1. Definition—Malformation (most often, Congential maldeformation), “Too few” (see Table 1-1, Chapter 1)
a. Congenital deficiency (failure of formation) of one or more central rays (toe or toe and metatarsal [MT]) of the foot (Figure 6-1)
b. The most extreme form is absence of all but the lateral ray of the foot.
c. The most subtle form is a soft tissue cleft between the 1st and 2nd MT heads, with no bone deficiency.
2. Elucidation of the segmental deformities
a. Toes
i. Absence of 0–4 toes
• In the most subtle presentation, there is a soft tissue cleft between the 1st and 2nd MT heads, with no toe deficiency or mere deficiency of the distal phalanx of the 2nd toe.
• 5th toe and MT are always present, or the diagnosis would be congenital transverse deficiency of the midfoot.
ii. Hallux valgus and 5th toe varus—typically seen in feet with 3 or fewer rays (Figure 6-1)
b. Forefoot
i. Dorsiflexed (and often hypermobile) 1st ray—typically seen in feet with 3 or fewer rays
ii. Absence of 0 to 3 central rays (toes and associated MTs, and occasionally cuneiforms) of the foot, and including the 1st ray in the most extreme form
iii. Splaying of the border rays
iv. Soft tissues envelop the formed medial and lateral bony rays, thereby creating a central cleft (Figure 6-1).
c. Midfoot
i. Abducted lateral ray(s)
ii. Adducted 1st ray
d. Hindfoot
i. Neutral or valgus
• Occasionally with synchondrosis/synostosis of the hindfoot/midfoot bones
e. Ankle
i. Possible ball-and-socket
3. Imaging
a. Simulated standing or standing anteroposterior (AP), lateral, and oblique of the foot
b. AP, lateral, and mortis of the ankle
4. Natural history
a. Comfort and function are satisfactory in most cases with the use of modified shoe wear
b. Shoe-fitting problems and pain are experienced in the more severely deficient forms because the splaying of the MTs results in excessive width of the forefoot in relation to the length of the foot.
5. Nonoperative treatment
a. Accommodative shoe wear, including custom shoes if necessary
6. Operative indications
a. Inability to provide shoe-fitting comfort even with custom-made shoes and inserts/orthotics
7. Operative treatment with reference to the surgical techniques section of the book for each individual procedure
a. Individualize treatment
i. Be creative
ii. Opening or closing wedge osteotomies of the midtarsal bones or MTs should be performed to narrow an excessively wide and painful forefoot. Supplement the osseous reconstruction by resecting some of the redundant soft tissues in the cleft and approximating the dorsal and plantar skin edges without tension (Figure 6-2).
b. Soft tissue procedures and even distal MT osteotomies that are used to correct hallux valgus and 5th toe varus are rarely successful.

Figure 6-1. Bilateral cleft foot, class IV according to the Blauth and Borisch classification.
Longitudinal Epiphyseal Bracket
1. Definition—Congenital mal-deformation, “Too large” (see Table 1-1, Chapter 1)
a. “Delta phalanx” of a MT
b. Almost exclusively the 1st MT, though I have seen it in the 5th MT in two syndromic children.
c. The epiphysis and physis wrap around the medial side of the 1st MT diaphysis connecting the normal proximal epiphysis with a distal pseudoepiphysis. This leaves only the lateral side of the diaphysis without an overlying epiphysis (Figure 6-3).
d. Longitudinal epiphyseal bracket (LEB) is always associated with either preaxial polydactyly (see this chapter) or congenital hallux varus (see Chapter 5), though both conditions may exist without an LEB.
2. Elucidation of the segmental deformities
a. Short, wide 1st MT with varus orientation of the 1st metatarsophalangeal (MTP) joint and varus alignment of the hallux on the 1st MT
i. Always associated with either congenital hallux varus or preaxial polydactyly
3. Imaging
a. Simulated standing AP and lateral of the foot (Figure 6-3)
b. Although it is not necessary if the plain x-rays are characteristically diagnostic, an MRI will show the pathoanatomy well (Figure 6-3).
4. Natural history
a. Increasing or persistent varus deformity of the hallux, causing shoe-fitting difficulties
b. Increasing length discrepancy between the 1st and 2nd MTs, resulting in stress overload and pain under the 2nd MT head (Figure 6-4)
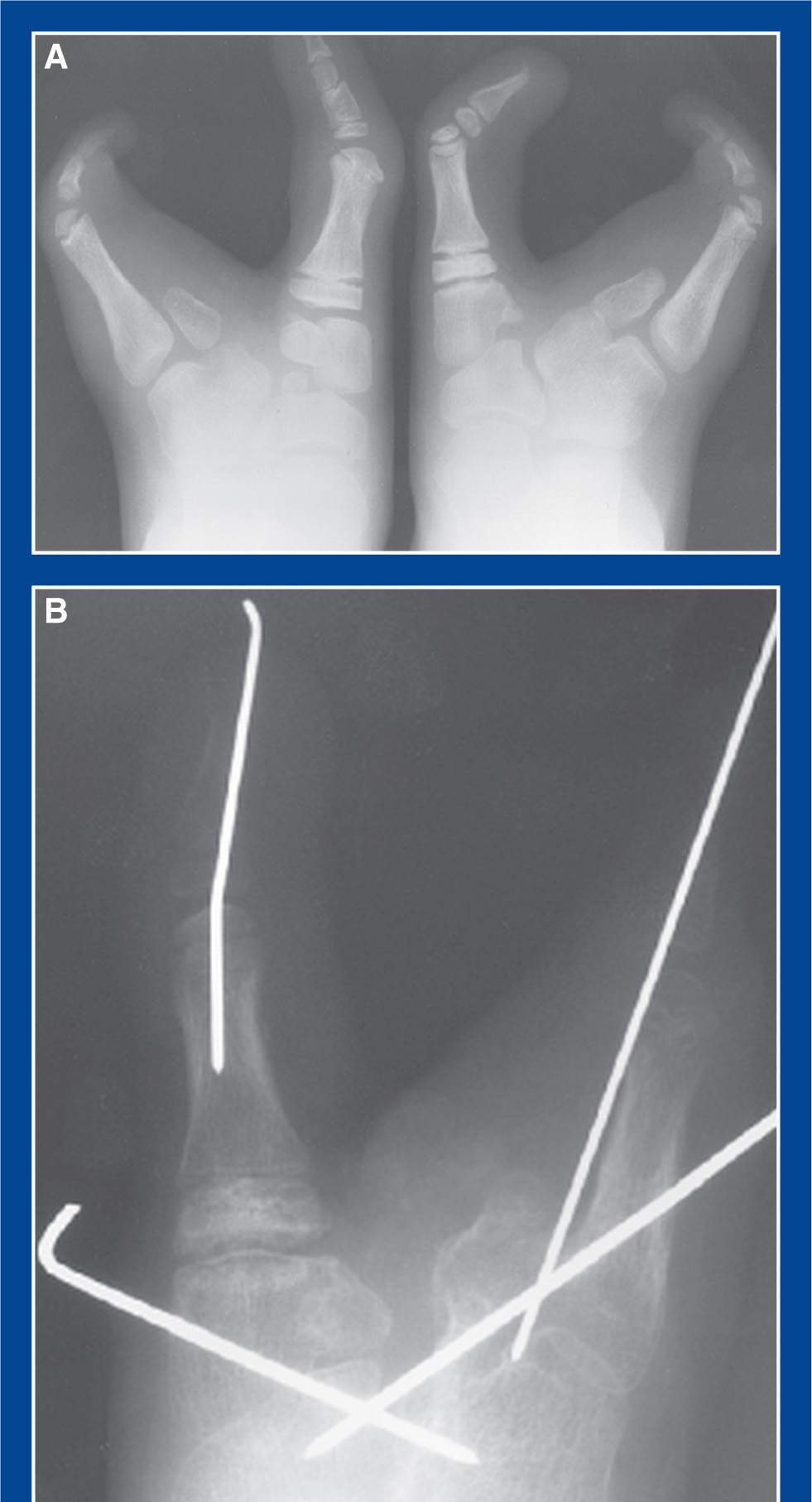
Figure 6-2. A. Preoperative AP x-ray of painful cleft feet. B. Postoperative AP x-ray of the right foot following medial and lateral column midfoot osteotomies and MTP joint capsulotomies. As anticipated, the toes returned to their original positions after the pins were removed, but the midfoot deformity correction persisted long term. (From Mosca VS. The foot. In: Weinstein SL, Flynn JM, eds. Lovell and Winter’s Pediatric Orthopaedics. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013:1411, Figure 29-27.)
5. Nonoperative treatment
a. None
6. Operative indications
a. Presence of the malformation—it is best to operate when the child is over 6 months of age (due to technical considerations associated with the small size of the pathology) but under 1 year.

Figure 6-3. A. AP x-ray of a first MT LEB associated with preaxial polydactyly in an infant. The lateral cortex of the diaphysis is concave and has the normal density of cortical bone. The medial cortex is convex and does not have normal cortical bone density. It has the density more characteristic of metaphyseal bone adjacent to a normal physis. B. The LEB is outlined wrapping around the medial side of the 1st MT diaphysis connecting the normal proximal epiphysis with a distal pseudoepiphysis. C. An MRI of the same foot shows the LEB wrapping around the 1st MT shaft from proximal to distal (green arrows outline it). The two adjacent proximal phalanges (dark rectangular shadows indicated by yellow dashed arrows) can be seen distal and distal-medial to the LEB. NOTE: An MRI is not required if the plain x-rays are characteristically diagnostic.
7. Operative treatment with reference to the surgical techniques section of the book for each individual procedure
a. Resection of the LEB (see Chapter 8), with preservation of the normal proximal epiphysis and the distal pseudoepiphysis
i. Concurrent soft tissue release of the congenital hallux varus, if present
ii. Concurrent resection of a duplicate hallux, if present
1. Definition—Malformation, “Too large” (see Table 1-1, Chapter 1)
a. Congenital enlargement of all tissue types in a ray (toe and MT) in a linear and circumferential array, starting distally at the tip of a toe and extending proximally to a variable extent along a ray (Figure 6-5)
b. Occasionally, enlargement is present in adjacent rays to the same or a lesser extent, always starting distally at the tip of a toe and extending to a variable extent proximally along a ray (Figure 6-6).
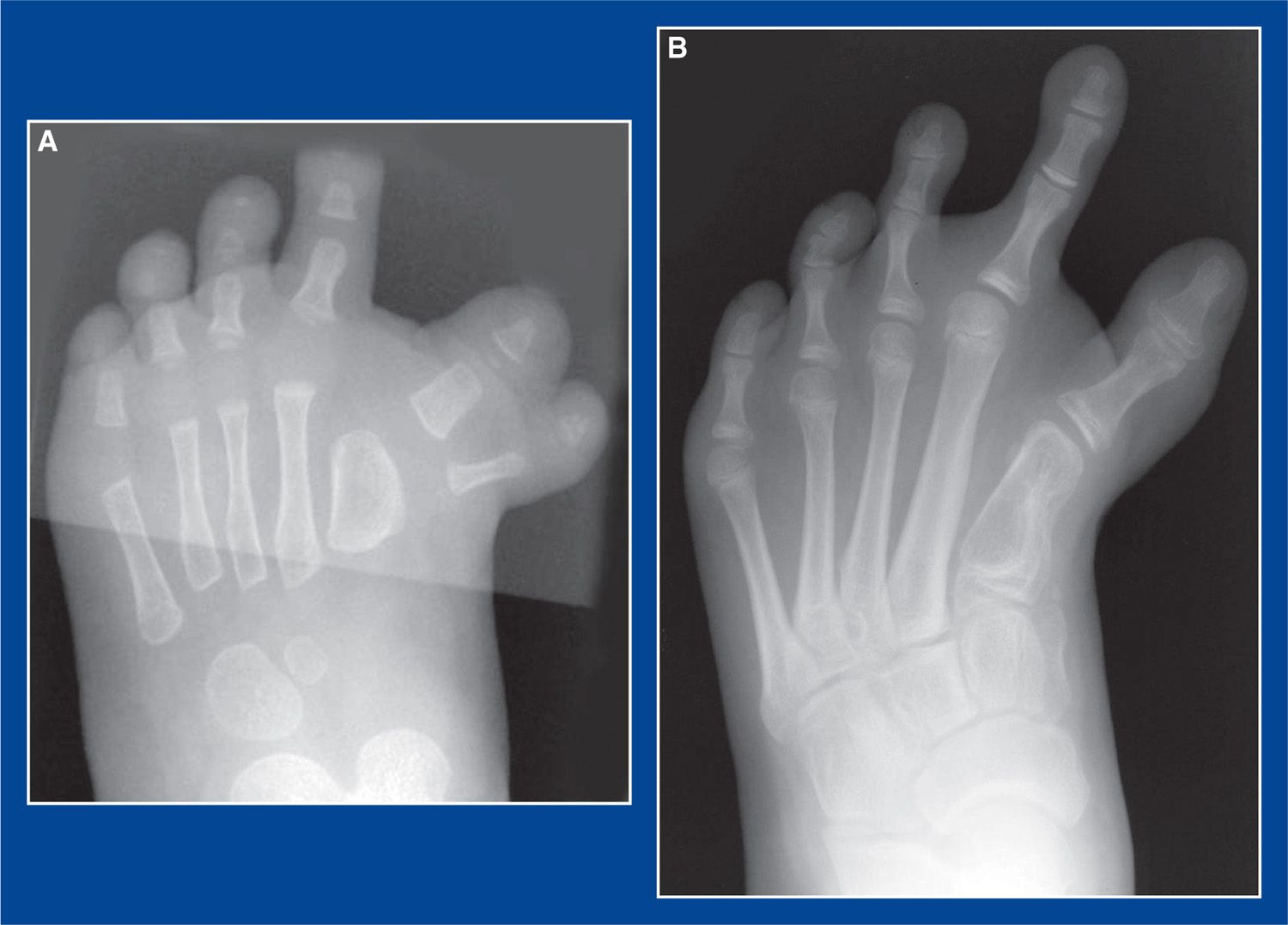
Figure 6-4. A. AP x-ray of preaxial polydactyly associated with a LEB of the 1st MT. B. The duplicate hallux was resected, but the LEB was not. Years later, there is a short 1st MT with varus deformity, hallux varus with toe pain when wearing shoes, and pain under the 2nd MT head due to stress transfer. Note the hypertrophy of the 2nd MT caused by the stress transfer.

Figure 6-5. Typical macrodactyly of the 2nd ray in a foot.
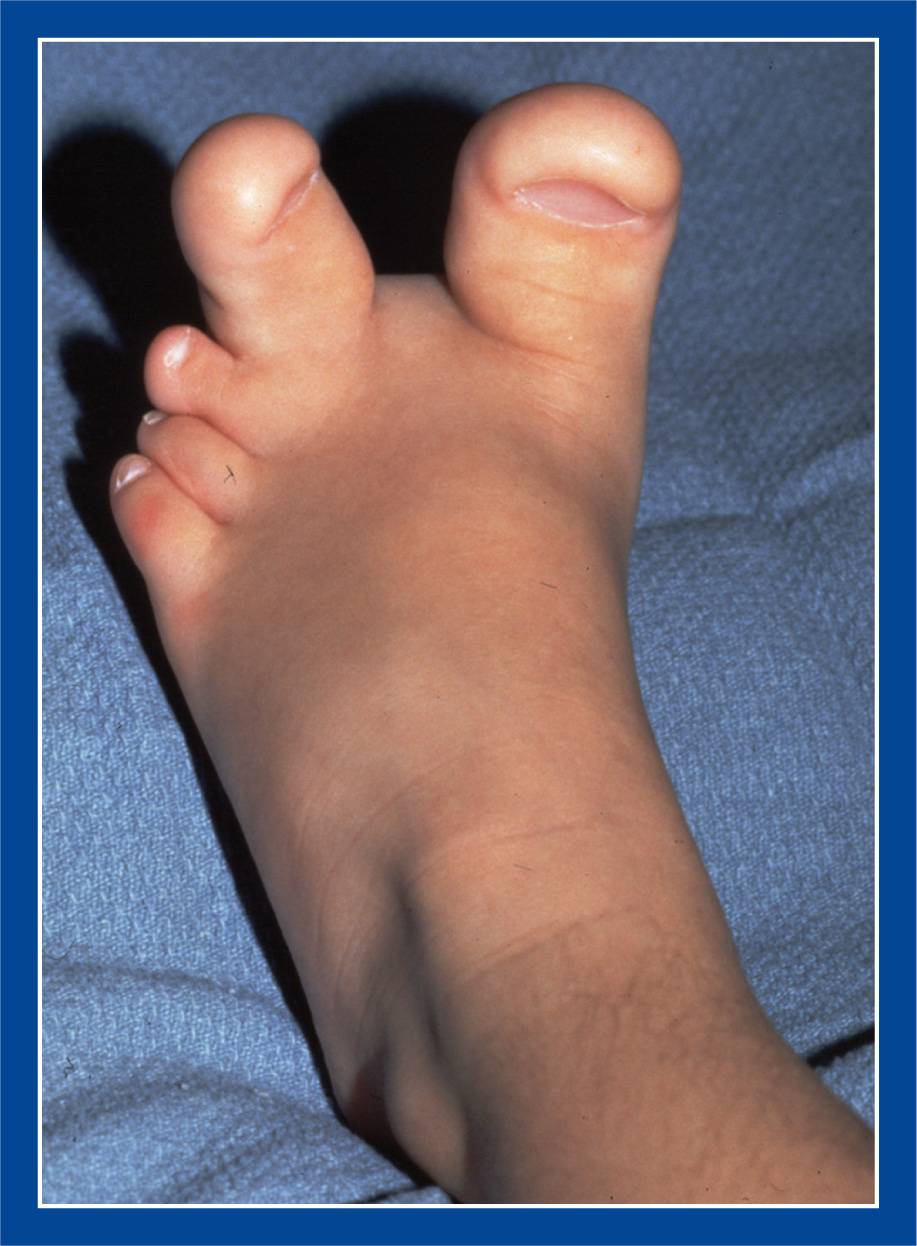
Figure 6-6. Macrodactyly of the 1st and 2nd rays in a foot.
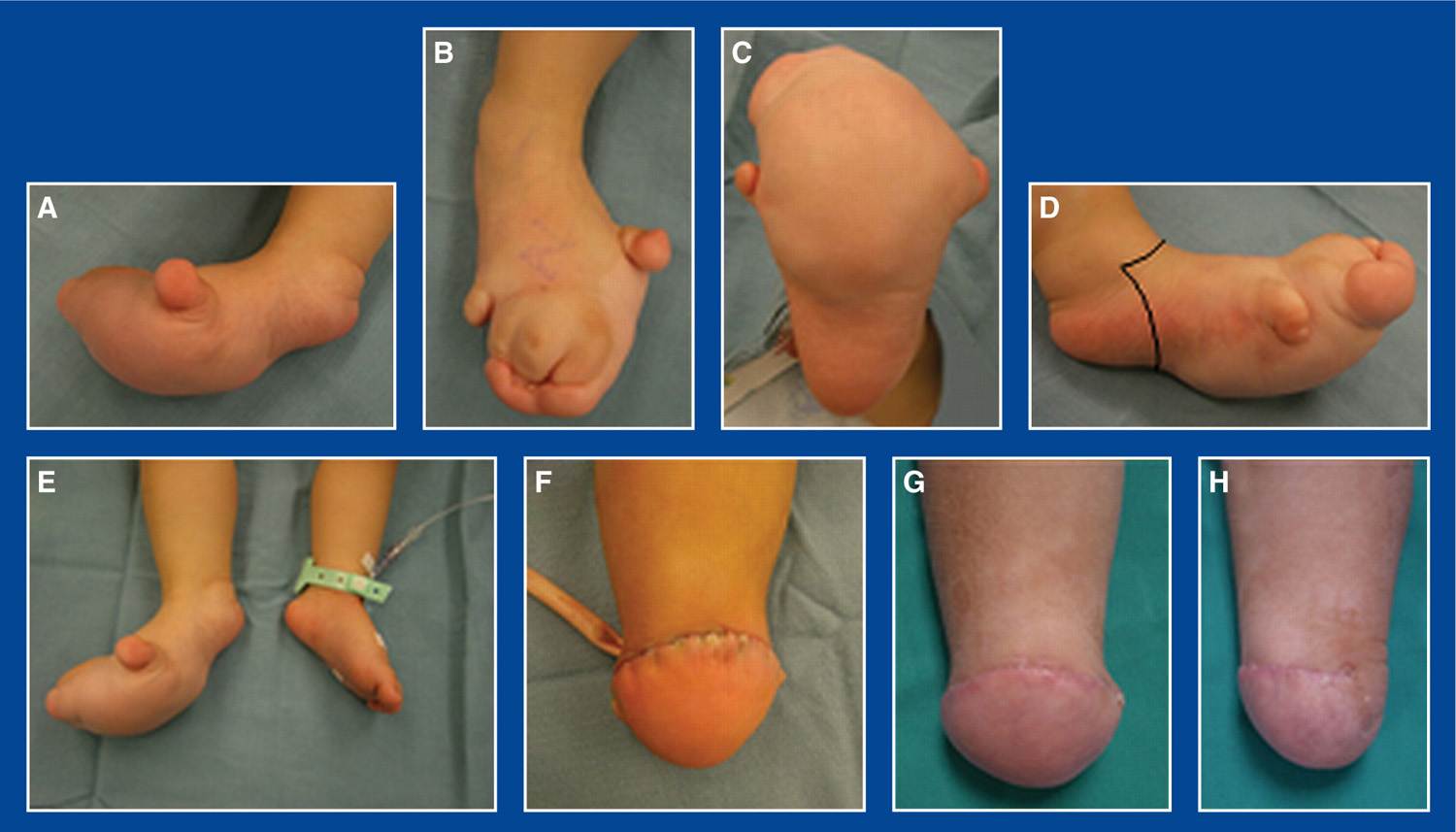
Figure 6-7. Macrodactyly or local gigantism (I have treated four of these). A. Medial view of the foot. B. Top view of the foot. C. Plantar view of the foot. Note the fairly sharp transverse demarcation between the enlarged forefoot soft tissues and the normal hindfoot soft tissues. D. Lateral view of the foot. Standard incision for a Syme amputation is indicated. It happens to cross the plantar surface of the foot immediately posterior to the pathologically enlarged soft tissues. E. Comparison view of feet confirms the need for ablation. F. Front view immediately after the Syme amputation. G. Front view of the residual limb 9 months later. Desirably bulbous, though not pathologic, heel pad is well centered under tibia. H. Side view of residual limb with heel pad well centered, i.e., slightly anterior to directly distal to the end of the tibia, anticipating slight posterior migration over time.
2. Elucidation of the segmental deformities
a. Linear and circumferential enlargement of the bones and soft tissues along one or more adjacent rays of the foot, usually including or exclusive to the 2nd ray
b. The enlargement of the bones and soft tissues is greatest distally, decreases in a gradual fashion proximally, and rarely extends proximal to the tarsometatarsal joint(s)
c. Enlargement of the entire forefoot or the entire foot is perhaps best called localized gigantism (Figure 6-7)
d. There is medial–lateral splaying and dorsal–plantar thickening of the forefoot due to a mass effect
3. Imaging
a. Simulated standing or standing AP and lateral of the foot
4. Natural history
a. Progressive enlargement of the affected bones and soft tissues, either proportionately or disproportionately faster than the normal adjacent tissues
b. It is impossible to remove all of the abnormal soft tissues, as there is no distinct line of demarcation. Furthermore, it might be impractical to do so even if it were possible. Any remaining abnormal soft tissues will grow faster than the adjacent normal tissues, possibly requiring subsequent and perhaps sequential soft tissue debulking operations (Figure 6-8).
5. Nonoperative treatment
a. Accommodative shoe wear. This is rarely, if ever, an acceptable option.
6. Operative indications
a. Anticipated and actual difficulty in fitting comfortably into normal shoes
b. Objectionable appearance
i. The appearance of the foot after surgery is never normal, but it is usually better than the original appearance. More importantly, more normal shoe wear is possible.
7. Operative treatment with reference to the surgical techniques section of the book for each individual procedure
a. Individualized treatment
i. Be creative
ii. Be aggressive
• It is impossible to remove all of the pathologic soft tissues with a segmental resection, even with a ray resection. There is no demarcation between the pathologic and normal soft tissues.
• The residual pathologic soft tissues will continue to grow disproportionately larger circumferentially than the adjacent normal soft tissues.
• It is almost guaranteed that a second operation will be required in the future to debulk the progressively enlarging/enlarged soft tissues (Figure 6-8).
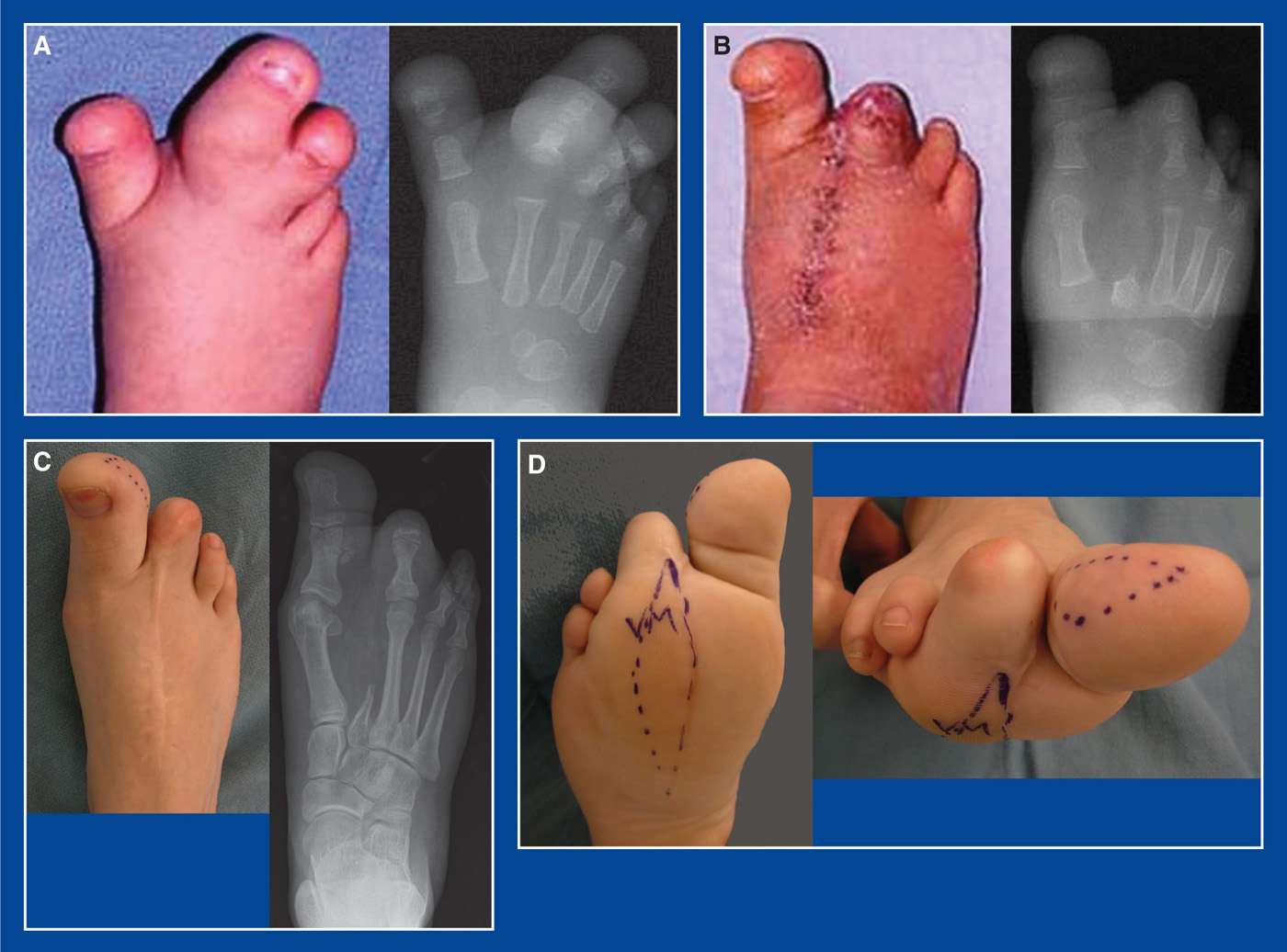
Figure 6-8. Macrodactyly. A. Top view and AP x-ray of the right foot in a 1-year-old girl. B. Top view and AP x-ray after 2nd ray resection and 3rd toe distal interphalangeal disarticulation. C. Top view and AP x-ray at age 17 years. There has been no change in the width of the foot. D. Remaining pathologic soft tissues at the margins of the resection site on the plantar surface of the forefoot grew faster than the adjacent normal soft tissues. This created a painful and callused “keel” that required resection. Painful enlarged soft tissues on the lateral side of the hallux were resected concurrently.
b. Ray resection (Figure 6-8; see Chapter 8)—perform this for enlargement of an entire ray. This is the most important and successful of the proposed procedures used to treat macrodactyly.
c. Interphalangeal joint disarticulation (Figure 6-8)—perform this if there is no enlargement of the MT or the soft tissues around the MT.
i. Disarticulate at the interphalangeal (IP) joint that will make the length of the residual toe equal to that of the adjacent lesser toe.
ii. Do not perform an MTP joint disarticulation, because the adjacent toes will drift toward each other, creating joint incongruity.
d. MT epiphysiodesis
i. It is challenging to calculate the timing for this procedure.
ii. Does not address the main disability of macrodactyly, which is the circumferential enlargement of the soft tissues
e. MT shortening—perform this after skeletal maturity for a painful transfer stress lesion under the MT head of an elongated metatarsal.
i. Does not address the circumferential enlargement of the soft tissues
f. Subsequent and sequential soft tissue debulking (Figure 6-8)—perform this for pain and progressive difficulty with shoe fitting due to circumferential enlargement of the soft tissues
g. Syme amputation (see Chapter 7)—perform this for enlargement of the entire forefoot (Figure 6-7)
h. Below-the-knee (transtibial and fibular) amputation—perform this for gigantism of the entire foot
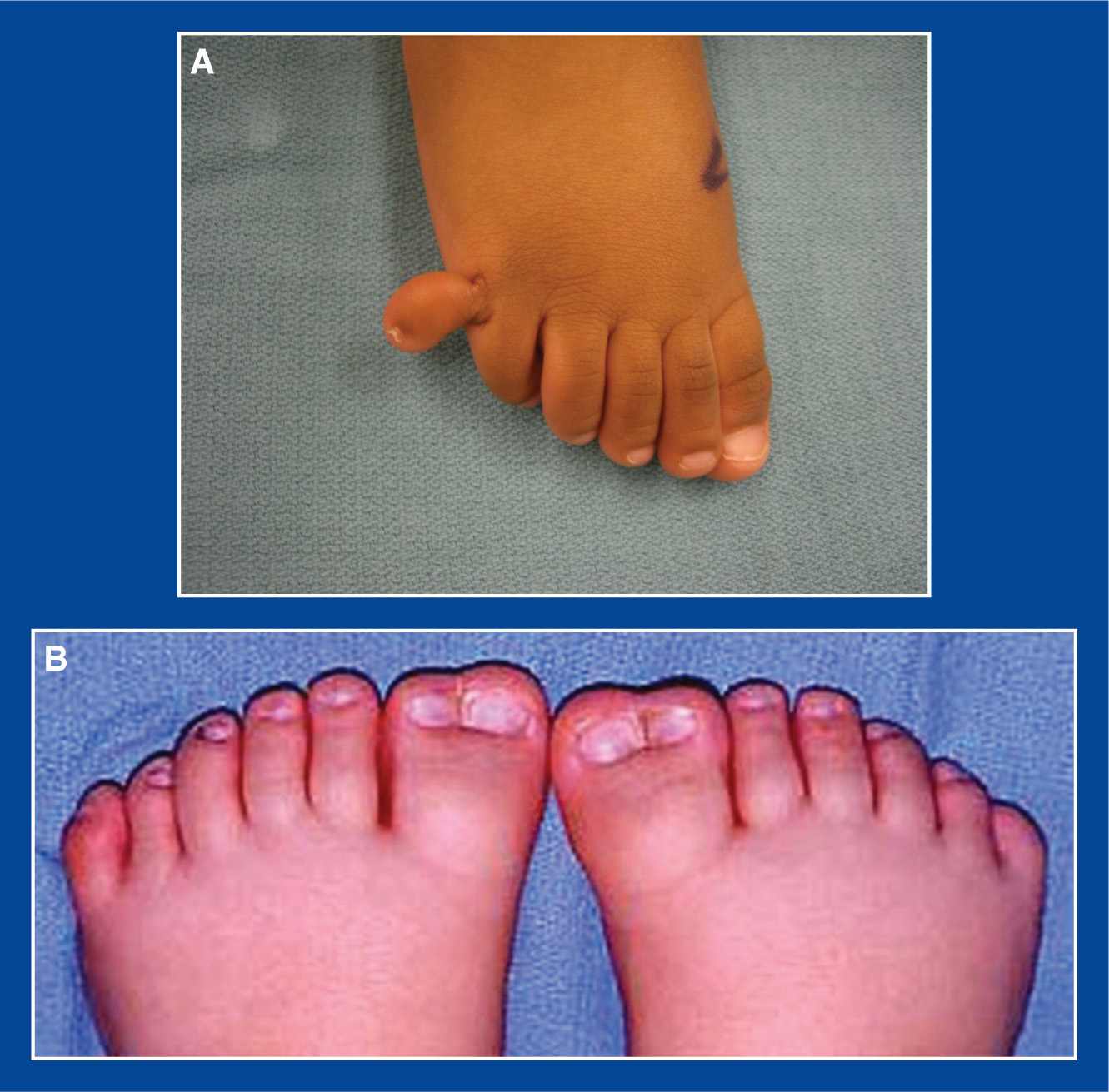
Figure 6-9. The extreme presentations of polydactyly. A. Postaxial polydactyly with only soft tissue and no bone or joint connection to the rest of the foot. B. Both feet have five well-formed lesser toes and MTs along with preaxial simple polysyndactyly consisting of complete duplication of the hallux and 1st MT bones.
1. Definition—Malformation, “Too many” (see Table 1-1, Chapter 1)
a. More than 5 complete toes per foot (Figure 6-9)
b. Foot polydactyly is associated with hand polydactyly in 34% of cases
c. Sporadic (most common) and hereditary types exist
d. More than 1 extra digit per foot, especially if combined with syndactyly, is often the manifestation of a syndrome, such as Greig cephalopolysyndactyly (autosomal dominant) (Figure 6-10)
2. Elucidation of the segmental deformities
a. Duplication of all or part of a toe, starting distally, and with or without segmentation/separation of the duplicate part(s)
b. There may be widening and partial duplication without separation (double scoop) of the distal MT epiphysis, with one toe articulating with each half (Figure 6-10). This is frequently seen in the 5th MT with postaxial polydactyly.
c. There may be complete duplication and separation of the distal end of the “normal” MT, creating a Y or T shape with each limb articulating with a toe.
d. The duplicated toe may be associated with, and articulate with, a partially or completely duplicated MT (Figure 6-11).
e. The duplicated toe may be separate or conjoined to an adjacent toe by soft tissue (simple syndactyly) or bone (complex syndactyly).
f. There may be conjoined or separate duplicated toenails with syndactylized toes.
g. Preaxial (great toe or medial border)—9% of the total (Figure 6-12)
i. often associated with LEB of the 1st MT (see this Chapter)
h. Central—6% of the total.
i. These occur most commonly between the normal 4th and 5th rays. There is a partially formed MT with a synchondrosis to the 4th MT. And in many cases, there is osseous syndactyly/synostosis of the proximal phalanx to the 5th toe proximal phalanx (Figure 6-11)
i. Postaxial (5th toe or lateral border)—85% of the total
i. A commonly seen presentation is polysyndactyly. There is often duplication of the toenails (with or without segmentation), duplication of the distal and middle phalanges, but with a single proximal phalanx. All parts are contained within a single soft tissue envelope that has simple syndactyly to the normal 4th toe. Neither middle phalanx lines up axially with the proximal phalanx (Figure 6-13).
3. Imaging
a. Simulated standing or standing AP and lateral of foot
4. Natural history
a. Difficulty fitting comfortably in normal shoes due to excessive width of the toes in relation to the width of the shoe
5. Nonoperative treatment
a. Wide shoes
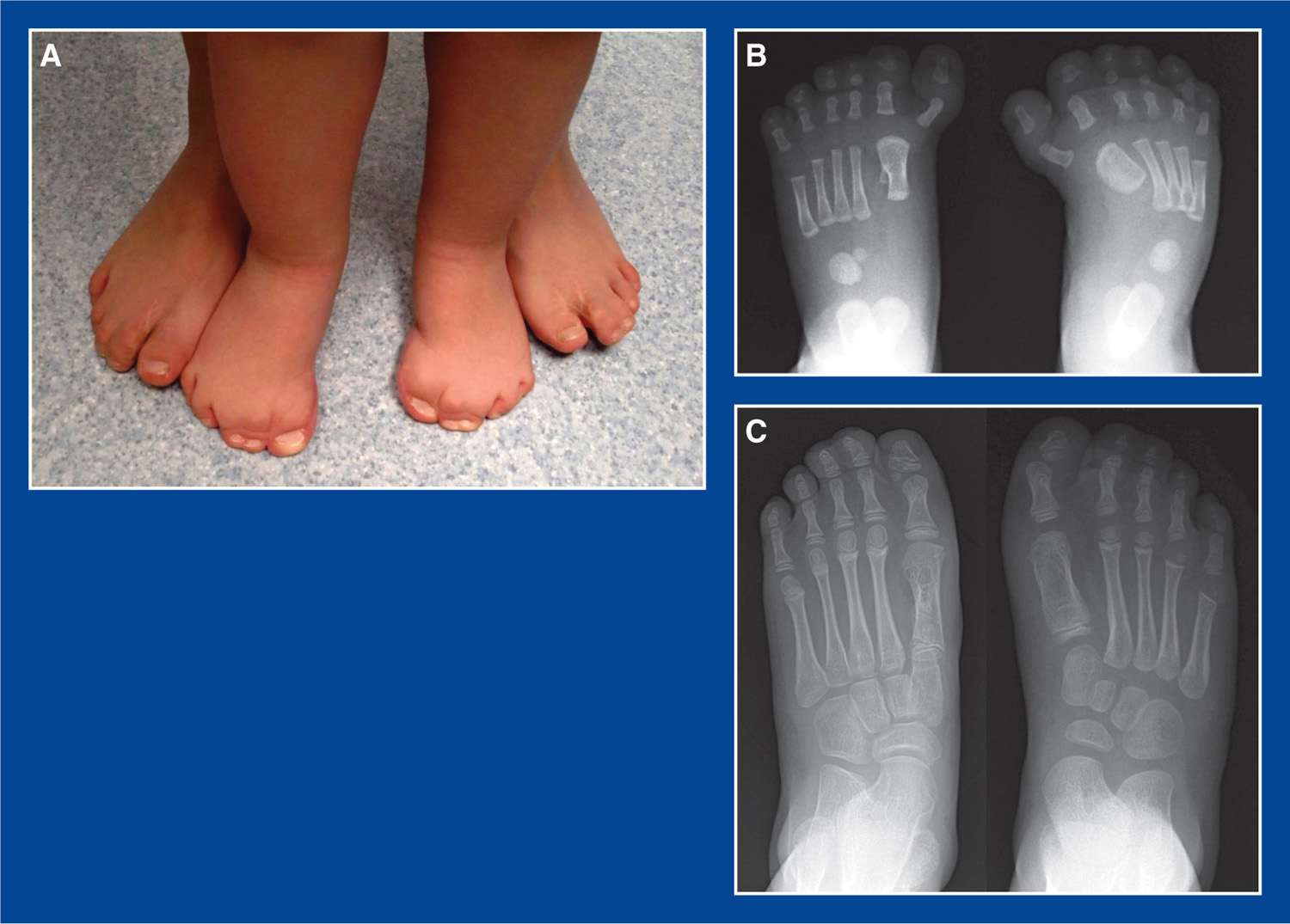
Figure 6-10. Greig cephalopolysyndactyly. A. The feet of mother and affected daughter with this autosomal dominant condition when the girl was 5 years old. B. AP x-rays of the girl’s feet taken when she was an infant. At 10 months of age, she underwent resection of the left duplicate hallux and shaving of the enlarged 1st MT head, and resection of the right duplicate hallux and the 1st MT longitudinal epiphyseal bracket. C. AP x-rays of her feet taken at age 6 years, showing nearly normal appearances of both feet, including normal growth of the right 1st MT.

Figure 6-11. A. AP x-ray of a foot in a 3-year-old child with isolated central polysyndactyly between the 4th and 5th rays. There is a congenital synchondrosis of the partially formed duplicate MT to the normal 4th MT shaft, and a congenital synostosis of the duplicate proximal phalanx to the normal proximal phalanx of the 5th toe. This is one of the most common patterns of polydactyly that I have seen in recent years. B.Normal radiographic appearance of the foot 3 years after a ray resection. Separation of the proximal phalanges did not injure the physis of the 5th toe.
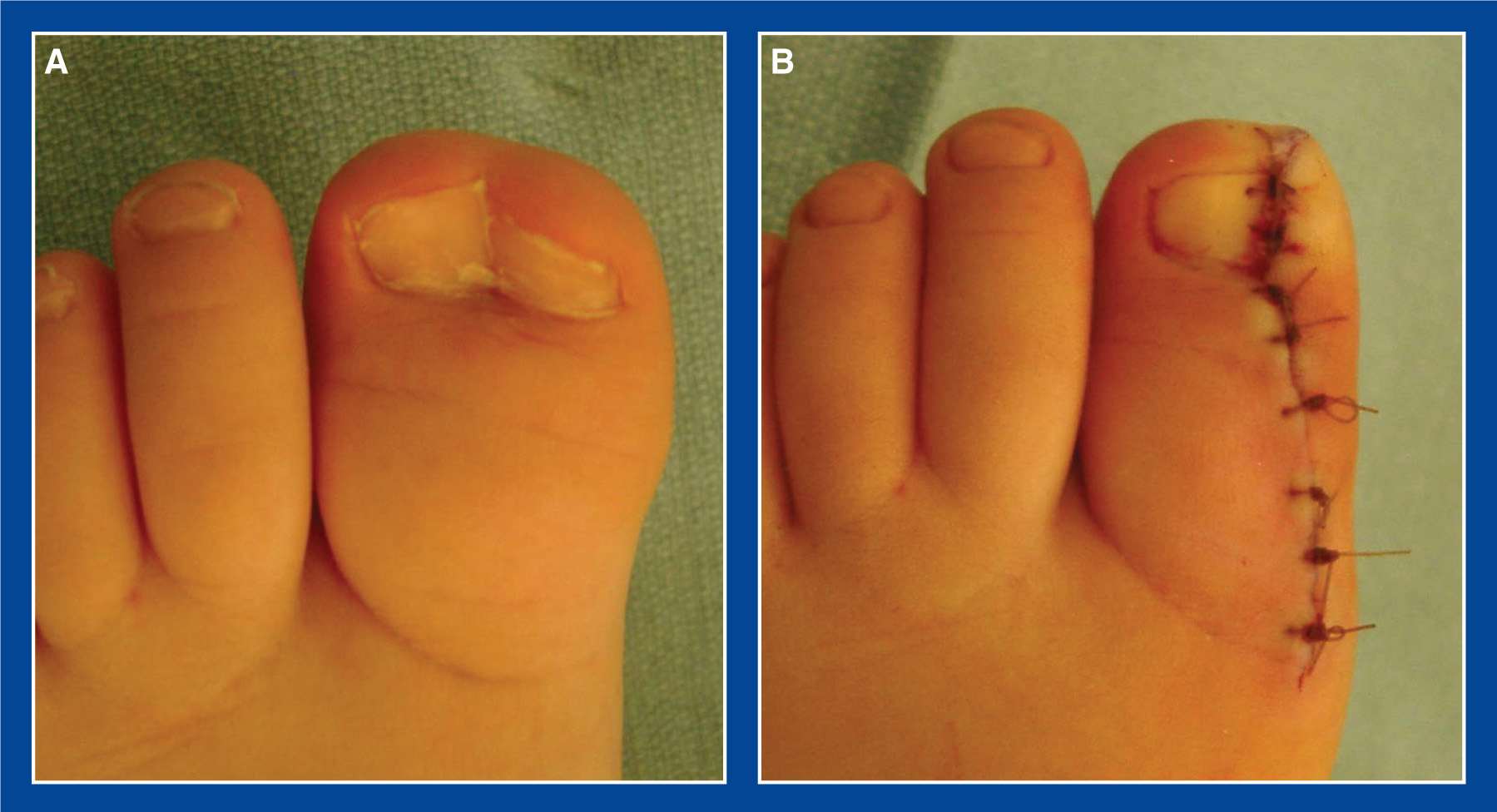
Figure 6-12. A. Preaxial polysyndactyly with a normal 1st MT. B. Appearance immediately after resection of the duplicate distal and proximal phalanges and toenail. A medial nail fold was carefully re-created with 4-0 chromic sutures.

Figure 6-13. Postaxial polysyndactyly. A. This is one of the most common patterns of polydactyly. The duplicate toenails are segmented (adjacent, but separate) in this case. The planned elliptical incision is marked. B. X-ray shows a single proximal phalanx and 2 middle phalanges, neither of which is aligned axially with the proximal phalanx. C. Intraoperative mini-fluoroscopy image shows the longitudinal osteotomy that was performed in the lateral duplicate middle phalanx. If the entire duplicate middle phalanx were removed, there would be instability at the proximal interphalangeal joint. D. Appearance of the toe after wound closure. 4-0 chromic sutures were used to enable the creation of a lateral nail fold that will prevent toenail ingrowth in the future. E. A soft tissue dressing is used following this short-duration day-surgery procedure. The child can bear weight immediately. The dressing is removed after 1 week.
6. Operative indications
a. Difficulty or anticipated difficulty fitting comfortably in normal shoes
b. Objectionable appearance
7. Operative treatment with reference to the surgical techniques section of the book for each individual procedure
a. Remove/disarticulate the abnormal (least well-aligned) toe through an elliptical skin incision
i. It is both important and safe to create a Salter–Harris IV fracture-type resection of a partially duplicated and nonsegmented 5th MT head when removing an associated duplicated lateral toe (and certainly safe to resect the wide portion of a partially duplicated and nonsegmented 1st MT head (Figure 6-10) where no physis exists).
b. Perform a ray resection (see Chapter 8) if an associated partially or completely duplicated MT is present (Figure 6-11)
c. Remove the limb of a Y- or T-shaped MT along with the toe with which it articulates
i. Perform a concurrent angular deformity corrective osteotomy of the residual MT for severe angular deformity
ii. or delay/avoid the osteotomy if only a minor angular deformity exists, as it might correct spontaneously over time
d. For polysyndactyly, remove the abnormal (least well-aligned) toe/toe parts/toenail through a dorsal elliptical incision; create a soft tissue lateral nail fold (Figures 6-12 and 6-13)
i. When neither duplicated middle phalanx aligns with a single proximal phalanx, it is appropriate to longitudinally split the middle phalanx that is being removed, leaving the articular portion in the proximal interphalangeal joint rather than destabilizing the joint by removing the entire middle phalanx (Figure 6-13).
e. Concurrently resect a LEB (see Chapter 8), if one exists
f. Perform a percutaneous tenotomy of a contracted flexor digitorum longus tendon slip to the 4th and/or 5th toe if one exists (see Chapter 7); a common finding in postaxial polydactyly
g. Do not separate 4th–5th toes syndactyly when associated with 5th toe polydactyly for the following reasons:
i. It is dangerous to the vascularity of the remaining digit when both sides of the digit are operated on concurrently.
ii. There are no functional or cosmetic advantages (the scar is less cosmetic than the syndactyly) achieved with separation of any toes, particularly the lateral toes (Figure 6-14).
iii. Finally, there is a reasonably high risk of lateral drift of the lateral toe, which would cause pain and shoe-fitting difficulties—for which the treatment would be to re-create the syndactyly (Figure 6-14)!
h. If a complete duplicate lateral 6th ray is resected, attach the peroneus brevis to the base of the 5th MT with sutures through drill holes.
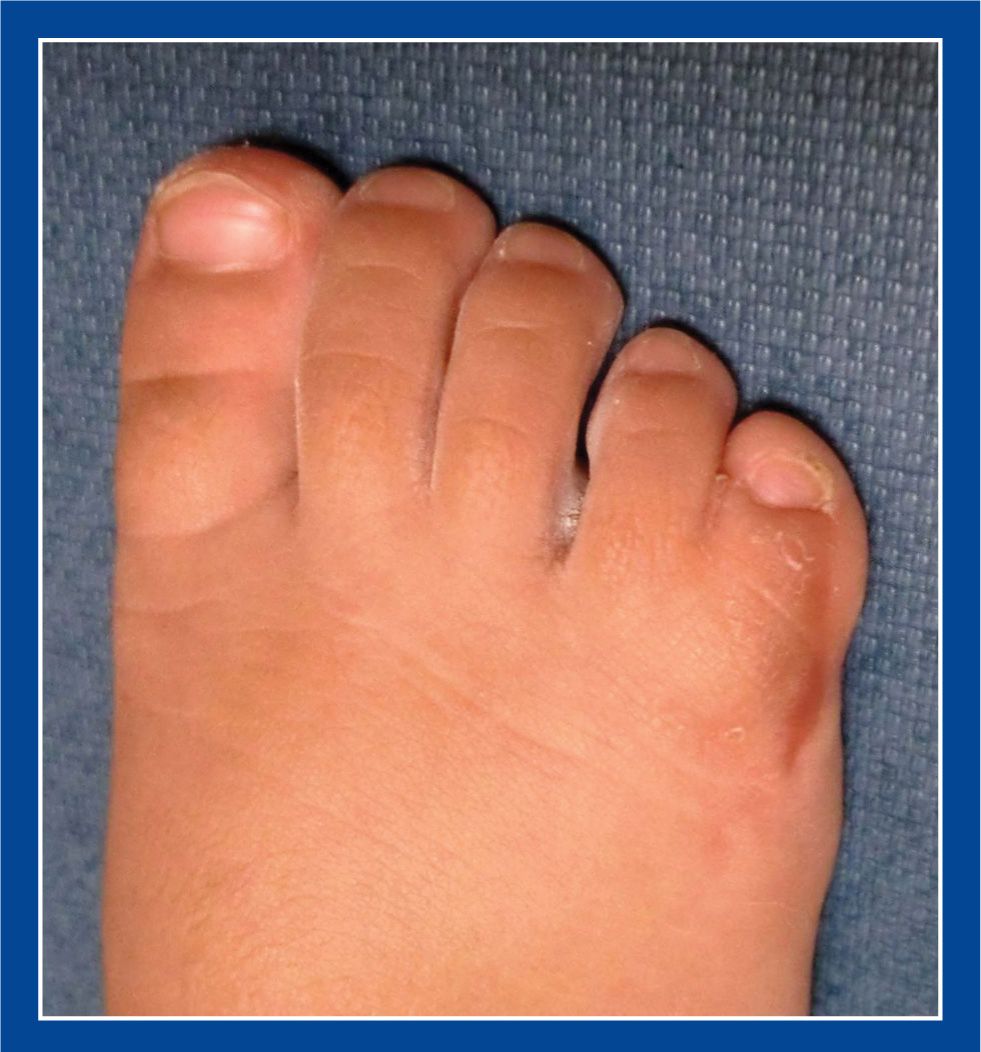
Figure 6-14. Excellent cosmetic appearance of postaxial polysyndactyly several years following resection of the duplicate lateral middle and distal phalanges and toenail, with maintenance of the simple syndactyly to the 4th toe. Also note the excellent cosmetic appearance of the surgically constructed lateral nail fold.
1. Definition—Malformation, “Joined together (failed to separate)” (see Table 1-1, Chapter 1)
a. Congenital failure of segmentation/separation of adjacent toes or of extra toes (polysyndactyly)
b. Simple
i. Congenital failure of segmentation/separation of the soft tissues of adjacent toes or of extra toes.
ii. As an isolated malformation, it occurs most often between the 2nd and 3rd toes in normal children (Figure 6-15).
• may be shallow (very close to the normal web position), intermediate, or complete (out to the tips of the toes)
• often bilateral
• often familial
iii. If more than 1 syndactyly per foot, the syndactylies are often manifestations of a syndrome, such as Greg cephalopolysyndactyly (autosomal dominant).

Figure 6-15. Simple syndactyly between the 2nd and 3rd toes of both feet. These are a cosmetic difference and rarely, if ever, a cause of pain or disability.

Figure 6-16. A. Typical appearance of the toes of a child with Apert syndrome. There is syndactyly of all toes. B. X-ray shows simple (soft tissue) and complex (osseous) polysyndactyly. Multiple synostoses and tarsal coalitions are seen in the forefoot, midfoot, and hindfoot.
c. Complex
i. Congenital failure of segmentation/separation of the soft tissues and bones of adjacent toes or of extra toes
ii. Most often found in Apert syndrome or other syndromes (Figure 6-16)
d. Differentiate syndactyly from acrosyndactyly (acro means end or tip), a postseparation, acquired distal connection between toes that is due to an amniotic band (Streeter dysplasia) (Figure 6-17)
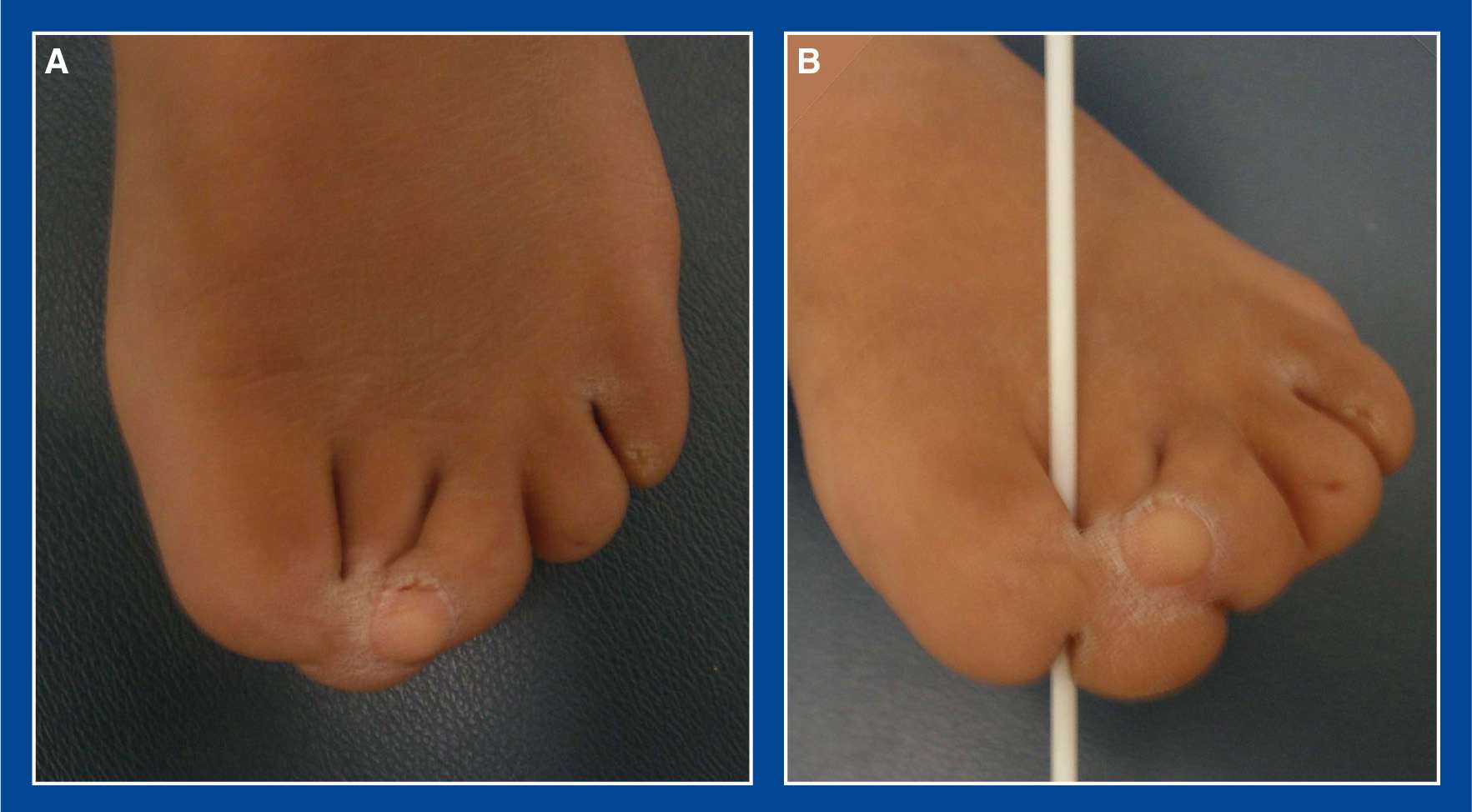
Figure 6-17. A. Acrosyndactyly due to amniotic band syndrome, a.k.a. Streeter dysplasia. B. Proximal separation is confirmed with a swizzle stick. Congenital syndactyly is a failure of separation. Acrosyndactyly, by way of contrast, is acquired and represents an injury to toes that have already separated in utero. The amniotic constriction band causes the developing fetal toes to unite or “spot weld” at the site of the band with amputation of the distal parts. Acrosyndactyly is neither a deformity nor a malformation, but instead an injury comparable to a burn.
2. Elucidation of the segmental deformities
a. Simple
i. Partial to complete (proximal to distal) failure of segmentation/separation of the soft tissue between 2 usually otherwise normal adjacent toes with normal bones, joints, tendons, neurovascular (NV) structures (though may be shared on the adjacent sides of the 2 toes), skin, nails.
b. Complex
i. Failure of segmentation/separation of the bones and soft tissues of 2 usually abnormal adjacent toes. The bones are frequently malformed as well as conjoined. Frequently, the joints are fused or ankylosed. The NV structures on adjacent sides of the toes are absent or malformed. Toenails are frequently unsegmented/conjoined.
3. Imaging
a. None for simple syndactyly
b. Simulated standing or standing AP and lateral of foot for complex syndactyly
4. Natural history
a. Simple
i. No pain or functional disability. The 2nd and 3rd toes typically grow at the same rate and achieve equal length. They perform identical tasks simultaneously that do not require independence.
ii. Rarely, if ever, pain may develop if differential growth in length of the toes causes joint flexion of the longer toe, with painful callus formation over the dorsum of the flexed IP joint(s).
• This can perhaps be anticipated in the unusual case of syndactyly between the hallux and 2nd toe.
b. Complex
i. Rarely a cause of pain or functional disability
5. Nonoperative treatment
a. None needed or indicated for simple syndactyly
b. Accommodative shoes for complex syndactyly and polysyndactyly which are often associated with other foot malformations, as in children with Apert syndrome
6. Operative indications
a. Simple
i. None
ii. Except perhaps if differential growth in length of the toes causes joint flexion of the longer toe and painful callus formation over the dorsum of the flexed IP joint(s)
b. Complex
i. Pain that is directly related to the bony syndactyly. Occasionally, the joints spontaneously fuse in poor alignment (often plantar flexion of the 2nd MTP joint), creating poor plantar pressure distribution and soft tissue overload.
7. Operative treatment with reference to the surgical techniques section of the book for each individual procedure
a. Syndactyly release (separation of the toes)—perform this rarely, and only if there is painful callus formation over the dorsum of the flexed IP joint(s) of the longer toe in the clinical scenario in which the syndactylized toes have grown at different rates and to different lengths.
i. The alternative, and perhaps preferred, treatment in this clinical scenario is to resect and fuse the painful, flexed IP joint(s).
b. Anecdotally, I have seen a few children who had undergone syndactyly release between the hallux and 2nd toe with the goal of wearing thong-type sandals. The scars, in all cases, were too hypersensitive to enable the children to wear thong sandals comfortably. There was also web creep that re-created much of the syndactyly over time.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








