I. Fractures of the Distal Radius
A. Overview—Fractures of the distal radius are the most common fractures of the upper extremity, representing 17% of all fractures treated each year. Although they are seen most frequently among older women (ages 60 to 70), young adults make up a significant portion of cases. For those patients older than 60 years of age, almost 70% will have significant osteoporosis of the hip or spine. High-energy injuries resulting in complex fracture patterns have led to the development of newer treatment modalities. Residual articular incongruity greater than 2 mm leads to posttraumatic arthritis in most, if not all, patients. As a result, traditional methods of nonoperative treatment of high-energy injuries have been abandoned in favor of surgical techniques that restore articular anatomic structures.
B. Mechanism of Injury—Approximately 90% of all distal-radius fractures are caused by compressive loading on the dorsiflexed wrist. The degree of comminution is proportional to the energy transferred to the bone, with high-energy injuries causing more comminution and increasingly complex fracture patterns.
C. Anatomy
1. Bony anatomy
• Distal radius—The distal radius is composed of three concave articular surfaces: scaphoid fossa, lunate fossa, and sigmoid notch (Fig. 23-1).
• Articulation between the distal radius and the ulna—The articulation between the distal radius and the ulna occurs at the sigmoid notch, forming the distal radioulnar joint (DRUJ) and allowing forearm rotation.
• Triangular fibrocartilage complex (TFCC)—The TFCC has multiple attachments to the ulna and carpus and may be injured in combination with a distal radius fracture (see later section on the DRUJ).
• Biomechanics—The radius normally carries 80% of the axial load across the wrist. This percentage may change after fracture if there is radial shortening or dorsal tilt of the radial articular surface. As fracture deformity increases, greater loads are shifted to the ulnar side of the wrist. A dorsal tilt of 30° results in 50% load transmission to the ulna.
• Wrist range of motion—Normal ranges of motion of the wrist joint are as follows: dorsiflexion, up to 80°; palmar flexion, up to 85°; radial deviation, up to 25°; ulnar deviation, up to 35°; and pronation/supination, up to 90°. These ranges often decrease after injury as a result of fracture deformity, prolonged immobilization, or both.
2. Ligamentous anatomy—The extrinsic ligaments of the wrist stabilize the carpus to the distal radius and ulna. The intrinsic ligaments of the wrist link the individual carpal bones and are discussed later in this chapter.
• Volar ligaments—The volar extrinsic ligaments are stronger and clinically more important. They include the radioscaphocapitate (RSC), long radiolunate (LRL), short radiolunate (SRL), ulnolunate (UL), and ulnotriquetral (UT) ligaments (Fig. 23-2). The radioscapholunate ligament (ligament of Testut) is now believed to be a neurovascular pedicle and does not provide ligamentous support.
• Dorsal ligaments—The dorsal extrinsic ligaments are less well defined and include the dorsal radiocarpal (DRC) and dorsal intercarpal (DIC) ligaments (Fig. 23-3). Because they are less well defined, they are not very effective at restoring palmar tilt during fracture reduction (by ligamentotaxis).
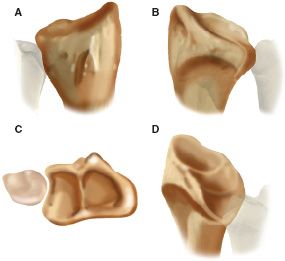
FIGURE 23-1 Distal radius. A. Dorsal view of Lister’s tubercle. B. Palmar view of the scaphoid and lunate fossae distally as well as the sigmoid notch ulnarly. Vascular foramina can be noted on the palmar and dorsal aspects of the distal radius. C. End-on view of the distal radius and radioulnar joint showing the scaphoid fossa, lunate fossa, and ulnar head resting in the sigmoid notch. D. Sigmoid notch from the ulnar aspect.
• Triangular fibrocartilage (TFC)—The TFC attaches to the carpus through the volar UT and UL ligaments (see Fig. 23-2). The TFC with its accompanying attachments is called the TFCC.
3. Radiographic measurements (Fig. 23-4)—Radiographic measurements are important in assessing fracture reduction and residual deformity.
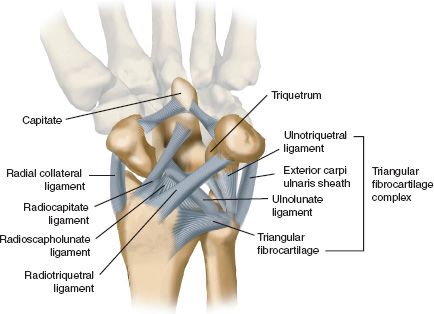
FIGURE 23-2 Volar extrinsic ligaments of the wrist.
• Radial inclination—The normal range is 15° to 30°; the average is 23° (posteroanterior [PA] view).
• Radial length—The normal range is 11 to 12 mm; the average is 12 mm (PA view).
• Volar tilt—The normal range is up to 20°; the average is 11° (lateral view).
D. Classification of Fractures
1. Common eponyms—Although eponyms are imprecise, they continue to be used by orthopaedists to describe distal radius fractures.
• Colles’ fracture (Colles, 1814)—Colles’ fracture is typically extra-articular with dorsal comminution, dorsal displacement, and radial shortening (Fig. 23-5).
• Smith’s fracture (Smith, 1847)—Smith’s fracture is a “reverse Colles’ fracture” with volar displacement. There are three types: Types I, II, and III (Fig. 23-6).
• Barton’s fracture (Barton, 1838)—Barton’s fracture is an intra-articular fracture (a fracture-dislocation of the wrist). These fractures can be volar or dorsal and are usually unstable (see Fig. 23-6). (A Smith Type II fracture is the same as a volar Barton’s fracture.)
• Chauffeur’s fracture (Edwards, 1910)—A Chauffeur’s fracture is an intra-articular fracture of the radial styloid. It may be associated with disruption of the scapholunate ligament (Fig. 23-7).
• Die-Punch (Lunate Load) fracture (Rutherford, 1891; Scheck, 1962)—A die-punch fracture is an intra-articular depression fracture of the lunate fossa of the distal radius (Fig. 23-7).
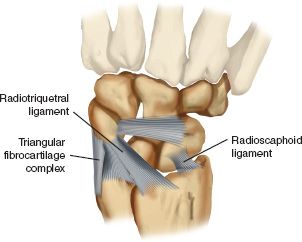
FIGURE 23-3 Dorsal extrinsic ligaments of the wrist.
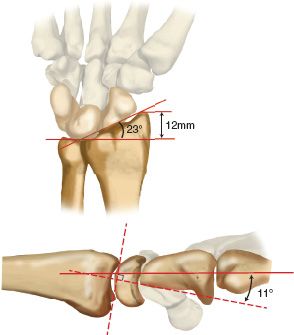
FIGURE 23-4 Radiographic measurements important in assessing fracture reduction and residual deformity: radial inclination (shown here as a normal 23°), radial length (shown here as a normal 12 mm), and volar tilt (shown here as a normal 11°).
2. Modern classification systems—Modern classification systems are treatment-oriented and more specific.
• Frykman classification (1937)—Frykman Types I to VIII are classified according to fracture pattern (Fig. 23-8).
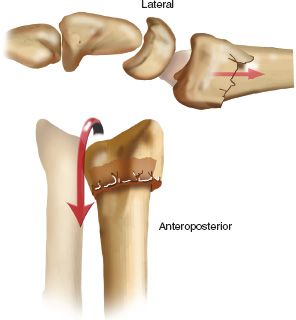
FIGURE 23-5 Typical deformity seen in a Colles’ fracture, showing dorsal comminution and displacement with shortening of the radius relative to the ulna.
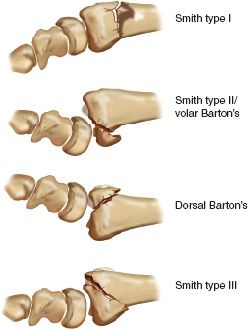
FIGURE 23-6 Thomas’ classification of Smith’s fractures. Type I. extra-articular fracture with volar tilt and displacement of the distal fragment. Type II. intra-articular fracture with volar and proximal displacement of the distal fragment along with the carpus (the same as a volar Barton’s fracture). A dorsal Barton’s fracture is illustrated for comparison, showing the dorsal and proximal displacement of the carpus and distal fragment on the radial shaft. Type III. extra-articular fracture with volar displacement of the distal fragment and carpus. (In Type III, the fracture line is more oblique than in Type I.)
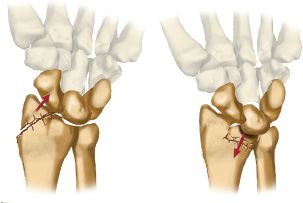
FIGURE 23-7 Left, Chauffeur’s fracture with the carpus displaced ulnarly by the radial styloid fracture. Right, Lunate load (die-punch) fracture with depression of the lunate fossa of the radius that allows proximal migration of the lunate and/or proximal carpal row.
• Melone’s classification (1984)—Melone’s Types I to V are determined by the orientation of the four main intra-articular fragments (Fig. 23-9).
• AO/ASIF classification (1986)—The AO/ASIF system is a comprehensive system of classification. Fractures are classified as one of three possible types: A, extra-articular; B, partial articular; and C, complete articular (Fig. 23-10).
E. Evaluation
1. Plain radiographs—PA and lateral views are standard and demonstrate most fractures. Radiographic measurements can be made (see previous section) to calculate initial displacement and to assess reduction. Standard views also facilitate classification of fractures and choice of treatment. Oblique views detect occult carpal fractures (12% incidence), whereas the PA ulnar-deviation view shows the scaphoid more clearly. Facet lateral views are taken with a 20° proximal tilt to give a better view of the articular surface.
2. Special studies—Special studies are helpful when complex fracture patterns must be assessed or when associated soft-tissue injuries are suspected.
• Computed tomography (CT)—The 1- to 2-mm sections in the sagittal plane are most effective in demonstrating articular depression (die-punch) fractures. Axial views are best for evaluating the distal radioulnar joint and should include the opposite, uninjured wrist for comparison. Three-dimensional reconstructions provide anatomic images and can be useful in surgical planning.
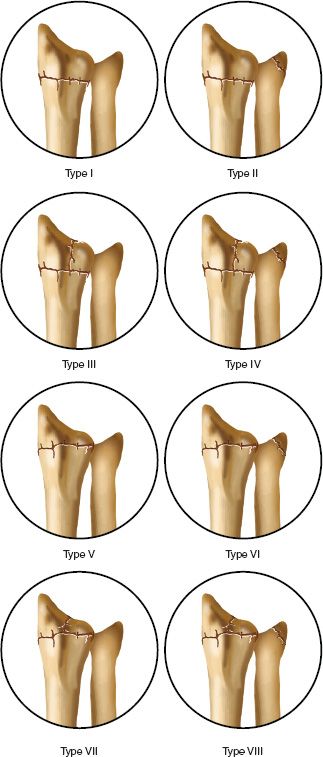
FIGURE 23-8 Frykman classification of distal radius fractures. Types I, III, V, and VII do not have an associated fracture of the ulnar styloid. Fractures III through VII are intra-articular fractures. (Types III and IV involve the radiocarpal joint, Types V and VI involve the radioulnar joint, and Types VII and VIII involve both the radiocarpal and the radioulnar joints.) Higher-classification fractures have a worse prognosis.
• Magnetic resonance imaging (MRI)—MRI should be reserved for suspected soft-tissue injuries (TFCC or scapholunate ligament tears).
• Radionuclide bone imaging—Radionuclide bone imaging may have a role in the detection of occult fractures or the evaluation of reflex sympathetic dystrophy (RSD) as a late complication.
F. Associated Soft-Tissue Injuries—Associated soft-tissue injuries are common in high-energy fractures.
1. Open fracture—Management should include emergent irrigation and debridement, administration of intravenous antibiotics, and early fracture stabilization (external fixation). Wound coverage may require skin grafting or local flap.
2. Median nerve injury—Median nerve injury, usually a neurapraxic injury, commonly improves after fracture reduction. If there is no improvement after 48 hours of observation, exploration and carpal tunnel release are indicated.
3. TFCC injury—TFCC injury has been documented in up to 50% of cases of distal radius fractures when there is an associated ulnar styloid fracture. It often causes late ulnar-sided wrist pain. When the ulnar styloid fracture occurs at the base and is displaced, DRUJ instability is likely present and should be treated.
4. Carpal ligament injury—A complete tear of the scapholunate ligament (most common) can lead to scapholunate instability and if untreated, carpal collapse and posttraumatic arthritis.
5. Tendon injury—Acute tendon laceration is rare but may be seen in fractures with gross displacement. Attritional rupture of the extensor pollicis longus (EPL) tendon may be a late sequela (see later section).
6. Arterial injury—A rare but serious complication, arterial injury (radial or ulnar artery) requires emergent evaluation and repair.
7. Compartment syndrome—Compartment syndrome is seen in approximately 1% of distal radius fractures. The cardinal signs of pain (with passive finger motion), paralysis, and paresthesia should alert the treating physician to this condition. Appropriate fasciotomy of the involved compartments (volar forearm is the most common) is mandatory and most successful when performed early.
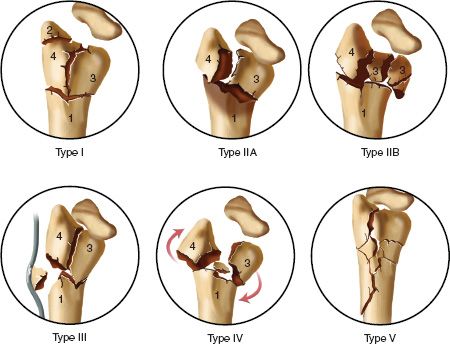
FIGURE 23-9 Melone’s classification of subtypes of four-part intra-articular fractures.
G. Treatment
1. Principles
• Assessment of stability—The stability of the fracture is the most important point to consider when determining treatment. Hallmarks of an unstable fracture include articular depression greater than 2 mm, radial shortening greater than 5 mm, and dorsal tilt greater than 20°. Metaphyseal comminution involving both the volar and dorsal cortices is also indicative of an unstable fracture pattern. In general, a stable fracture can be treated by closed reduction and plaster immobilization, whereas an unstable fracture requires some form of internal or external fixation. Certain fracture patterns are known to be unstable by nature, and as a result, should almost always be treated surgically. These include displaced articular margin fractures: Barton’s and Chauffeur’s fractures (AO Types B1 to B3). DRUJ stability also needs to be assessed on injury radiographs. Widening of the DRUJ or ulnar styloid fracture displacement is indicative of instability.
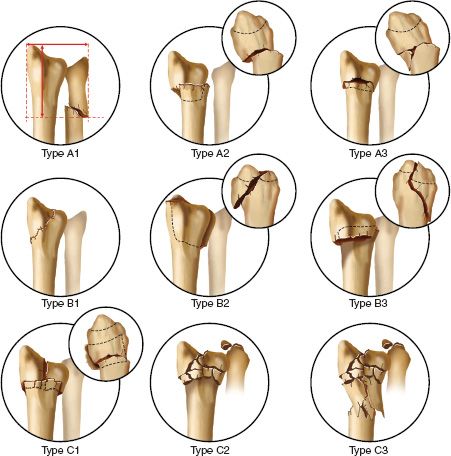
FIGURE 23-10 AO/ASIF classification of distal radius fractures based on the ABC system. The subgroups are not shown. Type A is an extra-articular metaphyseal fracture. The junction of the metaphysis and diaphysis is identified by the “square” or “T” method (the greatest width on the frontal plane of the distal forearm; illustrated on A1). Type A1 is an isolated fracture of the distal ulna. Type A2 is a simple distal radius fracture. Type A3 is a radius fracture with metaphyseal impaction. Type B is an intra-articular rim fracture (preserving the continuity of the epiphysis and metaphysis). Type B1 is a fracture of the radial styloid. Type B2 is a dorsal rim fracture (dorsal Barton’s). Type B3 is a volar rim fracture (volar Barton’s is the same as a Smith Type II). Type C is a complex intra-articular fracture (disrupting the continuity of the epiphysis and metaphysis). Type C1 is a metaphyeal fracture with radiocarpal joint congruity preserved. Type C2 has articular displacement. Type C3 has diaphyseal–metaphyseal involvement. Injury of the distal radioulnar joint is possible in any of these fractures.
• Assessment of reduction—Recent studies have highlighted the importance of achieving and maintaining a near anatomic reduction when treating distal radius fractures in younger patients. Guidelines for an acceptable reduction are (in order of importance) articular step-off less than 2 mm, radial shortening less than 5 mm, and dorsal tilt less than 10°. Failure to achieve and maintain an adequate reduction results in predictable sequelae and potential long-term disability.
2. Methods of reduction
• Closed reduction—Closed reduction relies on ligamentotaxis to restore alignment and correct fracture deformity. Traction/countertraction is used and can be combined with varying degrees of palmar flexion, ulnar deviation, and pronation of the distal fragment. Volar tilt cannot be reliably restored by longitudinal traction alone because of the nature of the radiocarpal ligaments (the volar ligaments tighten first). Alternatively, palmar displacement of the carpus improves volar tilt by using the dorsal periosteal hinge (Fig. 23-11). However, this maneuver requires an intact volar cortical strut without comminution. Postreduction radiographs should be carefully inspected to identify any residual articular step-off or fragment depression (die-punch type).
• Open reduction—Open reduction is indicated when closed reduction has failed to achieve an acceptable result. Articular depression and die-punch fractures often require open reduction through a limited dorsal approach and manual elevation of fragments. Other surgical approaches are recommended for different fracture patterns.
(a) Limited dorsal approach (proximal to Lister’s tubercle)—The limited dorsal approach is indicated for a simple depressed fragment that can be elevated under fluoroscopic control. Fixation is achieved with percutaneous K-wires (oblique or transverse) and may be supplemented with bone graft.
(b) Formal dorsal approach (through the third dorsal compartment and combined with a dorsal arthrotomy)—The formal dorsal approach is indicated for complex joint involvement requiring direct visualization of the articular surface. Fixation is achieved with either K-wires or a dorsal plate. Several low-profile plates have been developed for this specific application. Bone graft or bone graft substitute is usually necessary to support the elevated fragments. SL ligament injuries can also be repaired using the dorsal approach.
(c) Standard volar approach (the interval is between the flexor carpi radialis tendon and the radial artery)—The standard volar approach is indicated for volarly displaced articular margin (Barton’s) fractures. Fixation is usually achieved with a T-plate. This approach is now commonly used to fix dorsally displaced fractures as well. Fixed angle locking plates can be employed to support these fractures.
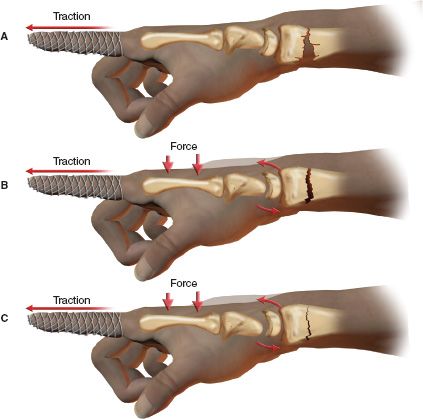
FIGURE 23-11 In a dorsally displaced distal radius fracture, reduction can be obtained by two distinct and separate forms of ligamentotaxis. A. The ligamentotaxis obtained by forces of longitudinal traction restores skeletal length, but the distal fragment remains dorsally tilted. B and C. A palmar translating force (applied by the physician) attempts to sublux the midcarpal joint, creating a force that is transmitted through the proximal carpal row via capsular ligaments to the distal radial fragment, tilting its articular surface palmarly.
(d) Extensile volar approach (the interval is between the ulnar artery and nerve and the carpal canal)—The extensile volar approach is indicated for treatment of complex articular fractures involving the DRUJ and lunate fossa. This approach also allows for carpal tunnel release.
(e) Dorsal radial approach (the interval is between the first and second dorsal compartments)—The dorsal radial approach is indicated for displaced radial styloid fractures. Fixation is achieved with pins or screws.
(f) Combined volar and dorsal approach—The combined volar and dorsal approach is indicated only in the most severe high-energy fractures with both volar and dorsal articular fragmentation.
• Bone grafting—The use of bone graft or bone graft substitute is indicated when there has been significant depression of the radial articular surface. After elevation of the fragments, bone graft is used to fill the metaphyseal defect. This technique prevents late collapse and may allow for earlier mobilization of the radiocarpal joint. Cancellous autograft (iliac crest) has been used traditionally but may be replaced by allograft or graft substitute in certain cases. Bone graft can be used with either pin or plate fixation as long as adequate bone stock is available for implant purchase. In addition to allograft cancellous chips (osteoconductive effect), new formulations are now marketed with demineralized bone matrix (DBM) which may have osteoinductive properties. Graft substitutes are produced from a variety of ceramics including calcium sulfate, calcium phosphate, hydroxyapatite and silicone dioxide (bioactive glass). More recent products have been produced using recombinant technology to create bone morphogenic proteins (BMPs), which have the ability to induce bone forming cells (osteogenic potential).
3. Methods of stabilization—Stabilization techniques can be used alone or in combination as dictated by the fracture type.
• Plaster cast or splint—A plaster cast or splint is the traditional method of treating nondisplaced and stable displaced fractures after closed reduction. Sugar tong splints and long-arm and short-arm casts have been recommended in different combinations, depending on the fracture type and amount of displacement. Regardless of the specific choice, serial radiographs (at 1- to 2-week intervals) are necessary to check for subsequent displacement. Fractures that displace in plaster are by definition unstable and should be treated by other means.
• Pins and plaster—Pins and plaster has become less popular with the advent of external fixation frames. Complication rates may be as high as 50%.
• Percutaneous pin fixation—Percutaneous pin fixation is indicated for unstable extra-articular fractures after successful closed reduction. Certain intra-articular fractures may also be amenable to this treatment, particularly those without significant comminution. Various techniques of pinning have been described and are often combined with external fixation. They include radial styloid pinning, combination radial styloid and dorsal pinning (usually crossed), and intrafocal (Kapandji) pinning placed through the fracture site.
• External fixation—Once the treatment of choice for unstable, comminuted distal radius fractures, external fixation has become less popular with the advent of locking fixed angle plates. Newer external fixator designs allow for multiplanar fracture reduction, including palmar translation, which can be used to restore volar tilt. External fixation frames are often combined with pin fixation to improve fracture stability and reduce distraction forces across the carpus. Overdistraction may lead to finger stiffness and delayed union, and should be avoided. Depressed articular fractures usually require limited open reduction, bone grafting, and supplemental pin fixation in addition to external fixation (Fig. 23-12). When this combination is used, the fixator frame may be removed earlier (4 to 6 weeks vs. 6 to 8 weeks), reducing wrist stiffness. The open technique of fixator pin placement reduces the incidence of eccentric drilling, pin loosening, and radial sensory nerve injury. Additional complications may include pin tract infection, pin breakage, and complex regional pain syndrome. Median nerve compression can occur when the wrist is immobilized in extreme flexion (Cotton-Loder position), so the fixator should be locked in a neutral or slightly extended wrist position. In rare cases of combined volar and dorsal articular involvement, the external fixator must be applied in combination with open reduction with internal fixation (ORIF) of the articular fragments. The plate is usually applied volarly (as a preliminary step) and is followed by dorsal fragment reduction using ligamentotaxis.
• Internal fixation—ORIF has become more popular since the development of volar locking plates. These plates utilize fixed angle screws or pegs to support the intact subchondral bone of the distal radius. Even in cases of severe comminution the locked screws prevent collapse and hold the fragments out to length. The plate is usually applied to the volar aspect of the bone where it is well tolerated and tendon problems are minimized. Elevation of depressed articular fragments and bone grafting can be performed through the fracture site by pronating the proximal fragment. Use of these plates has allowed earlier wrist motion and produced better results when compared to external fixation. Although most distal radius fractures are amendable to volar plating, certain fractures will still require a dorsal or radial approach.
(a) Radial styloid fractures (Chauffeur’s, AO Type B1)—When displaced, radial styloid fractures must be reduced anatomically through a dorsal radial approach. Percutaneous pins or lag screws may be used for fracture fixation.
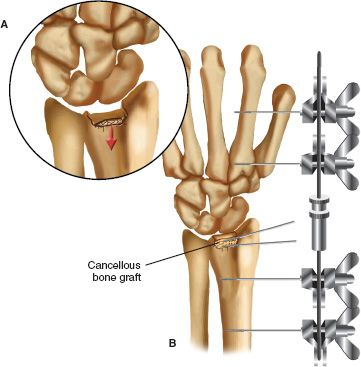
FIGURE 23-12 A. Depressed fracture of the distal radius with a portion of the lunate fossa of the radius dorsally and proximally displaced. B. Treatment of the fracture with application of an external fixation device, carpal distraction, elevation of the depressed fragment and fixation with two K-wires, and cancellous bone grafting of the bony defect left behind by elevation of the depressed fracture fragment.
(b) Articular margin fractures (Barton’s, AO Types B2 and B3)—An AO T-plate is applied either volarly or dorsally depending on the direction of fracture displacement. These fractures are inherently unstable and require buttress plate fixation across the oblique fracture line.
(c) Complex articular fractures (AO types C1 to C3)—Often, complex articular fractures cannot be reduced by other means, necessitating ORIF. The surgical approach is dictated by fracture location. For volar articular fragments, an extensile volar approach, followed by buttress plate fixation, is recommended. Of particular concern is the volar ulnar fragment of the distal radius, which may be difficult to reduce and fix through a standard volar approach. Failure to stabilize this fragment may lead to persistent volar collapse. This type of lunate facet fracture should be approached through an extended carpal tunnel incision. Dorsal fragmentation requires a formal arthrotomy and fixation with a low-profile plate specifically designed for this location. Dorsally applied plates still carry a higher risk of tenosynovitis than volar plates and many (30% to 50%) will need to be removed after fracture healing is complete. These fractures are the most challenging to treat and occasionally require combinations of internal and external fixation and combined volar and dorsal approaches.
• Arthroscopic evaluation and treatment—Techniques of wrist arthroscopy have recently been applied to the treatment of distal radius fractures. Indications have not fully evolved, but several points can be made. Arthroscopy provides an excellent view of the distal radial articular surface; during reduction maneuvers, the joint surface can be visualized directly, avoiding residual articular step-off. Associated carpal ligament and TFCC tears can be easily identified and treated. Arthroscopic evaluation is not without risk, which may include fluid extravasation and neurovascular injury.
• Treatment of ulnar styloid fractures—Treatment of these associated fractures has traditionally received little attention. However, in cases of ulnar styloid base fractures, particularly if widely displaced, instability of the DRUJ will be present. In these cases, ORIF of the styloid fracture is recommended either by tension band wiring or by mini-screw fixation. Because of its attachments to the ulnar styloid, fracture fixation will generally stabilize the TFCC.
H. Late Complications—For acute complications, see earlier section on associated soft-tissue injuries.
1. Malunion—Extra-articular malunion usually involves dorsal tilt and loss of radial length. These deformities in turn lead to ulnocarpal impingement, DRUJ incongruity, and midcarpal instability. Chronic symptoms can include pain, weakness, and loss of motion. Functional limitations can be disabling, especially in younger patients. Corrective surgery is indicated in these cases and involves radial opening wedge (triplanar) osteotomy with corticocancellous bone graft. Intra-articular malunion is even more serious, with an early onset of radiocarpal arthritis in 90% of wrists with more than 2 mm of articular step-off. Surgical treatment usually involves a salvage-type procedure such as arthrodesis or arthroplasty.
2. Nonunion—Nonunion is a rare complication that has occasionally been reported as a result of overdistraction by external fixation.
3. Tendon problems—Tendon problems are relatively common after distal radius fracture and include tendon adhesion, tendinitis (from a dorsal plate), and tendon rupture. The EPL tendon is most often involved and may rupture as a result of mechanical attrition within a narrowed third dorsal compartment. The incidence of tendon rupture is greater in nondisplaced fractures, suggesting that stripped periosteum, as in the case of a displaced fracture, protects the EPL tendon. Direct repair of the EPL tendon is usually not possible; therefore, treatment involves extensor indicis proprius tendon transfer.
4. Complex regional pain syndrome (CRPS)—Also known as RSD, this condition has been reported after distal radius fracture in varying percentages (2% to 20%). Overdistraction by an external fixator has been implicated in some studies. Disabling pain, swelling, finger stiffness, and osteopenia may develop and require long-term treatment. Avoidance of this problem by aggressive hand therapy, edema control, and fixator removal (as early as possible) helps prevent permanent sequelae. When present, CRPS should be treated by a combination of therapy, medications, and stellate ganglion blockade.
I. Rehabilitation—Postfracture rehabilitation should begin early, with finger range of motion exercises starting as soon as the cast or fixator is applied. Overdistraction of the fixator may limit tendon excursion and should be avoided. Similarly, a cast that impedes finger motion may lead to permanent stiffness. After cast or fixator removal, exercises may be advanced as the patient tolerates. Removable splints are helpful in allowing intermittent wrist motion while still protecting a healing fracture. Some patients may require a more formal program supervised by an occupational or physical therapist. Plate fixation may improve wrist function by allowing earlier range of motion.
II. Fractures of the Carpal Bones
A. Fractures of the Scaphoid
1. Overview—Scaphoid fractures are the most common carpal fracture and are typically seen in young men. Radial deviation and wrist dorsiflexion greater than 90° may lead to scaphoid fracture during a fall on the outstretched hand. Fractures of the scaphoid waist are most frequent. Early evaluation and appropriate treatment are important in avoiding nonunion, avascular necrosis (AVN), and late carpal collapse.
2. Anatomy—The proximal pole of the scaphoid is completely intra-articular (with no capsular attachments) and receives all of its blood supply from distal (volar and dorsal) branches of the radial artery (Fig. 23-13). Fractures of the proximal pole depend on intraosseous arterial flow and heal more slowly than distal fractures. They also have a higher risk of nonunion and AVN.
3. Evaluation—“Snuffbox tenderness” is a classic sign and should alert the physician to the possibility of scaphoid fracture. The diagnosis is confirmed radiographically with standard PA, lateral, and oblique views of the wrist. A PA view with ulnar deviation (scaphoid view) shows the scaphoid in profile and should be ordered when the appearance of the initial radiographs is equivocal. Associated ligamentous injuries must be ruled out by careful radiographic assessment or arthrography. When no fracture is seen initially, the wrist should be splinted for 1 to 2 weeks, and another X-ray study should be performed after fracture resorption has occurred. Occult fractures may be detected in this manner or through the use of bone isotope scanning or MRI. CT scanning has proved useful in the assessment of established nonunions with carpal collapse.
4. Classification systems—Most systems highlight the importance of fracture location in regard to treatment and risk of late complications. Waist fractures are most common (65%), followed by proximal pole (25%) and distal pole (10%) fractures.
• Russe system—The Russe system divides scaphoid fractures into transverse, horizontal, oblique, and vertical oblique patterns. Vertical oblique fractures are considered unstable.
• Herbert system—The Herbert system is more comprehensive and also includes delayed union and nonunion (Fig. 23-14).
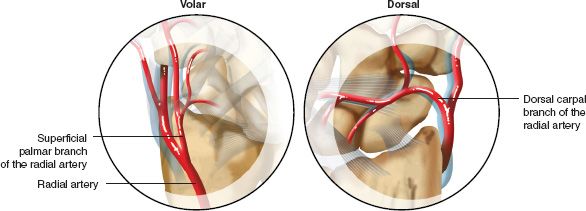
FIGURE 23-13 Blood supply of the scaphoid.
5. Treatment—Treatment is determined by location and degree of displacement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







