Forearm Fractures
CASE PRESENTATION
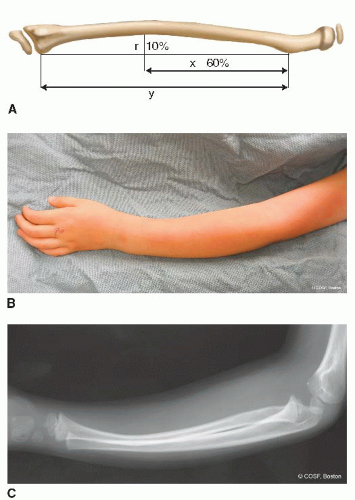
A 10-year-old male presents for evaluation of forearm pain after a fall off a skateboard. He denies any distal numbness, weakness, or tingling. Examination demonstrates obvious deformity of the forearm and a small volar ulnar 1-cm wound. The hand is well perfused, and grossly he is neurologically intact in the radial, ulnar, and median nerve distributions. Radiographs are shown in Figure 33-1.
CLINICAL QUESTIONS
How common are diaphyseal forearm fractures in children and adolescents?
How are diaphyseal forearm fractures classified?
What are the maneuvers used for closed reduction of displaced incomplete and complete forearm fractures?
What are the limits of radiographic deformity that will remodel over time?
What are the indications for surgical treatment?
What are the surgical approaches and techniques used for internal fixation of diaphyseal forearm fractures?
What are the complications of forearm fractures and their surgical management?
What are the indications and techniques for deformity correction in diaphyseal forearm fracture malunions?
What are the anticipated results of surgery?
THE FUNDAMENTALS
Forearm fractures are among the most common injuries requiring surgical care in children.1,2 Despite established treatment principles and advances in surgical techniques, forearm fractures continue to present clinical challenges, even to the pediatric hand and upper extremity surgeon. There is a wide spectrum of fracture pattern and presentation, a host of nonoperative and surgical treatment options, constant consideration of skeletal growth and remodeling potential, and ever-changing patient and family expectations. Historically, almost all pediatric forearm fractures were treated nonoperatively with closed reduction and cast immobilization. However, treatment patterns continue to evolve, perhaps due to increasing awareness of patient-derived functional outcomes; desires for more expedient return of motion, strength, and sports participation; and improvements in technical abilities. Understanding of the treatment principles and mastery of surgical techniques is essential for the pediatric hand and upper limb specialist (see Sidebar).
Etiology and Epidemiology
Forearm fractures occur in approximately 1:100 children each year.2 When distal radius and ulna fractures are considered separately, diaphyseal forearm fractures represent the third most common long bone fracture in children, following distal radius and supracondylar humerus fractures.1 The forearm is the most common site of open fractures of the upper extremity and the most common location of refractures in the pediatric patient population.3 Peak age of incidence is between 12 and 14 years of age, perhaps due to the combination of rapid skeletal growth and increased sporting and high-energy activities.
 FIGURE 33-1 Anteroposterior (AP) and lateral radiographs of a grade I open forearm fracture in a 10-year-old male. |
SIDEBAR
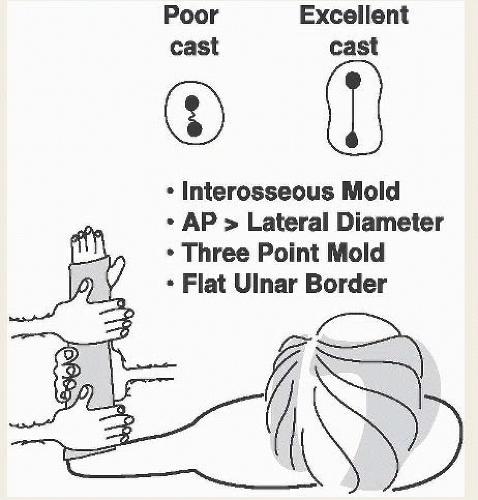
Molds and Burns: The Lost Art of Casting
Pediatric hand and upper extremity surgeons must not only possess surgical skill but also expertise in nonoperative fracture care. In the age of emerging technologies and increasing choice of surgical approaches, implants, and techniques, the merits of cast immobilization cannot and should not be forgotten. Indeed, perhaps more important than techniques of achieving reduction or methods of internal fixation is proper cast application.
In appropriate patients, successful closed treatment of diaphyseal forearm fractures involves application of a well-molded cast. As Mercer Rang and others have taught us, there are several elements to a properly molded cast (Figure 33-2). First, a three-point bending mold should be applied to maintain angular correction. Second, an interosseous mold should be applied to preserve the interosseous space, with care taken to ensure that the AP diameter is greater than the lateral. Third, a straight ulnar border should be maintained to ensure ulnar alignment and an acceptable aesthetic result. Finally, a supracondylar mold above the flexed elbow will help to prevent cast migration, particularly in the very young patient.
Any cast applied will eventually need to be removed, and often a cast will need to be bivalved shortly after application to accommodate soft tissue swelling. While seemingly straightforward, cast removal may result in lacerations or thermal injuries during inappropriate cast saw use.56, 57, 58 and 59 In the pediatric population, risk is particularly high, as casts are bivalved or removed in the nonverbal, sedated, or anesthetized patient, who cannot communicate pain or discomfort. This is an entirely preventable complication and one we feel should never occur.
Both common sense and published information inform us that cast saw injuries may be avoided by a number of simple preventative interventions. Adequate cast padding of at least three to four layers should always be applied. When applying plaster casting material, excessive thickness and higher ambient dip water temperatures (>24°C) should be avoided. Sufficient time should be allotted to allow plaster material to cure and cool before fiberglass material is over-wrapped. Oscillating cast saws should be kept sharp, with frequent cooling during use to avoid thermal skin injury. With these simple steps, cast saw injuries may be prevented.
The mechanism of injury is usually a fall onto an out-stretched upper extremity, imparting axial, rotational, and/or bending forces to the radius and ulna. The position of the forearm and the forces applied determine the fracture pattern. Bending injuries typically cause same-level radius and ulna fractures, while rotational forces result in fractures at different levels. With higher energy mechanisms of injury, greater degrees of soft tissue injury occur, leading in some cases to ligamentous disruption and open fractures.4, 5 and 6
Clinical Evaluation
Patients will present with pain, swelling, deformity, and limited forearm motion. Circumferential inspection of the limb should be made to assess for wounds or lacerations suggestive of open fractures. Palpation and evaluation of the elbow and wrist should similarly be performed, as tenderness or deformity may indicate adjacent joint injury or concomitant fractures. The vascular and neurological status should be systematically examined to rule out associated vascular injury, nerve palsy, or impending compartment syndrome.7, 8 and 9
Standard AP and lateral radiographs of the entire forearm are performed in all cases of suspected forearm fracture and will confirm the diagnosis. Systematic evaluation of the wrist and elbow should be performed, even in the setting of known bony injuries. Information regarding
rotational alignment of the radius and ulna can be derived from the position of bony landmarks. On AP projections, the radial styloid lies 180 degrees opposite the bicipital tuberosity; on the lateral projection, the ulnar styloid is also positioned 180 degrees from the coronoid process. Even using these radiographic landmarks, malrotation is difficult to quantify using radiographic indices and may be within 45 degrees of accuracy.10,11
rotational alignment of the radius and ulna can be derived from the position of bony landmarks. On AP projections, the radial styloid lies 180 degrees opposite the bicipital tuberosity; on the lateral projection, the ulnar styloid is also positioned 180 degrees from the coronoid process. Even using these radiographic landmarks, malrotation is difficult to quantify using radiographic indices and may be within 45 degrees of accuracy.10,11
Forearm fractures are classified according to anatomic location (proximal, middle, or distal thirds), fracture displacement and angulation, and fracture pattern. In general, three patterns occur in skeletally immature patients: plastic deformation injuries, greenstick (incomplete) fractures, and complete fractures. Each fracture pattern has its unique anatomic features and treatment considerations.
Radiographically, plastic deformation, or traumatic bowing, presents as bones that are “bent but not broken.”12 Typically affecting younger patients under 10 years of age, there is often little clinical deformity, swelling, ecchymosis, and/or tenderness. Forearm rotation, however, will be limited. Radiographic findings may be subtle, characterized by abnormal curvature of the radial and/or ulnar shafts in association with narrowing of the interosseous space. An understanding of the normal radiographic appearance of the radius and ulna, and in particular the normal radial bow, is imperative in identifying plastic deformation injuries13 (Figure 33-3). Depending on the severity of the plastic deformation, the physical exam in patients with these injuries ranges from subtle motion and aesthetic differences, to a block to rotational motion, and an S-shaped forearm grossly. Identification of the injuries with limited motion acutely is important for a positive long-term outcome.
Greenstick, or incomplete, fractures result from torsional and bending injuries in younger children. Radiographically, one cortex is disrupted while the other cortex remains intact or is plastically deformed. Due to the inherent stability conferred by the intact cortex, closed reduction and cast immobilization remain the standard of care.
Complete fractures are those in which there is complete cortical disruption. These injuries are akin to their adult counterparts in mechanism of injury, clinical presentation, and radiographic appearance.
Because the ulna is subcutaneous in location and straight in alignment, ulnar deformity results in aesthetic differences. Conversely, radial malalignment is less visible but results in loss of forearm rotation. While loss of pronation is well compensated for by shoulder abduction, forearm supination loss is poorly tolerated due to the blocking effect of the thorax with attempted shoulder adduction to bring the palm in an upward position.11 Multiple published series have demonstrated that diaphyseal fracture malunions contribute to loss of forearm rotation and functional impairment.11,14, 15 and 16 Cadaveric studies have demonstrated that <10 degrees of angulation results in little if any loss of forearm rotation. Greater than 10 degrees of angulation will proportionally impede forearm rotation. More proximal bony deformity will impart greater restrictions in forearm rotation. As a result, less angular deformity is tolerated in more proximal than more distal fractures. Malrotation, while difficult to quantify radiographically, similarly causes loss of forearm rotation.17,18 Indeed, for every degree of rotational deformity, 1 to 2 degrees of forearm rotation may be lost. In general, ulnar malrotation does not alter the overall arc of forearm rotation but does change the “set point” of forearm motion. Radial malrotation, on the other hand, does reduce the overall arc of forearm supination-pronation. Ultimately, however, clinical forearm rotation and radiographic alignment are poorly correlated.19
Additional consideration must be made for bony remodeling. With fracture healing and subsequent skeletal growth, a number of bony changes occur. The adjacent physis is reoriented. The bone continues to elongate, reducing the apparent angular deformity. And finally, appositional periosteal bone formation, typically at the
concavity of the deformity, serves to “correct” angulation and displacement. Clearly, remodeling potential is greatest in younger patients, in fractures closer to the adjacent physis, and with deformity in the plane of adjacent joint motion. In general, up to 20 degrees of diaphyseal angulation may remodel in children under 8 years of age. Beyond the age of 10 years, however, more than 10 degrees of angulation is not likely to remodel spontaneously.
concavity of the deformity, serves to “correct” angulation and displacement. Clearly, remodeling potential is greatest in younger patients, in fractures closer to the adjacent physis, and with deformity in the plane of adjacent joint motion. In general, up to 20 degrees of diaphyseal angulation may remodel in children under 8 years of age. Beyond the age of 10 years, however, more than 10 degrees of angulation is not likely to remodel spontaneously.
The available published information provides guidelines as to how much radiographic deformity can be expected to remodel with continued skeletal growth. Up to 1 cm of shortening may be accepted with little impact on forearm rotation, perhaps due to relaxation of the interosseous membrane.11,20 Complete or 100% translation may remodel in younger patients in fractures of the middle and distal thirds.10,11,20 Radioulnar angulation is less well tolerated, due to narrowing of the interosseous space and bony impingement during forearm rotation. Mehlman and Wall3 have proposed the “20-15-10” rule to guide what constitutes acceptable angulation in radius and ulna fractures. Dividing the forearm into thirds, 20, 15, and 10 degrees of angulation may be accepted in the distal, middle, and proximal thirds of the forearm, respectively.
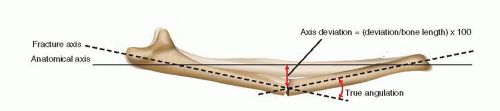
In addition to angulation, displacement, and translation, other tools have been proposed to predict the final position and ultimate outcomes of diaphyseal forearm fractures.21,22 Younger et al. have proposed that axis deviation be utilized to predict outcomes following forearm diaphyseal fractures and thus to guide when closed reduction or surgical intervention is required (Figure 33-4). Axis deviation is defined as the distance between the fractured and anatomical axes of the bone measured at the fracture site, divided by the total length of the bone multiplied by 100. An axis deviation of >5 at the time of bony healing (i.e., cast removal) has been correlated with restricted forearm motion even after completion of skeletal growth and bony remodeling. The advantages of the axis deviation index are that it eliminates variables associated with vagaries of radiographic projection, magnification, and fracture location and does not rely strictly on radiographic angulation or translation to predict functional loss.
As clinical motion does not directly correlate with radiographic alignment, a more important question is “how much bony deformity can still allow for reasonable functional outcomes?” Historically, up to 10 degrees of angulation, complete translation, and 30 to 45 degrees of malrotation were thought to be well tolerated without functional limitations.11 These parameters should be considered carefully, particularly given the patient and family expectations for restoration of full forearm rotation.
Surgical Indications
We make a living by what we get, but we make a life by what we give.
—Winston Churchill
The goals of diaphyseal forearm fracture treatment are to achieve bony healing, preserve forearm motion, prevent aesthetically displeasing deformity, and avoid complications.16,19,23,24
With this in mind, closed reduction should be considered in all acute displaced diaphyseal forearm fractures. Surgical indications include open forearm fractures, floating elbow injuries, fractures with vascular injury, fractures with soft tissue swelling precluding circumferential cast immobilization, and irreducible or unstable fractures with deformity beyond what would be anticipated to remodel, given the fracture pattern and patient age. Diaphyseal forearm refracture is considered a relative indication for surgery.
Although there are a host of surgical options, percutaneous pinning is generally insufficient, and external fixation is used most commonly in grade III open fractures and fractures with vascular impairment.25 Currently, most forearm diaphyseal fractures are treated with intramedullary (IM) fixation or internal fixation with plate and screw constructs.
SURGICAL PROCEDURES
• Closed Reduction of Incomplete Fractures
Closed reduction should be performed for all plastic deformation injuries with >20 degrees of angulation in patients over 4 years of age, given the limited remodeling potential.12,26,27 Although seemingly straightforward, forces as high as 30 kg sustained over several minutes are required
to correct traumatic bowing.26 As a result, controlled three-point bending over a sandbag, rolled towel, or the clinician’s thigh should be performed under general anesthesia or well-administered conscious sedation (Figure 33-5



to correct traumatic bowing.26 As a result, controlled three-point bending over a sandbag, rolled towel, or the clinician’s thigh should be performed under general anesthesia or well-administered conscious sedation (Figure 33-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree