Foot and Ankle
Julie E. Adams
Joseph R. Cass
Harold Kitaoka
ANATOMIC CONSIDERATIONS
The ankle is stabilized by anatomic congruence of the talus in the mortise as well as the strong ligaments and capsular attachments. The medial ligaments coalesce into a strong single ligament known as the deltoid ligament (1,2). It has superficial and deep fibers (1,2). The lateral collateral ligament is comprised of three discrete components; the anterior talofibular ligament, the calcaneofibular ligament, and the posterior talofibular ligament (1,3). The thin anterior talofibular ligament is most commonly disrupted with ankle sprains. Other stabilizers of the ankle joint include the syndesmosis and interosseous membrane.
Soft Tissue Anatomy
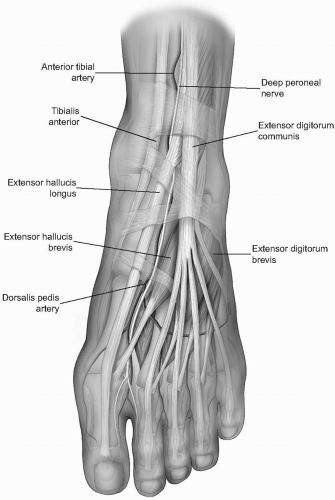
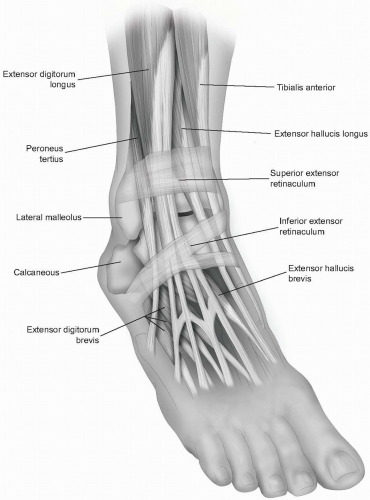
The muscles of the foot may be divided into the intrinsic muscles, whose origins and insertions lie in the foot, and extrinsic muscles, whose bellies lie proximal and tendons extend into the foot to exert their influences. Plantarly, the musculature of the foot is arranged in four layers, from plantar to dorsal: (a) abductor hallucis, flexor digitorum brevis, abductor digit minimi; (b) flexor digitorum longus, flexor hallucis longus, quadratus plantae, and the lumbricals; (c) flexor digiti minimi brevis, adductor hallucis, flexor hallucis brevis; and (d) the four dorsal and three plantar interossei muscles. Dorsally, the extensor digitorum brevis and extensor hallucis brevis lie in a relatively superficial plane (Fig. 11-1).
Overlying the tendons of the ankle are the retinacula, which prevent bowstringing of the tendons. The superior extensor retinaculum lies anteriorly and is split by the tibialis anterior tendon. The inferior extensor retinaculum lies over the dorsum of the foot and is Y shaped. It stretches from the lateral os calcis to the medial malleolus and to the plantar aponeurosis (Fig. 11-2). The flexor retinacula are lateral and consist of the superior peroneal retinaculum, which is a thickening of deep fascia stretching from the tip of the lateral malleolus to the calcaneus, and the inferior peroneal retinaculum, which crosses from the peroneal tubercle to lateral calcaneus.
The potential internervous planes include medially, between the tibial nerve innervated flexors (tibialis posterior) and the deep peroneal nerve innervated extensors (tibialis anterior); posterolaterally between the flexors (flexor hallucis longus) and the superficial peroneal nerve innervated everters (peroneus brevis); and laterally, between the extensors (peroneus tertius) and the everters (peroneus brevis) (4).
Neurovascular Anatomy
Anteriorly, the anterior tibial artery and the deep branch of the peroneal nerve course toward the foot, crossing the ankle joint midway between the malleoli (see Fig. 11-1) (4, 5, 6). The anterior tibial artery lies between the tibialis anterior tendon and the extensor hallucis longus proximal to joint and then between the extensor hallicus longus (EHL) and the extensor digitorum longus (EDL) distal to the
joint. It becomes the dorsalis pedis artery distally as it enters the foot. The deep peroneal nerve supplies the extensor digitorum brevis (EDB) and extensor hallucis brevis and provides cutaneous sensation to the first web space.
joint. It becomes the dorsalis pedis artery distally as it enters the foot. The deep peroneal nerve supplies the extensor digitorum brevis (EDB) and extensor hallucis brevis and provides cutaneous sensation to the first web space.
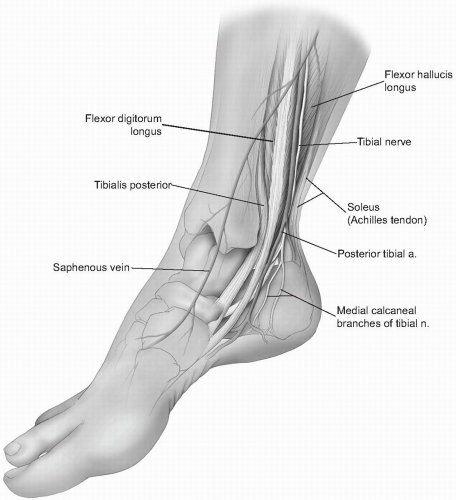
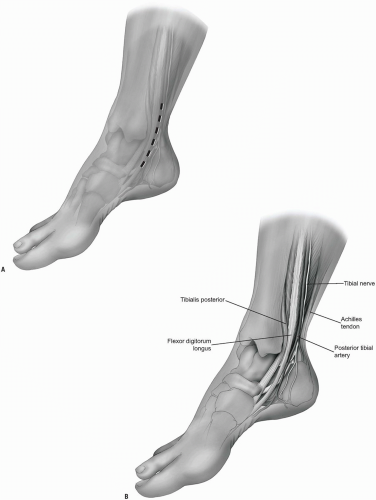
Posteromedially, the neurovascular bundle includes the posterior tibial artery and the tibial nerve and courses posterior to medial malleolus, lying between the tendons of the flexor digitorum longus (FDL) and flexor hallucis longus (FHL) (Fig. 11-3). The posterior tibial artery passes behind the tendon of the flexor digitorum longus before entering the sole of the foot and dividing into medial and lateral plantar arteries. Analogous to the hand, the lateral plantar nerve supplies sensation to 1.5 digits, while the medial plantar nerve supplies 3.5 digits (1,3).
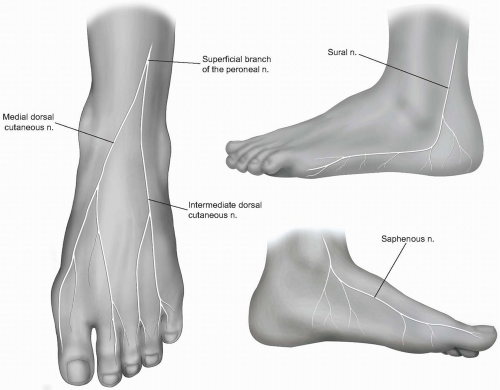
Several superficial structures are important to identify and preserve. The saphenous nerve, the terminal branch of femoral nerve, runs with the long saphenous vein anterior to medial malleolus. Proximally, it pierces the deep fascia between the sartorius and gracilis tendons. The branches of the nerve are closely associated with those of the long saphenous vein throughout their courses. The saphenous nerve passes anterior to the medial malleolus to provide cutaneous sensation to the medial first ray and base of the big toe. The nerve divides into two branches at the level of the medial malleolus and thus supplies sensation to the medial midfoot as well (Fig. 11-4).
The superficial peroneal nerve is a terminal branch of the common peroneal nerve. It pierces the deep fascia of the anterior compartment at the distal one-third of the leg and distally crosses the ankle anteriorly at the mid-malleolar line. It is superficial and lateral to the anterior tibial neurovascular bundle. It divides into the medial and intermediate dorsal cutaneous nerves, which provide sensation to the dorsum of the foot (see Fig. 11-4).
The sural nerve is the terminal branch of tibial nerve and runs over the lateral aspect of the leg and foot, posterior to the lateral malleolus. It pierces the deep fascia in the posterior calf then travels distally, lateral to the Achilles tendon. The sural nerve travels with the short saphenous vein, with which its branches are closely bound. Its path curves anteriorly distal to the lateral malleolus along the fifth
ray to finally become the lateral dorsal cutaneous nerve of the foot and provides sensation to the lateral aspect of the foot (see Fig. 11-4) (1,2,4,5).
ray to finally become the lateral dorsal cutaneous nerve of the foot and provides sensation to the lateral aspect of the foot (see Fig. 11-4) (1,2,4,5).
APPROACHES TO THE DISTAL TIBIA/ANKLE JOINT (5,7-10)
Anteromedial Approach to the Distal Tibia/Ankle Joint
Indications
The standard anterior approach to the ankle joint involves entering via the plane between the tibialis anterior medially and the neurovascular bundle and toe extensors laterally. This works well for intraarticular ankle procedures but not as well for distal tibial fracture reduction and fixation. This anteromedial approach works well for medial plating and fractures of the distal tibia in which the medial side has failed in compression and requires plating and bone grafting.
Technique
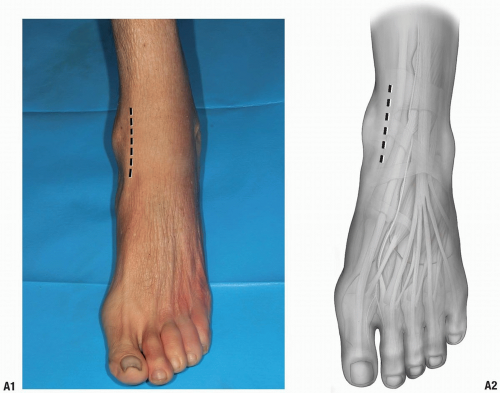
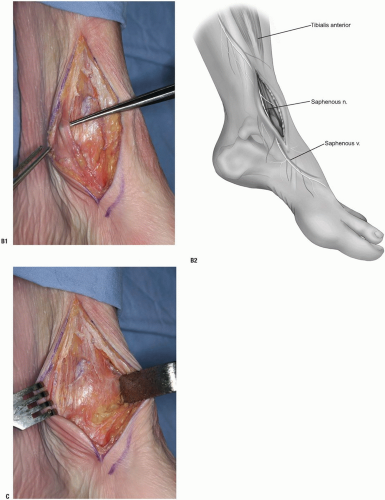
The incision is made medial, rather than lateral, to the tibialis anterior tendon (Fig. 11-5A).
That tendon is retracted laterally along with the other structures lateral to it. One must identify and preserve the saphenous nerve; otherwise the medial malleolus and medial distal tibia are well presented via this approach (Fig. 11-5B). The tubercle of Chaput is not as well visualized via this approach, however.
The knee retractor may be utilized to retract the anterior tibial tendon laterally and the ankle capsule is readily visible (Fig. 11-5C).
Anterolateral Approach to the Distal Tibia/Ankle Joint
Indications
Pilon fractures with compression failure laterally can be easily exposed anterolaterally. This is an excellent exposure for application of anterolateral periarticular plates. The interval is defined by retracting the extensors of the ankle and toes medially along with the neurovascular bundle.
Note: One has to watch out for the superficial peroneal nerve as it crosses the fibula and proceeds distally and medially. The peroneus tertius is a part of the extensor digitorum communis.
Note: This anterolateral exposure has been described both as between the tertius and communis tendons, or lateral to those tendons.
Technique
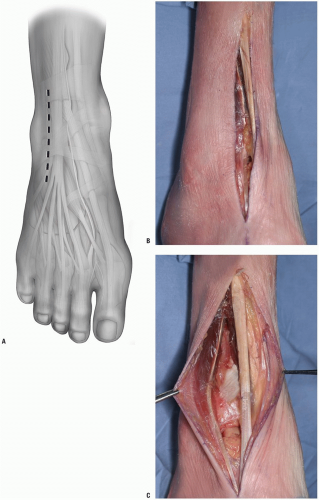
The incision is made in line with the fourth metatarsal distally (Fig. 11-6A). It is a straight incision, crossing the ankle joint.
Note: It can be extended proximally as necessary, freeing up the anterior compartment muscles as necessary. It can be extended distally and allows access to the dorsal lateral aspect of the talar neck as well, if necessary.
After incising the skin, the retinaculum is encountered and incised as well (Fig. 11-6B). The tendons and neurovascular structures are identified (Fig. 11-6C).
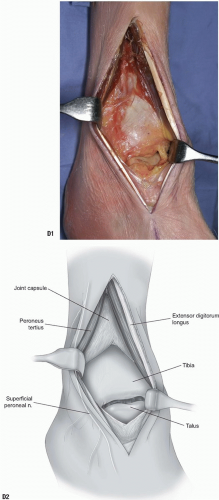
The extensor muscles are retracted laterally and the peroneus tertius medially.
With retraction, the joint and anterior distal tibia are easily observed. The superficial peroneal nerve is behind the lateral retractor along with the peroneus tertius tendon (Fig. 11-6D).
Posteromedial Approach to the Distal Tibia/Ankle Joint
Indications
Occasionally it is necessary to approach the tibia or the talus via a posterior medial approach, usually for medial malleolar fractures or possibly to expose the talus with a medial malleolar osteotomy.
Position
This can be accomplished with the patient prone or supine. If the patient is positioned supine, a bump can be placed under the opposite hip. The ipsilateral leg is then flexed and externally rotated.
Technique
The incision is made at approximately the midpoint between the Achilles tendon and the medial malleolus (Fig. 11-7A).
Note: The plane past the neurovascular bundle can either be via the flexor digitorum longus medially and the neurovascular bundle laterally, between the neurovascular bundle and the flexor hallucis longus, or by retracting the flexor hallucis medially and protecting the nerve and artery (Fig. 11-7B).
The malleolus is readily exposed by a periosteal elevator (Fig. 11-7C). One cannot directly visualize the intraarticular aspect of the distal tibia directly via this approach but it works well for indirect reduction techniques and also for posteromedial fractures of the talus.
Note: It is also possible, by making the incision more anteriorly over the posterior aspect of the medial malleolus, to access both the posterior distal tibia and the medial malleolus.
Release the cephalad attachments of the posterior tibial sheath (Fig. 11-7D) and retract the tendon distally and posteriorly.
The malleolus is osteotomized, and by retracting the malleolar fragment distally, the posterior reduction of the articular surface may be assessed (Fig. 11-7E).
Note: Both the tibial and talar articular surfaces are visible, along with the posterior tibia, through this approach. This approach works well for the supination-adduction type ankle fracture pattern where there is medial plafond depression that has to be elevated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree