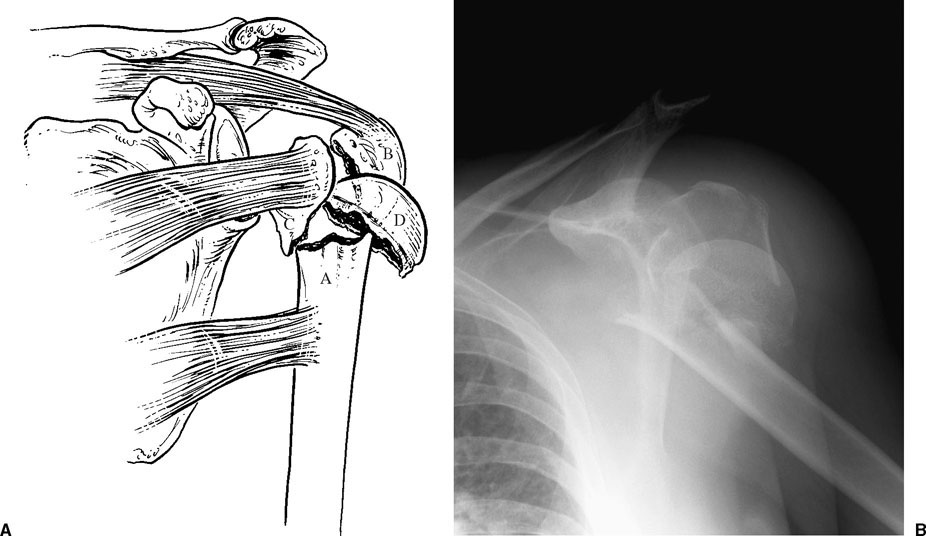
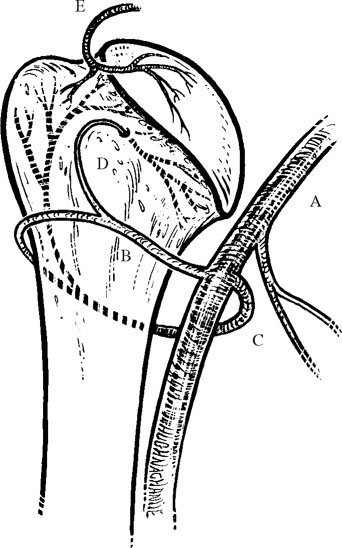
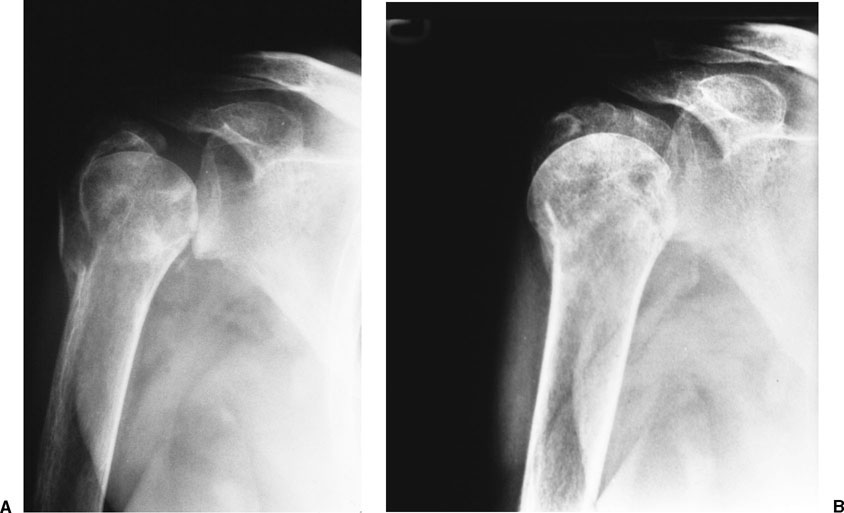
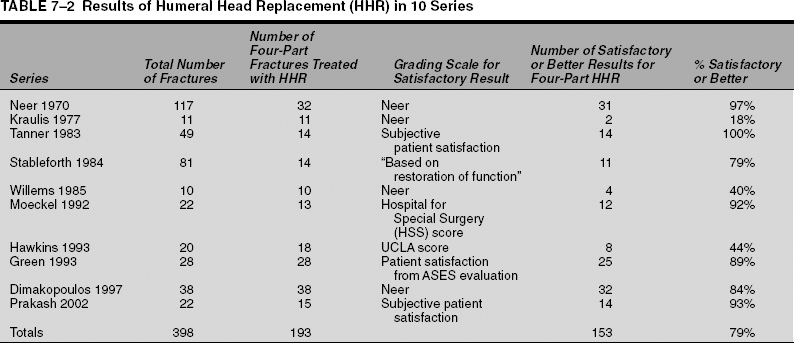
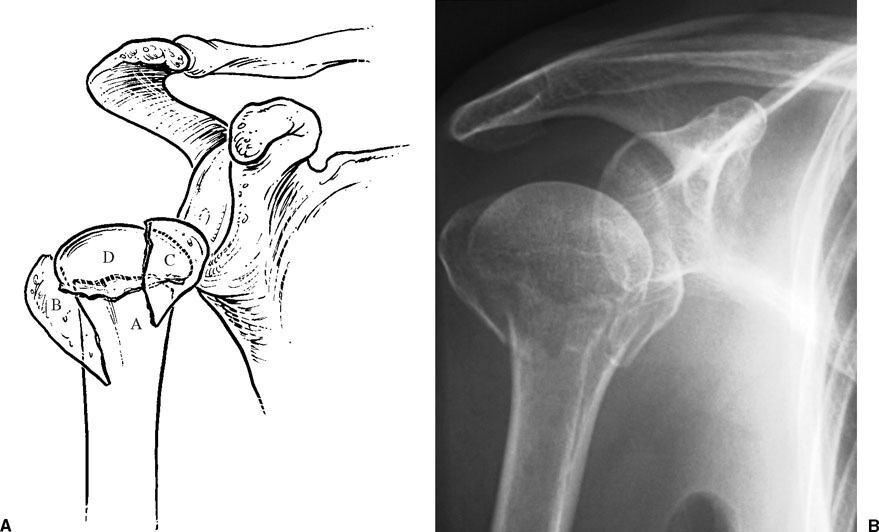
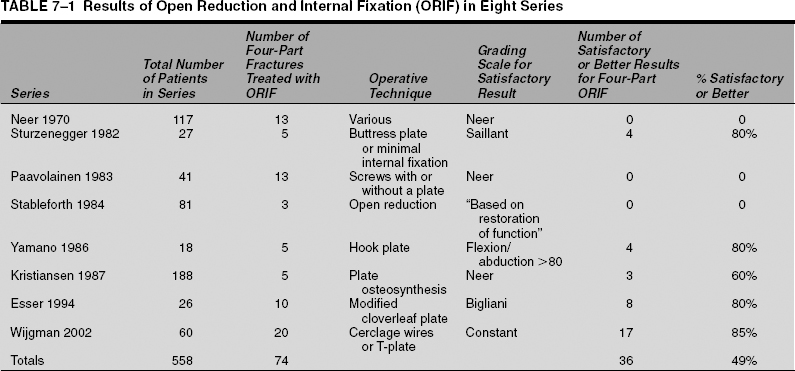
Four-part fractures represent 2 to 10% of all proximal humerus fractures and are associated with a higher energy mechanism of injury.1–5 The displacement pattern of four-part fractures is secondary to the muscular attachments of the different segments. The humeral shaft is displaced medially and anteriorly by the pectoralis major. Retraction of both the greater and lesser tuberosities occurs due to the pull of the rotator cuff tendons, and the separation of these fragments results in a longitudinal tear in the rotator cuff usually along the rotator interval. Classically, the articular segment is displaced and rotated laterally (Fig. 7-1), although its position in a four-part fracture can be variable. Of significance is the loss of soft tissue attachments to the articular segment that compromises the blood supply to the humeral head, resulting in a significant risk of osteonecrosis. A fracture-dislocation is characterized by a dislocation of this articular segment either anteriorly or posteriorly along with this fracture pattern.4 The valgus-impacted four-part fracture has been described as a distinct type of four-part fracture pattern (Fig. 7-2).6–9 Not specifically described in Neer’s original classification, this pattern meets the criterion for displacement of all four segments, but the articular segment is impacted into valgus rather than completely separated from the shaft. This pattern is reported to account for 14 to 35% of all four-part fractures.5,8,10,11 The important distinction between the classical displaced four-part fracture and the valgus-impacted pattern is based on the impact on the blood supply to the articular surface (Fig. 7-3). In the classic displaced pattern, the articular surface is devascularized because it is detached from all soft tissue attachments. Neer reported that six of eight patients treated by open reduction for this type of four-part fracture developed osteonecrosis. This resulted in his recommendation that humeral head replacement should be performed for four-part fractures.4 Subsequent studies have documented osteonecrosis in 20 to 75% of these fractures12–16; however, only 8 to 26% of the valgus-impacted four-part fractures develop osteonecrosis.9,15,16 Jakob et al17 theorized that without lateral displacement of the humeral head, an intact medial periosteum may preserve the blood supply to this fragment. This vascular preservation has been confirmed by radiographic analysis, direct specimen analysis, and perfusion studies.9,18 Information obtained from the patient’s history will direct the treatment of proximal humerus fractures. Patients who sustain four-part fractures and fracture-dislocations are more often elderly with compromised bone quality, making stable internal fixation more difficult to obtain.19 Other factors to consider in deciding treatment include the patient’s activity level, medical status, and the ability to follow a structured postoperative rehabilitation program.5,20–23 The evaluation of the patient with four-part fracture or fracture-dislocation must include a complete evaluation of the patient, with a focused exam of the involved extremity and chest wall. Neurovascular injuries are reported to occur most commonly with anterior four-part fracture-dislocations.4 Stableforth5 reported vascular injuries in four of 81 (5%) four-part fractures.5 Nerve injuries have been reported in 6 to 27% of four-part fractures and can involve the axillary, median, or ulnar nerves or a combination of these nerves.4,5,24 Neer documented 12 nerve injuries in his series of 44 four-part fractures. Five of the nerve deficits occurred after attempted closed reduction of a fracture-dislocation. Ten of the 12 resolved spontaneously.24 Chest wall injuries including rib fracture, pneumothorax, and intrathoracic humeral head dislocation have been documented in association with four-part fractures that occur as a result of high-energy injuries.5 Although four-part fractures and fracture dislocations are most commonly encountered in the elderly, these injuries do occur in young patients and are frequently secondary to high-energy injuries. FIGURE 7-1 The “classic” four-part fracture is characterized by lateral displacement of the articular segment, medial displacement of the lesser tuberosity, and posterior/superior displacement of the greater tuberosity shown graphically (A) and radiographically (B). The four identified fragments are as follows: A, shaft; B, greater tuberosity; C, lesser tuberosity; D, articular segment. FIGURE 7-2 The “valgus-impacted” four-part fracture is characterized by a valgus and impacted position of the articular segment resulting in outward displacement of the tuberosities shown graphically (A) and radiographically (B). The four identified fragments are as follows: A, shaft; B, greater tuberosity; C, lesser tuberosity; D, articular segment. FIGURE 7-3 The blood supply to the humeral head originates form the axillary artery (A) and is derived from the anterior (B) and posterior (C) humeral circumflex arteries through the arcuate artery (D) and from the rotator cuff insertion (E). It may be compromised with four-part fractures, resulting in risk for the development of osteonecrosis. The standard trauma series is usually sufficient to evaluate four-part fracture patterns in the acute setting. Assistance is usually needed to position the patient for the axillary view. Computed tomography (CT) scans can be helpful to further delineate the fracture pattern and displacements, but are not routinely obtained. In our experience, two-and three-dimensional reconstructions have been of limited value. Four-part fractures by definition represent significant displacement of all four segments of the proximal humerus. The deforming muscular forces causing displacement of each fragment makes an adequate closed reduction essentially impossible to maintain.4,19 Closed reduction of four-part fracture-dislocations may also be of limited usefulness due to the limited chance of success and the increased risk of neurovascular injury associated with traction on the injured extremity. Neer reported 11 acceptable closed reductions out of 38 attempts of four-part fractures or fracture-dislocations, with unsatisfactory results in all 11 due to nonunion, malunion, or osteonecrosis.4 A review of five series with a total of 97 four-part fractures treated nonoperatively documented only 5% satisfactory results.4,5,12,14,20,25 Stableforth5 reported greater functional disability and loss of sleep (due to pain) in patients treated nonoperatively compared with those who underwent hemiarthroplasty. Although valgus-impacted fractures have a lower risk of osteonecrosis, closed reduction will also be unsuccessful resulting in malunion.5,9,17 In our experience, nonoperative treatment is reserved for selected patients who are poor operative risks or have very limited functional demands. For these patients, we do not attempt a closed reduction; rather, the degree of deformity is accepted (Fig. 7-4). With a period of 4 to 6 weeks of immobilization, the goal in these patients is limited, painless below-shoulder motion, which may be indeed possible in spite of the residual deformity. Operative management is the recommended treatment for four-part fractures including the classic pattern and the valgus-impacted pattern. Options include open reduction and internal fixation (ORIF) with or without bone grafting, closed reduction with percutaneous fixation, or humeral head replacement with tuberosity reconstruction. Open reduction and internal fixation of four-part proximal humerus fractures is typically reserved for younger patients with good quality bone or for the valgus-impacted fracture pattern. Techniques utilized for fixation of four-part fractures and fracture-dislocations include AO/Association for the Study of Internal Fixation (ASIF) plates and screws,3,26,27 cerclage wires or sutures,16,27 lag screws,16 intramedullary nails,28 or a fixed-angle device.29 Plates can be bent to create improved fixed-angled stability29,30 or modified to minimize the prominence in the subacromial space.26 FIGURE 7-4 (A,B) Nonoperative treatment of this four-part fracture in this 72-year-old patient with significant medical comorbidities resulted in malunion but reasonable function for activities of daily living. Evaluating the results of internal fixation of complex, comminuted proximal humerus fractures requires a careful analysis to confirm the distinction between three- versus four-part fractures, classic displaced versus valgus-impacted fractures, and young patients with better bone quality versus elderly patients with poor bone quality.31 In addition, differentiating the outcomes of four-part fractures versus fracture-dislocations is also important because of the higher energy associated with fracture-dislocations and the greater potential for additional soft tissue injuries. Neer4 reported that open reduction with preservation of the humeral head failed in all eight four-part fractures or fracture-dislocations secondary to osteonecrosis in six and nonunion or infection in the other two. Other investigators have reported that malunion or other soft tissue injuries rather than osteonecrosis is the primary cause for failure of ORIF of these injuries. Lee and Hansen13 did not identify osteonecrosis in their series of 19 four-part fractures and fracture-dislocations treated nonoperatively or by ORIF at an average follow-up of 23.6 months. Four of their patients did demonstrate evidence of revascularization of the humeral head following the transient appearance of osteonecrosis. Gerber et al32 recommend attempting ORIF of four-part fractures in young patients as long as anatomic reduction can be obtained. Their results in patients who developed osteonecrosis in the absence of malunion were similar to the results of primary hemiarthroplasty. Wijgman et al33 demonstrated satisfactory results in 17 of 20 four-part fractures treated with ORIF with cerclage wiring or a T-plate. All three poor results developed symptomatic osteonecrosis, but 10 of the 17 good or excellent results also developed osteonecrosis that had minimal impact on the outcome. Sturzenegger et al16 demonstrated that limited internal fixation of three-and four-part fractures was associated with osteonecrosis in 10% of cases, compared with 30% of fractures treated with plate and screw fixation. They recommended minimal osteosynthesis as an alternative to primary prosthetic replacement. Despite these findings, internal fixation for classic displaced four-part fractures is considered primarily in the younger patient if stable fixation and anatomic reduction can be obtained to allow early rehabilitation exercises.31 A review of eight series reported in the literature identified 74 four-part fractures treated by ORIF and demonstrated a satisfactory result in only 36 patients (49%) (Table 7-1). These reports did not necessarily differentiate between classic or valgus-impacted four-part fractures, which may certainly affect the outcome. Unsatisfactory results were associated with osteonecrosis, wound infection, stiffness, hardware impingement or loosening, malalignment, and axillary nerve palsy.4,5,12,16,26,27,29 Valgus-impacted four-part proximal humerus fractures may be more amenable to closed or open reduction and fixation. Jakob et al17 reported satisfactory results in 14 of 19 patients with this type of fracture. Five patients were treated by closed reduction and Kirschner wire (K-wire) fixation, and 14 were treated by open reduction and fixation by screws, K-wires, or cerclage wires. Osteonecrosis developed in all of the unsatisfactory results and in none of the satisfactory results. Resch et al9 reported 20 good results in 22 valgus impacted fractures. The authors indicated that lateral displacement of the articular surface and severe osteopenia were contraindications to this procedure. In these patients, hemiarthroplasty was recommended. Careful surgical technique with minimal internal fixation resulted in only two cases of osteonecrosis in this series. Functional results correlated with anatomic reduction of the fragments. This technique utilized limited dissection through a deltopectoral approach. The articular fragment was elevated and the tuberosities reduced. Fixation consisted of a combination of percutaneous K-wires and suture repair of the tuberosities. Bone graft was used to fill any void that remained as a result of the initial impaction. Percutaneous fixation for classic displaced four-part fractures has also been attempted but with less favorable results. Resch et al15 reported good results for three-part or valgus-impacted four-part fractures treated with percutaneous reduction and fixation, but two of the five displaced four-part fractures required conversion to prosthetic replacement secondary to loss of reduction or osteonecrosis. Soete et al34 reported similar results with three of their four four-part fractures developing osteonecrosis and unsatisfactory results. Neer4,35 originally recommended humeral head replacement for four-part fractures due to the high complication rate associated with nonoperative management or ORIF; 31 of 32 four-part fractures and fracture-dislocations treated with humeral head replacement and reconstruction of the tuberosities and rotator cuff achieved excellent, good, or satisfactory results, with only one failure due to wound infection. With prosthetic replacement, pain relief is predictable, but functional outcome is unpredictable.4,21,36–38 Isolating the results of four-part fractures and fracture dislocations in 10 studies treated by hemiarthroplasty (totaling 207 fractures), 79% achieved satisfactory or better results in fracture-dislocations treated with prosthetic replacement (Table 7-2).4,5,22,37–43 Many reports combine the results of hemiarthroplasty for all comminuted proximal humerus fractures together, but stratification of the results into fracture types demonstrates the inherent difficulties in reconstructing the more severely comminuted fractures. Goldman et al21 reported better results with hemiarthroplasty for three-part fractures than for four-part fractures. Many authors have demonstrated the correlation of proper reconstruction of the rotator cuff and tuberosities with improved functional outcome.20–22,40,44 Other factors associated with improved results are younger age,21,22,41 male sex,21 and compliance with the postoperative rehabilitation program.20,23,40 Prosthetic reconstruction after failed ORIF or malunion following four-part humerus fractures is more technically challenging and is more commonly associated with complications and worse functional results than hemiarthroplasty for acute fracture.38,45–47 This emphasizes the importance of acute fracture management to optimize outcomes. We prefer to perform humeral head replacement with tuberosity reconstruction for the vast majority of four-part fractures and fracture-dislocations. The exceptions are the treatment of valgus-impacted four-part fractures and fractures that occur in younger patients with good bone stock in whom an acceptable reduction and secure fixation can be achieved. We will describe techniques for hemiarthroplasty followed by our preferred approaches for ORIF. FIGURE 7-5 Patient positioning for proximal humeral replacement. The basic principles of prosthetic replacement for proximal humerus fractures include (1) utilization of a deltopectoral approach that preserves the origin and insertion of the deltoid muscle; (2) insertion of the proximal humeral prosthesis to restore humeral length and proper retroversion; and (3) secure fixation of the tuberosities to the prosthesis, to the humeral shaft, and to each other to allow early postoperative rehabilitation. The success of humeral head replacement depends, in large part, on close attention to the technical details of the procedure and the utilization of meticulous surgical technique. The patient should be placed on the operating table in a supine position. The head of the operating table should be elevated ~30° in a modified beach chair position. A small bolster should be placed behind the involved shoulder. The patient should be moved to the side of the table so that the upper extremity can be placed into maximum extension without obstruction by the operating table (Fig. 7-5). The patient should be secured to the operating table to minimize any changes in position intraoperatively. The entire upper extremity should be prepped and draped to allow full mobility during the procedure. A straight deltopectoral incision is used that begins just lateral to the tip of the coracoid process and extends distally and laterally to the insertion of the deltoid (Fig. 7-6). The subcutaneous tissues are divided, and medial and lateral flaps are elevated to expose the deeper muscular layers. The deltopectoral interval is identified by localization of the cephalic vein. The cephalic vein is usually retracted laterally with the deltoid muscle. In some instances, the cephalic vein is more easily retracted medially with the pectoralis major. In either case, care should be taken to preserve the cephalic vein throughout the procedure. The sub-deltoid space is mobilized, as is the pectoralis major. The conjoined tendon muscles are identified, and the clavipectoral fascia is divided at the medial edge of the conjoined tendon muscles. The fracture hematoma is usually evident after dividing the clavipectoral fascia. The conjoined tendon muscles and the pectoralis major are retracted medially and the deltoid is retracted laterally. This can be most easily accomplished with the use of a self-retaining type of retractor. After the fracture hematoma has been evacuated, the deeper structures can be visualized. The biceps tendon should be identified and tagged with a suture (Fig. 7-7). The biceps tendon provides an orientation to the greater and lesser tuberosities. The lesser tuberosity is located medial to the biceps tendon and the greater tuberosity is located superiorly and laterally. Each tuberosity should be tagged with a No. 2 suture for easier mobilization (Fig. 7-8). These sutures should be placed at the tendon insertion site because this is generally the most secure area; placement of the sutures through the tuberosity itself can result in fragmentation. The lesser tuberosity is mobilized and retracted medially, while the greater tuberosity is retracted laterally and superiorly. This allows visualization of the articular segment. In four-part fractures this segment is generally devoid of soft tissue attachments and is easily removed. The coracoacromial ligament should be identified at its coracoid attachment and followed to its acromial attachment. We feel it is important to preserve the coracoacromial ligament because of its contribution to anterosuperior stability.
Four-Part Fractures and Fracture-Dislocations
 Clinical Evaluation
Clinical Evaluation
Radiographic/Imaging Studies
 Treatment
Treatment
Nonoperative
Operative
Preferred Operative Techniques

Humeral Head Replacement
Surgical Approach
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree