preoperative requirements to maximize success?
Which nerves are used for reinnervation of the transferred muscle?
What are the indications for myocutaneous flap coverage of the upper limb?
Which muscles are used most frequently?
What are the complications of free muscle transfer?
THE FUNDAMENTALS
The one man team is a complete and total myth.
—Don Shula
The absence of muscle function in a hand or upper limb can be devastating. This can be due to trauma, nerve injuries, compartment syndromes, cancers, and congenital deficiencies. Free muscle transfer is performed when (1) there are no other viable reconstructive options available, such as a regional tendon transfer, and (2) both the recipient site and donor muscle have a reasonable chance of successful functional outcome. Many muscles have been used for functional free muscle transfer with variable success. The best donor muscle for free transfer to the upper limb is the gracilis. The latissimus dorsi, pectoralis major, serratus anterior, and rectus abdominis have been used with less success. Restoration of elbow flexion, finger flexion, and finger extension are the most common functional goals of free muscle surgery, and much less commonly free transfers to the deltoid and triceps. This is complex surgery. Whenever possible, simpler solutions, if available, should be pursued.1,2
Free muscle transfer is also performed for coverage of upper limb major soft tissue deficiencies whenever other less complex treatments (skin grafts, regional or pedicle flaps) are not viable. This is most common after major trauma, oncologic resection, and chronic infection. The gracilis, latissimus dorsi, transverse rectus abdominis (TRAM), and serratus anterior muscles are the usual free musculocutaneous flaps used for coverage in the upper limb. Free tissue transfer surgery is best performed with an outstanding team. Simultaneous harvesting of the donor muscle and preparation of the recipient site lessens anesthesia time, surgeon fatigue, and the most likely patient complications. The optimal team consists of highly skilled nurses and/or midlevel providers, therapists, surgical subspecialists, and cooperative patients and families.
Etiology and Epidemiology
Severe avulsion and rupture injuries of the brachial plexus can result in a poor functional outcome by natural history. Nerve reconstruction by grafting (when there is at least one intact cervical spine nerve root), transfers in the first 1 to 9 months of life, or both are the usual treatment to alter natural history in these infants. When children present late or when nerve surgery fails,3 tendon transfers,4,5 tenodeses,6 and musculoskeletal stabilization procedures are the preferred regional solutions to improve the involved limb function. However, when the injury is so devastating and the donor options are too limited, free muscle transfer
may be indicated.7 This is usually to restore elbow flexion and/or to improve hand function8, 9 and 10 with a functional free gracilis transfer.11 Doi and his team developed the staged double muscle transfer for severe plexus avulsion injuries with (1) free gracilis for elbow flexion and finger extension neurotized by the spinal accessory nerve (SAN) and (2) second free gracilis for finger flexion neurotized by the intercostal nerves (ICNs). This is part of an extensive surgical plan also including sensibility and musculoskeletal stabilization procedures.
may be indicated.7 This is usually to restore elbow flexion and/or to improve hand function8, 9 and 10 with a functional free gracilis transfer.11 Doi and his team developed the staged double muscle transfer for severe plexus avulsion injuries with (1) free gracilis for elbow flexion and finger extension neurotized by the spinal accessory nerve (SAN) and (2) second free gracilis for finger flexion neurotized by the intercostal nerves (ICNs). This is part of an extensive surgical plan also including sensibility and musculoskeletal stabilization procedures.
Volkmann’s ischemic contracture can result in a devastating loss of flexor hand and wrist function. The preferred surgical solution is contracture release and regional transfers if possible (see Chapters 27 and 37). Free gracilis muscle transfer to the digital flexors with neurotization by the anterior interosseous nerve (AIN) is reserved for severe injuries with no other viable options.12 Similarly, there are upper limb malignancy situations, most commonly with rhabdomyosarcoma, in which tumor resection can be followed by free muscle transfer to restore hand or wrist function.13,14
Mangled upper extremities15,16 and severe, chronic osteomyelitis17 in children are also rare clinical scenarios that can respond favorably to free tissue transfer. These procedures are usually for soft tissue coverage but can include composite and functional transfers. Multiple transfers may be necessary. If feasible, this approach is often preferred to a less functional amputation (Figure 45-2).
Clinical Evaluation
The goal of a free muscle transfer is adequate antigravity strength to provide a functional arc of motion and improved use of the hand and upper limb. There must be (1) adequate passive range of motion of involved joints; (2) a recipient artery, vein, and nerve for a viable, functional transfer; (3) sufficient soft tissue coverage for unimpaired tendon and muscle excursion; (4) reasonable hand sensibility and intrinsic strength; (5) balanced antagonistic muscle strength; (6) a highly motivated patient with longterm vision and the ability to wait for functional results; and (7) no better or easier solutions.18 In our practice, this requires a lot of discussion, therapy, and often preliminary surgery to set the stage for a successful outcome. This is not for the faint of heart; weak of will; or impatient child, family, or surgeon. The message needs to be repeated often, the expected outcome made clear, and the patient’s and family’s ability to do the work and be reasonable tested along the way before diving into these procedures. These free muscle transfers are the ultimate “elective” operation. In the end, functional transfer and limb salvage surgery is not magic. If all goes well, the child will be better but not normal in function.
If there is any doubt about the vascularity of the recipient site, an angiogram is obtained. In trauma and oncology situations, this is almost always done. If there is uncertainty about the viability of a nerve donor, exploration and even nerve biopsy is done before donor-site harvesting.
Surgical Indications
It’s not enough that we do our best; sometimes we need to do what’s required.
—Winston Churchill
As discussed in the previous sections of this chapter, it is imperative that all the less complex solutions be considered first and compared against free tissue transfer. Patient selection is critical. Only when all the prerequisites for functional transfer have been met should surgery be
seriously considered. Specifically, free muscle transfers are indicated in the right patient for (1) restoration of elbow flexion (brachial plexopathy); (2) digital flexor function (Volkmann’s ischemic contracture); (3) prehension (brachial plexopathy, after oncologic resection); and (4) digital extension (Volkmann’s ischemic contracture, after oncologic resection).1,19,20 These elective procedures can be successfully performed (95% to 98% flap survival) in the child (even age 2 years or younger).21, 22 and 23
seriously considered. Specifically, free muscle transfers are indicated in the right patient for (1) restoration of elbow flexion (brachial plexopathy); (2) digital flexor function (Volkmann’s ischemic contracture); (3) prehension (brachial plexopathy, after oncologic resection); and (4) digital extension (Volkmann’s ischemic contracture, after oncologic resection).1,19,20 These elective procedures can be successfully performed (95% to 98% flap survival) in the child (even age 2 years or younger).21, 22 and 23
Similarly, free flaps for soft tissue coverage are indicated as a part of limb salvage surgery for major trauma, chronic infection, and oncology care. Again, less complex options must be considered first.24
SURGICAL PROCEDURES
The key is not the “will to win”…everybody has that. It is the will to prepare to win that is important.
—Bobby Knight
The prerequisites for free tissue transfers are a high level of familiarity with the anatomy and performance of these procedures as well as expert microsurgical and hand reconstructive skills. There are no green circle or blue square level procedures here, only black diamond and double black diamond level skill for all members of the team. The thinking and planning part of these procedures strains the
brain. The doing part is very hard (“Why do you think microsurgery is a four-letter word?”) and requires a large treasure chest of expert technical skills. The communicating and doctoring part is critical to your patient’s wellbeing and outcome. You need to build yourself and every member of your team up to an elite level if this is to be a part of your career. If not, find some outstanding professional colleagues to whom you can send these complex patients for the best care possible. And then help with the before and after care.
brain. The doing part is very hard (“Why do you think microsurgery is a four-letter word?”) and requires a large treasure chest of expert technical skills. The communicating and doctoring part is critical to your patient’s wellbeing and outcome. You need to build yourself and every member of your team up to an elite level if this is to be a part of your career. If not, find some outstanding professional colleagues to whom you can send these complex patients for the best care possible. And then help with the before and after care.
For functional free muscle transfers, a suitable donor nerve is essential to a positive outcome. One of the problems with a brachial plexus injury that has been treated with microsurgery is that there may not be adequate donor nerves for late reconstruction with a free muscle. If all reasonable ipsilateral donors were used in the initial microsurgical neural reconstruction, the only alternatives become the contralateral C7, contralateral pectoral, or ipsilateral phrenic. None of these are universally predictable and have been abandoned by most centers. Besides poor nerve surgery outcome with some avulsion injuries in adults, the dearth of donor nerves is one of the reasons that Doi advocated for early free gracilis transfer for elbow flexion and digital extension; the SAN could be used for neurotization without expending it in the initial nerve reconstruction. Similarly, the ICNs can be preserved for later reconstruction of digital flexion, elbow extension, and hand sensibility.25 The best donor nerves are the SAN, ICNs, and the AIN and PIN for elbow and finger function. The gracilis is the best muscle for upper limb functional transfers. It is expendable; has predictable nerve and blood supply; and contours well for elbow flexion, digital flexion, and digital extension. It can be harvested with a skin paddle or covered with a split-thickness skin graft. Its functional excursion usually results in an improved limb.
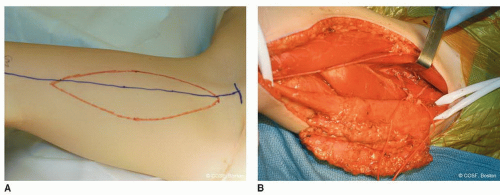 FIGURE 45-3 A: Outline of free gracilis muscle harvest with skin paddle for both coverage and postoperative monitoring. B: Gracilis flap elevation and isolation of neurovascular pedicle to muscle. |
Free Gracilis to Flexor Forearm
The more I practice, the luckier I get.
—Jerry Barber, about golf
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree