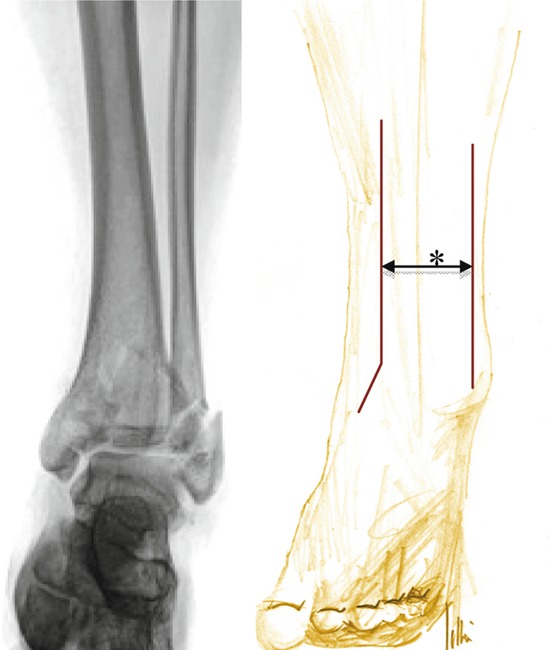
Fig. 27.1
The foot position at the moment of the axial impact. (a) Impartial position (b) dorsiflexion (c) plantarflexion
27.4 Classification
Since the 1960s, several classifications have been developed [9, 17, 21–23, 28]. The classifications of the tibial pilon fractures differentiate intra-articular and extra-articular fractures of the distal tibia. They describe the fracture dislocation and implicate by rising intricacy a higher level of soft-tissue damage.
Rüedi and Allgöwer classification (1968)
Arbeitsgemeinschaft für osteosynthese/orthopaedic trauma association (AO/OTA) classification (1990)
Robinson classification of metaphyseal fractures (1995)
Topliss classification of computed tomography (CT) scans (2004)
Rüedi and Allgöwer described a fracture classification that divides three fractures types, depending on the mechanism: nondisplaced low velocity (Type I), low-energy mildly displaced (Type II), and high-energy comminuted fractures (Type III) [22]. The AO/OTA classification is the most commonly used classification system (Fig. 27.2). Robinson et al. classified the metaphyseal fractures of the distal tibia in order to distinguish these fracture type [21]. They described bending forces (Type I) and torsion mechanisms (Type II).
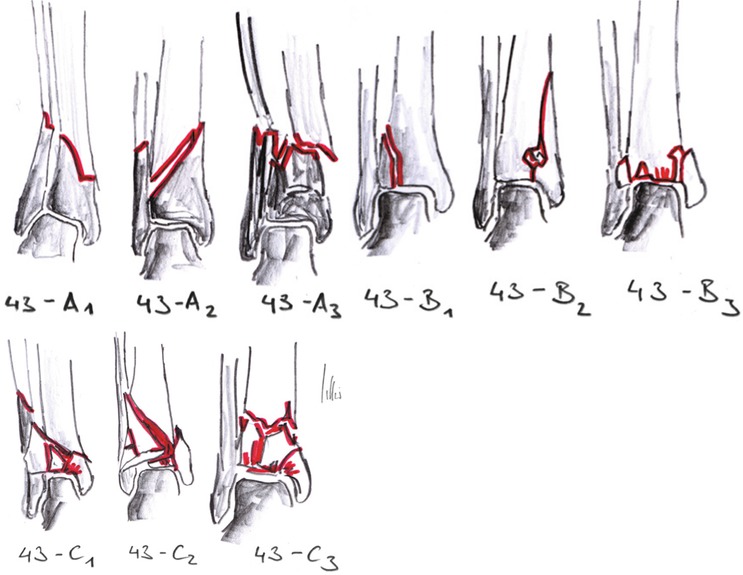
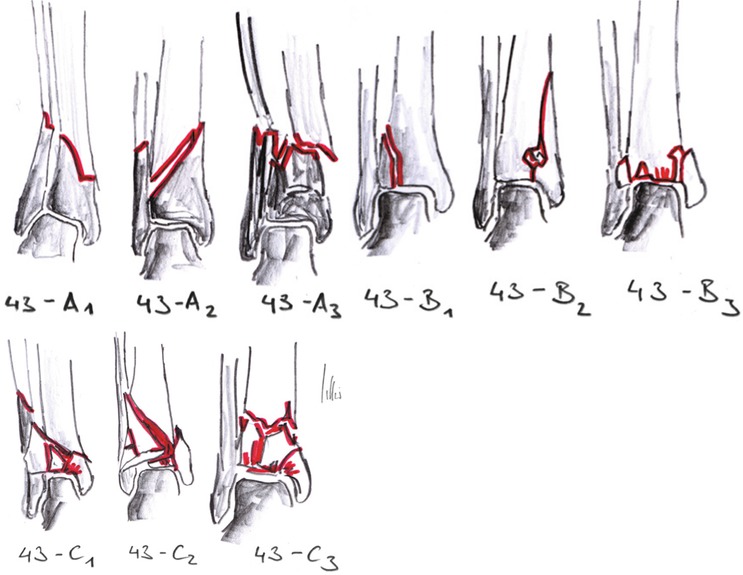
Fig. 27.2
The distal tibia is encoded with the numbers 43 (4 tibia, 3 distal) and additionally specified with the subclassification of extra-articular (Type A), partial articular (Type B), and complete articular fractures (Type C). There are further subgroups of fractures within these classifications, including the degree of dislocation, comminution, and location of fracture lines
Most classifications are developed by plane radiographs. Additionally, the CT scan enables subclassifications for detailed grouping. The plane radiographs (anterior-posterior and mortise view) are necessary for the AO classification. It is also recommended to revise the ankle position after bridging by external fixator. Computed tomography allows for adequate understanding of the fracture morphology and preoperative planning [29]. In CT scans of pilon fractures of the distal tibia, distinct fragments can be recognized [28]. Six different fragments can be distinguished (Fig. 27.3).
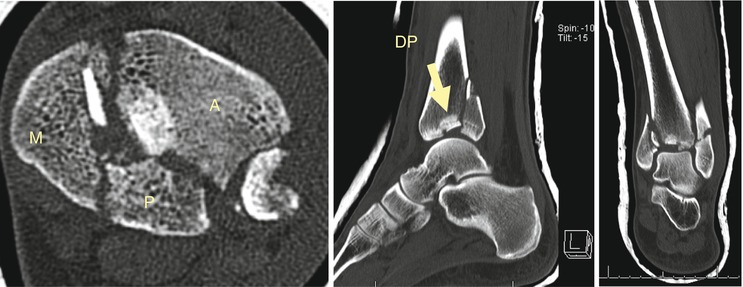
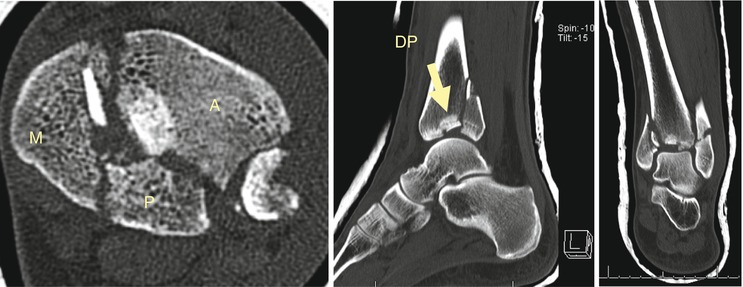
Fig. 27.3
Anterior, posterior, and medial fragments are seen in the CT scan as well as a central articular fragment called a “die-punch” fragment
Anterior fragment (A) – (Tubercule de Tillaux–Chaput)
Posterior fragment (P) – (Posterior malleolus or “Volkman”)
Medial fragment (M)
Antero-lateral fragment (AL)
Posterolateral fragment (PL)
Die-punch fragment (DP)
In addition further kind of fracture patterns in coronal and sagittal planes have been distinguished.
27.5 Diagnostics
Distinction of a low- or high-energy mechanism is important to quantify the degree of soft tissue damage.
27.5.1 Clinical Findings
Soft tissue damage involvement ranges from minor swelling up to early necrosis. Adequate assessment and careful physical examination are needed to estimate the status of the thin soft-tissue envelope. The demarcation of soft-tissue necrosis often takes up to 10 days. Thus, early open reduction and internal fixation of the pilon fractures should be done only in selected cases.
The most important findings are:
Pain and displacement
Soft-tissue breakdown
Fracture blisters (clear to blood filled)
Closed or open fractures
Acute compartment syndrome
Soft tissue injury, associated with closed fractures, is classified by Tscherne and Oestern [30]. They divided the level of injury into four categories. Soft tissue injury, associated with open fractures, is classified by Gustilo and Anderson [12], the standard classification for all open fractures.
27.5.2 Imaging
Preoperative imaging is necessary to allow for careful surgical planning of tibial pilon fractures. The plain radiograph allows an overview of the fracture pattern itself and is required to assure adequate closed reduction. Computed tomography is important to understand all the aspects of the fracture pattern [29]. The following aspects should be examined to allow for adequate surgical planning:
1.
Extension of the fracture:
(a)
Intra- or extra-articular
(b)
Diaphyseal extension (length of osteosynthesis)
(c)
Metaphyseal impaction (need for bone grafting)
2.
Involvement of the medial, lateral, or posterior column
3.
Topography of articular involvement and/or impaction (influence on the surgical approach)
4.
Course of split fracture (approach of the lag screw)
5.
Fracture of the fibula (shortening and rotation)
6.
Soft-tissue involvement (e.g., incorporation of air)
27.6 Associated Injuries
The tibial pilon fractures are often associated with the following injuries:
Fracture of the tarsus
Contralateral limb injury
Neurological deficits
Vascular deficits
Bone and soft-tissue loss
Fracture of the spine and the pelvis
27.7 Management of Treatment
Urgent closed reduction in cases of displacement of the ankle should be performed on an emergent basis. Early stabilization by splinting is necessary to avoid further soft-tissue damage. Depending on the injury pattern and its severity, an urgent surgery with operative reduction and external fixation should be prepared. The main objectives of the initial treatment of tibial pilon fractures are the following:
Acquire axial alignment after closed reduction
Achieve anatomical reduction of the joint surface (ligamentotaxis versus open reduction)
Need for bone grafting in case of impaction or comminuted fractures
Avoid further damage and respect soft-tissue envelope
Avoid superficial or deep infection
Restore joint stability
Pain-free mobility and functionality
In severe cases, a good or excellent result is not attainable because of the high degree of articular involvement.
27.7.1 Nonoperative Management
The treatment of tibial pilon fractures is predominated by the operative procedure. If ligamentotaxis does not reduce the articular fragments, the closed reduction failed and open reduction is indicated after soft-tissue recovery. In case of nondisplaced fractures, such as A1, B1, or C1 AO types, the nonoperative management is feasible. The acceptance of articular fragment displacement is low (gap <2 mm and offset <1 mm tolerated). A close follow-up for secondary displacement is mandatory. Weight bearing should be restricted for 8–10 weeks. Percutaneous or limited open reduction may be combined with cast immobilization. However, if the stability of the reduction is uncertain, an external fixator should be used instead of a cast.
27.7.2 Operative Management
A note of caution: Do not operate through a compromised soft-tissue envelope, particularly in the case of blood-filled blisters in diabetic patients.
27.7.2.1 Open Reduction and Plate Fixation
Rüedi and Allgöwer established the following guidelines [24]:
1.
Open reduction and internal fixation (ORIF) of the fractured fibula
2.
Reconstruction of the articular surface
3.
Bone-graft implantation if necessary
4.
Internal fixation by plate osteosynthesis
These guidelines follow the AO principles of anatomic reduction, rigid stabilization, and early mobilization. The posterolateral approach to the fibula is used for its ORIF (Fig. 27.4). The fibular nerve must be respected. In case of comminuted fracture, a bridging plate is used to ensure the alignment (length, rotation, axis). If the soft-tissue overlying the fibula is compromised, ORIF of the fibula should be delayed. The reconstruction of the articular surface is reached by an anteromedial approach. These articular fragments cannot be reduced by closed reduction and ligamentotaxis. If a two-incision approach is selected, a skin bridge of 7 cm should be maintained (Fig. 27.4). The open reduction of the articular surface often requires bone graft transfer. The following osteosynthesis aims at a sufficient stabilization. Many authors investigated the outcome after this procedure and concluded there were difficulties with wound healing, especially after high-energy trauma. Free tissue transfer was frequently required [7, 16, 27, 31, 33]. Therefore, a staged protocol has evolved over time to improve overall results of this severe injury.