CHAPTER 10 Fractures of the Scapula
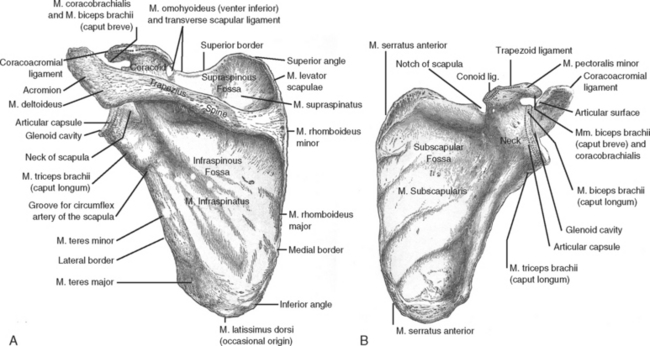
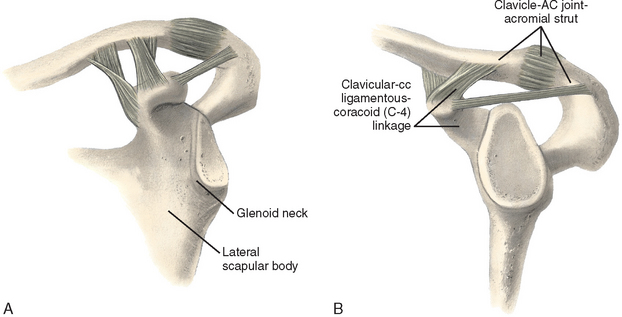
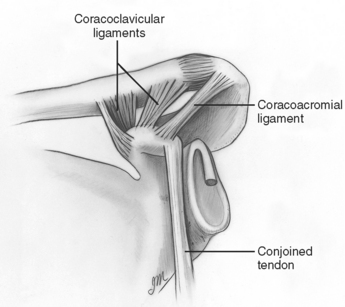
The scapula is quite important to upper extremity function. Lying over the posterior chest wall, it is an integral part of the connection between the upper extremity and the axial skeleton via the glenohumeral and acromioclavicular joints, as well as the sternoclavicular articulation. It functions as a semi-stable, fairly mobile platform for the humeral head and upper extremity to work against. Finally, it serves as a point of attachment for a variety of soft tissue structures (musculotendinous and ligamentous) (Fig. 10-1).
Fractures of the scapula account for 1% of all fractures, 5% of shoulder fractures, and 3% of injuries to the shoulder girdle (Box 10-1). This relative infrequency occurs for two reasons: (1) the scapula lies over the posterior chest wall and is protected by the rib cage and the thoracic cavity anteriorly and a thick layer of soft tissues posteriorly, and (2) the relative mobility of the scapula allows considerable dissipation of traumatic forces. The vast majority of scapula fractures (>90%) are insignificantly displaced, primarily because of the strong support provided by the surrounding soft tissues, thus making nonoperative management the treatment of choice.1 As a result, these injuries have received little attention in the literature. However, scapula fractures involve a major articulation, occur in patients with a mean age of 35 to 45 years, and, when significantly displaced, can cause considerable morbidity. Consequently, these injuries deserve more respect and recently have received more consideration in major texts,2–17 general and review articles, and papers dealing with specific issues.18–39
ANATOMY
Arising from the superior border of the scapula, the coracoid process curves superiorly, anteriorly, and laterally. The brachial plexus and axillary vessels pass medial to the coracoid process and deep to the pectoralis minor tendon. The suprascapular notch is found along the superior scapular border, just medial to the base of the coracoid process, and is bridged by the transverse scapular ligament. The suprascapular nerve courses through the notch beneath the ligament, and the suprascapular artery passes above the ligament. The acromion projects laterally and then anteriorly from the scapular spine. Its junction with the glenoid neck constitutes the spinoglenoid notch, through which the suprascapular nerve and vessels pass from the supraspinatus fossa into the infraspinatus fossa. The dorsal scapular and accessory nerves accompany the deep and superficial branches of the transverse cervical artery, respectively, medial to the vertebral border of the scapula.
CLASSIFICATION OF FRACTURES OF THE SCAPULA
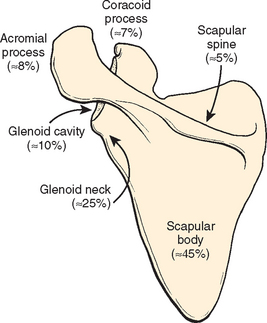
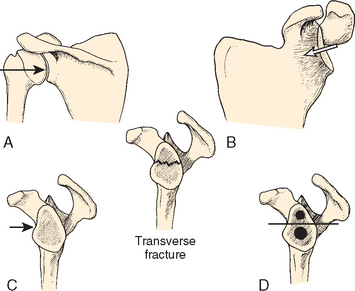
Quite a number of scapula fracture patterns occur. Typically, they are classified by anatomic area: body and spine, glenoid neck, glenoid cavity, acromial process, and coracoid process. Most scapula fractures involve the body and spine (∼50%).27 The remaining 50% involve its three processes (Fig. 10-2).
Fractures of the glenoid neck constitute approximately 25% of the total, and fractures of the glenoid cavity (the glenoid rim and glenoid fossa) make up approximately 10%. Fractures of the glenoid process therefore account for approximately 35% of all scapula fractures. Approximately 8% of these injuries involve the acromial process and approximately 7% involve the coracoid process.27 An acromial fracture is defined as any fracture that runs from the posterior margin of the scapular spine or acromion to the undersurface of the acromial process all the way to the deepest point of the spinoglenoid interval.
A group of injuries termed double disruptions of the superior shoulder suspensory complex (SSSC) also have been described and often involve fractures of the coracoid, acromial, or glenoid processes.40 Avulsion, stress, and fatigue fractures can also occur.
CLINICAL FEATURES
The physician’s attention is initially drawn to the scapular region by the patient’s complaints of pain. Characteristically, the arm is held adducted and all movement is resisted, particularly abduction, which is especially painful. Local tenderness is typical. Abnormal physical findings in the area include swelling and crepitus. Ecchymosis is less than what might be expected given the degree of bony injury. The specific diagnosis of a scapula fracture, however, is ultimately radiographic. These injuries are often initially missed41 or detected incidentally on the patient’s admission chest radiograph (Fig. 10-3). It cannot be overemphasized that scapula fractures are typically accompanied by associated injuries that often require more urgent management.
ASSOCIATED INJURIES AND COMPLICATIONS
The most significant complications associated with scapula fractures are those that result from accompanying injuries to adjacent and distant osseous and soft tissue structures.1,42 Because of the severe traumatic forces involved, these patients have an average of 3.9 additional injuries, with the most common sites being the ipsilateral shoulder girdle,43 upper extremity, lung, and chest wall.44 Twenty-five percent to 45% of patients have accompanying rib fractures, 15% to 40% have fractures of the clavicle, 15% to 55% have pulmonary injuries45 (e.g., hemopneumothorax, pulmonary contusion), 12% have humeral fractures, and 5% to 10% sustain injuries to the brachial plexus and peripheral nerves.46–48 Fractures of the skull are found in approximately 25% of patients, cerebral contusions in 10% to 40%, central neurologic deficits in 5%, tibia and fibula fractures in 11%,48–50 major vascular injuries in 11%, and injuries that result in splenectomy in 8%. Two percent of these patients die. Landi and colleagues have described a compartment syndrome associated with a scapula fracture.51 A variety of other cardiothoracic, genitourinary, and gastrointestinal injuries have also been reported. Interestingly, Stephens and associates reviewed 173 blunt trauma patients (92 with scapula fractures and 81 controls) and concluded that scapula fractures are not a significant marker for greater mortality or neurovascular morbidity.52 Veysi and colleagues also showed no increase in mortality, but they did confirm significantly greater severity scores in trauma patients sustaining scapula fractures.53
RADIOGRAPHIC EVALUATION
A fracture of the scapula is an x-ray diagnosis, but precisely defining the injury can be difficult. If a scapula fracture is suspected or noted on other radiographs, a scapula trauma series is indicated, including true anteroposterior (AP) and lateral views of the scapula, as well as a true axillary projection of the glenohumeral joint (Fig. 10-4 and Box 10-2).
Box 10-2 Radiographic Evaluation of the Scapula
Often detected incidentally on chest radiograph
CT with and without reconstructions
If an injury to the SSSC (the linkage system between the clavicle and the scapula) is suspected (e.g., a disruption of the coracoclavicular and/or acromioclavicular ligaments), a weight-bearing AP film is obtained (see Fig. 10-4). In some situations, transthoracic lateral and oblique projections of the region may be of value. The scapula trauma series should suffice for most injuries.
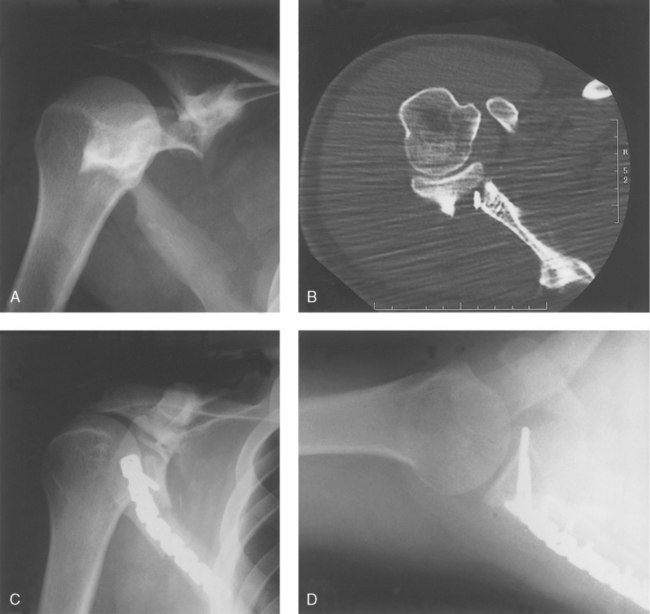
If the fracture pattern appears to be complex (multiple fracture lines and significant displacement), computed tomography (CT) scanning is necessary. Images in the superior plane allow evaluation of the acromioclavicular joint and acromial process, whereas the inferior images allow visualization of the scapular body and spine and the scapulothoracic articulation (Fig. 10-5). The middle images allow one to see the glenoid neck, the glenoid cavity (glenoid rim and glenoid fossa), the coracoid process, and the glenohumeral articulation (Fig. 10-6). In certain clinical situations, reconstructed views can be of great value. The proximal part of the humerus can be eliminated for optimal visualization of the glenoid cavity, and other reconstructed images are also possible (Fig. 10-7). Three-dimensional (3D) scanning can be extremely helpful to an orthopaedist trying to evaluate the most complex fracture patterns (Fig. 10-8). Images rotated at 15-degree increments in the horizontal, vertical, and oblique planes can be examined and the most useful printed for later reference. McAdams and colleagues found that CT scanning did not improve the evaluation of glenoid fractures over plain films but did help in identifying associated injuries to the SSSC.54
The exact role, if any, of arthroscopy (both diagnostic and therapeutic) is yet to be defined.
TYPES OF FRACTURES AND METHODS OF TREATMENT
Glenoid Neck (Extra-articular) Fractures
Fractures of the glenoid neck make up 25% of all scapula fractures (Box 10-3). It is somewhat surprising that these injuries are not more common because this portion ofthe glenoid process is quite narrow. These fractures may be caused by the following:
Box 10-3 Significantly Displaced Glenoid Neck Fractures
Translational displacement of ≥1 cm
Angular displacement of ≥40 degrees
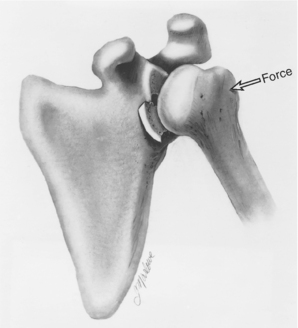
The glenoid neck is that portion of the glenoid process which lies between the scapular body and the glenoid cavity. The coracoid process arises from its superior aspect. Its stability is primarily osseous—specifically, its junction medially with the scapular body. Secondary support is provided by its attachments superiorly to the clavicular—acromioclavicular joint—acromial strut via the clavicular—coracoclavicular ligamentous—coracoid (C-4) linkage and the coracoacromial ligament (Fig. 10-9). Tertiary soft tissue support is provided anteriorly by the subscapularis muscle, superiorly by the supraspinatus muscle, and posteriorly by the infraspinatus and teres minor muscles.
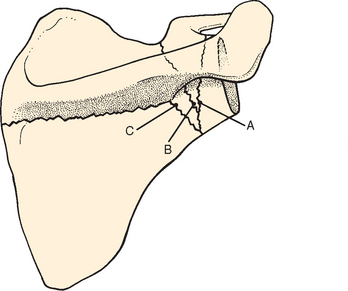
To be a glenoid neck fracture, the disruption must be complete: exiting along the lateral scapular border and the superior scapular margin, either just lateral or justmedial to the coracoid process (Fig. 10-10). Displacement can then occur. If, in addition, its secondary support is compromised (a coracoid process fracture, a coracoclavicular ligament disruption with or without a coracoacromial ligament injury, a clavicle fracture, an acromioclavicular joint disruption, or an acromial fracture; i.e., a double disruption of the SSSC), the fracture has the potential for severe displacement.55 Hardegger and coauthors56 described a rare case in which the fracture line exited the superior scapular border lateral to the coracoid process (the anatomic neck) (see Fig. 10-10), thereby allowing the glenoid fragment to be displaced laterally and distally by the pull of the long head of the triceps muscle. Arts and Louette57 described a similar injury. They saw these fractures as inherently unstable (the primary support is completely disrupted and the fracture is lateral to the secondary support system) and in need of open reduction and internal fixation (ORIF), as opposed to fractures of the surgical neck, which require associated injuries to their secondary support system to be rendered unstable and in need of surgical management.
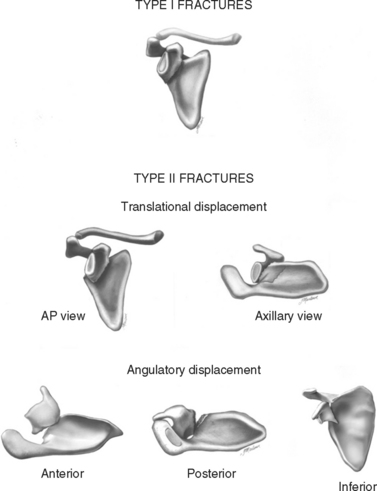
Type I fractures include all insignificantly displaced injuries and constitute more than 90% of the total. Management is nonoperative, and a good to excellent functional result can be expected. Type II fractures include all significantly displaced injuries; significant displacement is defined as translational displacement of the glenoid fragment of 1 cm or more or angular displacement of the fragment of at least 40 degrees (Fig. 10-11).58 Limb and McMurray described the case of a patient with a glenoid neck fracture so severely displaced and inferiorly angulated that the humeral head was articulatingwith the medial fracture surface and lateral margin of the scapular body rather than the glenoid fragment.59 Translational displacement of 1 cm was chosen by Zdravkovic and Damholt,60 Nordqvist and Petersson,61 and Miller and Ada62,63 as separating major from minor injuries. Bateman2 stated that this degree of displacement could interfere with abduction.
Hardegger and coworkers56 pointed out that significant translational displacement changes the normal relationships between the glenohumeral articulation and the undersurface of the distal end of the clavicle, the acromioclavicular joint, and the acromial process. This alters the mechanics of nearby musculotendinous units, resulting in a functional imbalance of the shoulder complex as a whole (a disorganization of the coracoacromial arch). Miller and Ada62,63 stated that the resultant weakness (especially abductor weakness), decreased range of motion, and pain (particularly subacromial pain) were largely due to rotator cuff dysfunction. The premise that significant translational displacement of the glenoid process can lead to shoulder discomfort and dysfunction certainly makes sense intuitively. The complex bony relationships in the glenohumeral region are clearly altered, as are the mechanics of the musculotendinous structures that pass from the scapula to the proximal part of the humerus (the deltoid muscle and rotator cuff, in particular). The fracture line usually exits the superior scapular margin medial to the coracoid process (the surgical neck region). The glenoid fragment is then drawn inferiorly by the weight of the arm and either anteromedially or posteromedially by the adjacent muscle forces (Fig. 10-12). (Van Noort and van der Werken think that the scapular body is displaced laterally rather than the glenoid fragment displaced medially).64
Bateman2 and DePalma65 stated that excessive angulation of the glenoid fragment could result in glenohumeral instability (anterior, posterior, or inferior). Normally, the glenoid cavity faces 15 degrees superiorly and is retroverted 6 degrees relative to the plane of the scapular body. With increasing angulation, the humeral head loses the normal bony support provided by the glenoid cavity (bony instability), which translates into glenohumeral discomfort and dysfunction.2,5,62,63 Miller and Ada62,63 stated that angular displacement of 40 degrees or more in either the coronal or sagittal plane was unacceptable. They saw this degree of displacement as adversely altering not only glenohumeral but also other bony relationships, as well as musculotendinous dynamics, particularly those of the rotator cuff, with resultant pain and overall shoulder dysfunction (diminished range of motion and loss of strength) (Fig. 10-13). Van Noort and van Kampen recommended surgical management for glenoid neck fractures with inferior angulation greater than 20 degrees (4 degrees of superior angulation being the mean in normal persons).66
Imatani,24 McGahan and associates,27 and Lindholm and Leven67 recommended nonsurgical treatment of all glenoid neck fractures, but their studies give few details to justify this conclusion. Although somewhat ambivalent in their recommendations, two studies do mention surgical management as an option in selected cases. Armstrong and Vanderspuy68 said that although most of these injuries do well, more aggressive treatment, including ORIF, may be indicated in patients who are young and fit. Wilbur and Evans36 stated that ORIF might be indicated if the glenoid fragment is markedly displaced or angulated but did not think that they had enough information or experience to warrant definitive surgical indications. Judet,69 Magerl,70 Ganz and Noesberger,71 and Tscherne and Christ72 said that operative management of displaced glenoid neck fractures prevents late disability and yields better results. Neer,9 as well as Rockwood10 and Butters,3 presented the recommendations of other investigators, as did a review article by Guttentag and Rechtine.22 Boerger and Limb73 reported the case of a patient with a fracture of the glenoid neck, acromial and coracoid fractures, a dislocated acromioclavicular joint, and incomplete paralysis of the infraspinatus muscle treated with ORIF of the acromial and glenoid neck fractures. DeBeer and colleagues described the operative treatment of a professional cyclist who was able to return to competition after 6 weeks and urged more aggressive management in high-demand patients.74
Bozkurt and colleagues reported on 18 patients treated nonoperatively and found that decreased functional outcome correlated significantly with increased inferior angulation of the fracture and the presence of associated injuries.75 Van Noort and van Kampen managed 13 patients without significant angular displacement, neurologic injury, and associated ipsilateral shoulder injuries, all of whom had a good to excellent outcome regardless of the degree of translational displacement when treated nonoperatively.66
Miller and Ada62,63 retrospectively reviewed 16 displaced glenoid neck fractures (≥1 cm of translational displacement or ≥40 degrees of angulation) managed nonoperatively (36-month average follow-up). They found that 20% had decreased range of motion, 50% had pain (75% of which was night pain), 40% had weakness with exertion, and 25% noted popping. In particular, these patients often had shoulder abductor weakness and subacromial pain that was due at least in part to rotator cuff dysfunction. They recommended ORIF of glenoid neck fractures with this degree of displacement. Chadwick and colleagues agreed.77
Pace and colleagues reviewed 9 patients with insignificantly displaced fractures and found the majority had some activity-related pain that was believed to be due to impingement and cuff arthropathy despite 90% good to excellent results.78 A long-term follow-up study by Zdravkovic and Damholt60 included 20 to 30 patients (it is difficult to determine the exact number from the text) with displaced glenoid neck fractures and noted that nonoperative treatment yielded satisfactory results. Nordqvist and Petersson61 evaluated 37 glenoid neck fractures treated without surgery (10- to 20-year follow-up) and found the functional result to be either fair or poor in 32%. They said that for some fractures, early ORIF might have improved the result. Hardegger and coauthors56 reported 80% good to excellent results in five displaced glenoid neck fractures treated surgically (6.5-year follow-up). They said that operative management of such injuries prevented late disability and yielded betterresults. Gagey and colleagues79 found a good result in only 1 of 12 displaced fractures treated nonoperatively. They stated that such injuries could “disorganize the coracoacromial arch” and recommended ORIF.
The diagnosis is ultimately radiographic. Plain radiographs are helpful, but because of the complex bony anatomy in the area, CT scanning is generally necessary to decide whether a glenoid neck fracture is indeed complete, to determine the degree of displacement, if any, and to identify injuries to adjacent bony structures and articulations.54 One must not confuse these injuries with the more common fractures that course through the inferior glenoid neck and the scapular body (see Fig. 10-10). CT scanning readily reveals that the latter are not complete disruptions of the glenoid process because the superior aspect of the glenoid neck is intact. These injuries are essentially fractures of the scapular body and do quite well with nonoperative care because the normal relationships between the glenohumeral articulation and the distal end of the clavicle acromion are unaltered (Fig. 10-14).80 Finally, if an injury to the SSSC (the clavicular—scapular linkage) is suspected, a weight-bearing AP view of the shoulder is obtained.
Glenoid Cavity (Intra-articular) Fractures
Fractures of the glenoid cavity make up 10% of scapula fractures. The majority (>90%) are insignificantly displaced and are managed nonoperatively (Fig. 10-15 and Box 10-4). Significantly displaced fractures require surgical treatment or at least merit surgical consideration. Ideberg reviewed more than 300 such injuries and proposed the first detailed classification scheme,43,81,82 which was subsequently expanded by Goss (Fig. 10-16).83 Type I fractures involve the glenoid rim: type Ia, the anterior rim; and type Ib, the posterior rim. Fractures of the glenoid fossa make up types II to V. Type VI fractures include all comminuted injuries (more than two glenoid cavity fragments).
FIGURE 10-15 AP radiograph showing an undisplaced fracture of the scapula involving the glenoid process.
(From Goss TP: Fractures of the scapula: Diagnosis and treatment. In Iannotti JP, Williams GR Jr [eds]: Disorders of the Shoulder: Diagnosis and Management. Philadelphia: Lippincott Williams & Wilkins, 1999, p 603.)
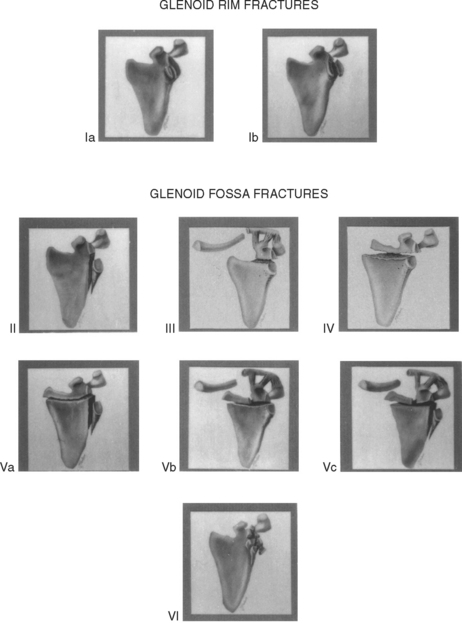
FIGURE 10-16 Goss—Ideberg classification scheme for fractures of the glenoid cavity.
(From Goss TP: Fractures of the glenoid cavity [Current Concepts Review]. J Bone Joint Surg Am 74[2]:299-305, 1992.)
Fractures of the glenoid rim occur when the humeral head strikes the periphery of the glenoid cavity with considerable violence (Fig. 10-17).84 These injuries are true fractures, distinct from the small avulsion injuries that occur when a dislocating humeral head applies a tensile force to the periarticular soft tissues.65 A true axillary view of the glenohumeral joint, CT imaging (routine and reconstructive), and, if necessary, 3D scanning allow one to determine the size and displacement of the rim fragment, whether persistent subluxation of the humeral head is present, and therefore whether stability of the glenohumeral articulation is significantly compromised (Figs. 10-18 and 10-19).
Once a transverse disruption occurs, the fracture can propagate in a variety of directions, depending on the exact direction of the humeral head force. An AP pro- jection of the glenohumeral joint, reconstructed CT images in the coronal plane, and even 3D CT scanningmay be necessary to accurately determine whether and to what degree articular incongruity, separation, or both are present. If an injury to the SSSC (the scapular—clavicular linkage) is suspected, a weight-bearing AP view of the shoulder is obtained.
Type I
Surgical management of fractures of the glenoid rim is indicated if the fracture results in persistent subluxation of the humeral head (failure of the humeral head to lie concentrically within the glenoid cavity) or if the fracture or humeral head is unstable after reduction. DePalma65 stated that instability could be expected if the fracture is displaced 10 mm or more and if a quarter or more of the glenoid cavity anteriorly or a third or more of the glenoid cavity posteriorly is involved. Hardegger and coworkers56 concurred and stated that operative reduction plus fixation of the fragment is indicated to prevent recurrent or permanent dislocation of the shoulder. Guttentag and Rechtine22 and Butters3 agreed with these recommendations. Several papers describing operative management of glenoid rim fractures have also appeared in the literature.85–89 Surgery, if necessary, is designed to restore articular stability and prevent post-traumatic degenerative joint disease (Fig. 10-21).
Type II
With type II glenoid fossa fractures, the humeral head is driven inferiorly and an inferior glenoid fragment is created. Surgery is indicated if an articular step-off of 5 mm or more is present or if the fragment is displaced inferiorly and carries the humeral head with it such that the humeral head fails to lie in the center of the glenoid cavity (Fig. 10-22). These injuries can result in post- traumatic degenerative joint disease or glenohumeral instability, or both.90
Type III
Type III (glenoid fossa) fractures occur when the force of the humeral head is directed superiorly and causes the transverse disruption to propagate upward, generally exiting through the superior scapular margin in the vicinity of the suprascapular notch.91,92 One might question whether this is a fracture of the glenoid cavity or a fracture of the coracoid process because the superior third of the glenoid cavity and the base of the coracoid process are formed from the same ossification center. Displacement is usually minimal, with the fragment lying medially. Consequently, as with base of the coracoid fractures, these injuries are generally treated nonoperatively and heal uneventfully.
Any glenoid cavity fracture may be associated with neurovascular injury due to the proximity of the brachial plexus and axillary vessels, as well as the considerable violence involved. Type III injuries, as well as Type Vb, Vc, and VI injuries, however, are particularly prone tosuch neurovascular involvement, especially if the superiorly directed force continues further upward and damages the SSSC—that is, if there is an associated disruption of the C-4 linkage or the clavicular—acromioclavicular joint—acromial strut. Neer and Rockwood considered compression of the adjacent neurovascular structures by these and fractures of the coracoid process indications for surgery.10 They and others also described the occurrence of suprascapular nerve paralysis associated with fractures involving the coracoid process and the glenoid neck that extend into the suprascapular notch (electromyographic [EMG] testing was essential to make the diagnosis, and early exploration was recommended).4,93–94
Surgical management of type III fractures is indicated if the fracture has an articular step-off of 5 mm or more with lateral displacement of the superior fragment or if a significantly displaced additional disruption of the SSSC is present (a double disruption injury) (Fig. 10-23). Examples include an associated disruption of the C-4 linkage or of the clavicular—acromioclavicular joint—acromial strut.55 These injuries can result in post-traumatic degenerative joint disease and severe functional impairment.
Type IV
Type IV (glenoid fossa) injuries occur when the humeral head is driven directly into the center of the glenoid cavity.95 The fracture courses transversely across the entire scapula and exits along its vertebral border. If there is an unacceptable articular step-off (≥5 mm) with the superior fragment displaced laterally, or if the superior and inferior glenoscapular segments are severely separated, ORIF is indicated to prevent symptomatic degenerative joint disease, nonunion at the fracture site (an extremely rare occurrence but a definite concern in the case shown [Fig. 10-24]), and instability of the glenohumeral joint. Ferraz and colleagues described a Type IV glenoid fossa fracture that progressed to a nonunion. When explored surgically less than 2 years after injury, a 7 mm articular step-off was noted as well as grade III cartilaginous erosion of the humeral head.96
Type V
These glenoid fossa injuries are combinations of type II, III, and IV injuries and are caused by more violent and complex forces. The same clinical concerns and operative indications detailed for the type II, III, and IV fractures apply to type V fractures (Fig. 10-25).
Type VI
Reports by Aulicino and coauthors97 and Aston and Gregory85 lend support to the role of surgery in managing significantly displaced glenoid fossa fractures. Lee and colleagues98 reported the case of a child who sustaineda type II fracture that required ORIF. Ruedi and Chapman15 stated that “grossly displaced intra-articular fractures of the glenoid that render the joint incongruent and unstable profit from operative reconstruction and internal fixation as incongruities result in osteoarthritic changes.” Rowe14 advocated surgical management of severely displaced injuries. Bauer and coworkers99 reviewed 20 patients treated surgically for significantly displaced fractures of the scapula (6.1-year average follow-up) and reported greater than 70% good or very good results based on the Constant score. They recommended early ORIF for grossly displaced fractures of the glenoid fossa, glenoid rim, glenoid neck, and coracoid and acromial processes. Hardegger and associates56 reported that if “there is significant displacement, conservative treatment alone cannot restore congruency,” and stiffness and pain can result—“for this reason open reduction and stabilization are indicated.”
Kavanagh and colleagues100 presented their experience at the Mayo Clinic in which 10 displaced intra-articular fractures of the glenoid cavity were treated with ORIF. They found ORIF to be “a useful and safe technique” that “can restore excellent function of the shoulder.” In their series, the major articular fragments were displaced 4 to 8 mm. The authors emphasized that they remained uncertain how much incongruity of the glenoid articular surface can be accepted without risking the long-term sequelae of pain, stiffness, and traumatic osteoarthritis. Soslowsky and coworkers101 found the maximal depth of the glenoid articular cartilage to be 5 mm. Consequently, if a glenoid fossa fracture is associated with an articular step-off of 5 mm or more, subchondral bone is exposed. Schandelmaier and coauthors102 reported a series of 22 fractures of the glenoid fossa treated with ORIF. They stated that “if the postoperative courses are uneventful, excellent to good results can be expected.” Leung and colleagues103 reviewed 14 displaced intra-articular fractures of the glenoid treated with ORIF (30.5-year average follow-up) and reported nine excellent and five good results.
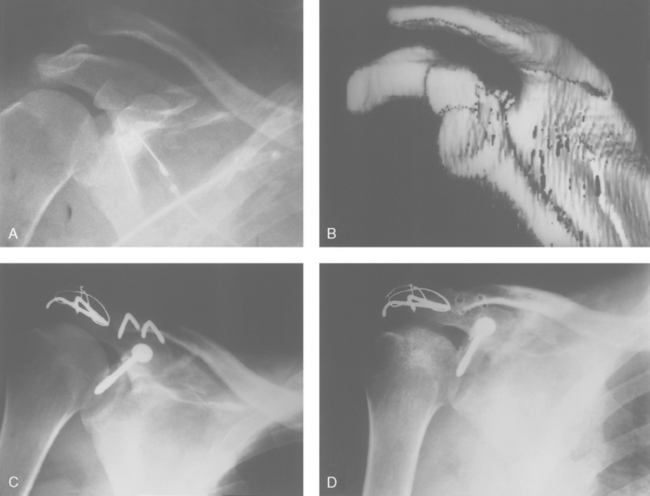
Fractures of the Scapular Body
These injuries are often rather alarming radiographically: Extensive comminution and displacement are often present (Fig. 10-26). However, there is very little enthusiasm in the literature for operative treatment104 because bone stock for fixation is at a premium and these injuries seem to heal quite nicely with nonoperative or symptomatic care,105 and a good to excellent functional result can be expected. The vast majority of fractures of the scapular body and insignificantly displaced fractures (>90% of glenoid, coracoid, acromial, and avulsion fractures) are managed nonoperatively.

FIGURE 10-26 AP radiograph showing a severely comminuted fracture of the scapular body.
(From Neer CS II: Less frequent procedures. In Neer CS II [ed]: Shoulder Reconstruction. Philadelphia: WB Saunders, 1990, pp 421-485.)
This prognosis is positive probably because the scapulothoracic interval is cushioned by a thick layer of soft tissues and the mobility of the scapulothoracic articulation compensates for most residual deformities of the scapular body. The literature does mention a fracture of the scapular body with a lateral spike entering the glenohumeral joint as an indication (albeit extremely uncommon) for surgical management,56 and a similar recommendation was made in two cases involving patients with fractures of the scapular body and intrathoracic penetration by one of the fragments.106,107 Bowen and colleagues reported a case of a significantly angulated greenstick fracture of the scapular body that required a closed reduction.108 On rare occasions, malunion of a scapular body fracture can result in scapulothoracic pain and crepitus requiring surgical exposure of its ventral surface and removal of the responsible bony pro- minence or prominences.109 Nonunion of a scapular body fracture requiring surgical management has been described.96,110–112
Fractures of the scapular body and spine, as well as insignificantly displaced fractures of the glenoid, acromial, and coracoid processes, are managed nonoperatively. These patients are initially placed in a sling and swathe immobilizer for comfort. Local ice packs to the affected area are helpful during the first 48 hours, followed by moist heat thereafter. Analgesic medications are prescribed as needed. Absolute immobilization is generally short (48 hours), but it can continue for up to 14 days, depending on the clinical situation. The patient is then permitted to gradually increase the functional use of the upper extremity as symptoms allow, and sling and swathe protection is gradually decreased until the 6-week point.
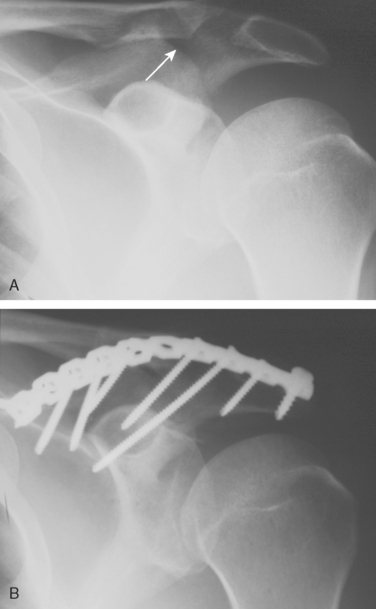
Isolated Acromial Fractures
Acromial fractures may be caused by a direct blow from the outside or a force transmitted via the humeral head. Avulsion fractures are the result of purely indirect forces occurring where musculotendinous or ligamentous structures (the deltoid and trapezius muscles as well as the coracoacromial and acromioclavicular ligaments) attach to the acromion. Even stress and fatigue fractures have been reported.113,114 These injuries may be minimally or significantly displaced.115 Kuhn and colleagues proposed a classification scheme that drew some discussion.116–119 They emphasized the need for ORIF if an acromial fragment is displaced inferiorly by the pull of the deltoid muscle and is compromising the subacromial space, thereby resulting in impingement symptoms and interfering with rotator cuff function.120
The diagnosis is radiographic. True AP and lateral views of the scapula and a true axillary projection of the glenohumeral joint detect most acromial fractures. An os acromiale can complicate the evaluation. On occasion, however, CT scanning may be needed to precisely define the injury and disclose involvement of adjacent bony and articular structures. A weight-bearing AP projection is obtained if disruption of the scapular—clavicular linkage (SSSC) is suspected. Arthrography to evaluate the rotator cuff is considered if an acromial fracture is the result of traumatic superior displacement of the humeral head or chronic superior migration of the proximal humerus as seen in long-standing rotator cuff disease (e.g., cuff tear arthropathy with a stress fracture of the acromion). Madhavan and coauthors121 described a case in which an acromial fracture was associated with an avulsed subscapularis tendon.
Although significantly displaced, isolated, nonavulsion acromial fractures have been described,122,123 the vast majority are nondisplaced or minimally displaced. Symptomatic nonoperative care reliably led to union and a good to excellent functional result. Significantly displaced injuries, however, require surgical management. Symptomatic acromial nonunion, although uncommon, has been reported in the literature.124–126 No more than a small fragment should ever be excised.127 The presence of a large fragment requires surgical stabilization and bone grafting (Fig. 10-27).
Isolated Coracoid Fractures
The coracoid process develops from two constant ossification centers: one at its base, which also forms the upper third of the glenoid process, and one that becomes its main body. In addition, it has at least two inconstant centers: one at its angle where the coracoclavicular ligament attaches and one at its tip where the conjoined tendon is located. The regions at which the centers finally unite are relatively weak, especially in young adults, thus making fractures more likely to occur when direct or indirect forces are applied.128,129
Coracoid fractures may be caused by a blow from the outside130 or contact by a dislocating humeral head or by indirect forces applied through the musculotendinous and ligamentous structures at their attachment sites (avulsion fractures fall into this category).131–134 Fatigue fractures have also been described.135,136 Other causes include fractures associated with coracoclavicular tape fixation used in acromioclavicular joint reconstructions137 and fractures associated with massive rotator cuff tears. Despite the relative scarcity of isolated coracoid fractures, several types have been described.91,127 These injuries can be anatomically divided into the following categories:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree