11 Foot and ankle
CHAPTER CONTENTS
Introduction
This chapter will focus on some of the most common conditions of the foot and ankle seen in physical medicine practice. However, there is also a brief discussion regarding the reasons biomechanical faults can be an underlying causes of chronic overuse syndromes in the local soft tissues, as well as how these contribute to chronic conditions further up the kinetic chain (Hertel 2000; Rose et al 2000; Ryan 1994).
Additionally, patients are prescribed either prescription or over-the-counter anti-inflammatory medications to reduce further swelling and thereby relieve pain. Other sources of neutraceutical remedies are available, but are not discussed (Pizzorno et al 1997, 2005, Pizzorno & Murray 2007).
Acute inversion sprain
The early management is pivotal to the effective rehabilitation of an ankle sprain. Early conservative treatment should consist of partial weight-bearing, cryotherapy, bandage compressions, and elevation above heart height with non-steroidal anti-inflammatory treatment and exercises to prevent loss of range of movement (ROM). Failing this, chronic pain, loss of ROM, and swelling can persist with potential joint instability. It is well established that effective ankle rehabilitation must involve four main components (Balduini et al 1987; Kerkhoffs et al 2002; Van der Wee et al 2006), ROM rehabilitation, progressive muscle-strengthening exercises, proprioceptive training, and activity-specific training, as functional stress stimulates the production and orientation of stronger replacement collagen with eccentric strengthening and conditioning of peroneal muscles providing additional support to the lateral ligaments (Glick et al 1976) and assisting in the prevention of reoccurrences.
The diagnosis will depend on the extent of the disruption of the ligament and the supportive lateral muscles and tendons, especially tibialis anterior and the peroneii. The problem often leads to chronic instability and recurrent minor sprains. In addition to the standard PRICES approach to the management of the resulting pain and swelling, there are also manipulative and mobilization techniques that have been shown (Peterson & Bergmann 2002; Whitman et al 2005) to restore normal intra-articular motion and enhance healing in both acute and chronic recurrent inversion ankle sprains (Gillman 2004).
Manipulation or mobilization is practised by manual therapists and has been shown to decrease joint pain and normalize function. The mechanisms of action are not well understood. Current theories propose that an imbalance of muscle activity is the source of pain. Manipulation can relieve this through reflexive actions and may be appropriate for early conservative care as part of a comprehensive treatment programme (Eisenhart et al 2007; Fryer et al 2002; Justus et al 2002). Eisenhart et al (2007) compared two groups of patients undergoing emergency ankle treatment in which one group was allocated to standard care and the other to standard care and osteopathic manipulation treatment (OMT). Both groups were found to have significant improvement, but the OMT group demonstrated significant (f = 5.92; p = 0.2) improvement in pain, oedema, and ROM.
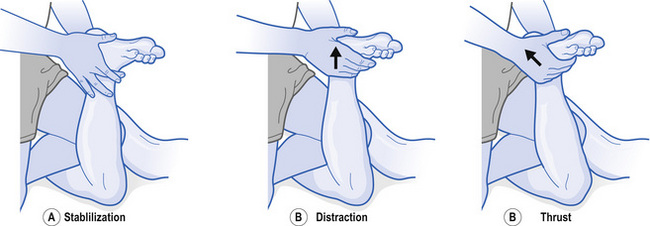
An inversion sprain/strain injury can result in a talus that is mal-positioned and fixed in both anterior and lateral positions. Fig. 11.1 demonstrates one method for adjusting an anterolateral talus.
It has also been suggested that the incorporation of manipulation of the lumbar spine and pelvis, as well as the hip and knee, can help to ensure normal circulation and nerve integrity in order to optimize healing (Logan & Row 1995). It is important to note that extremity manipulation techniques require a great deal of skill and training in order to be applied safely in acute or chronic circumstances.
Achilles tendinopathies (acute and chronic)
The achilles tendon can sustain either acute traumatic or chronic overuse injuries depending on the mechanism of injury. An acute strain of the achilles tendon results from a rapid tensile stress placed on the tendon that causes tissue disruption (Fig. 11.2). Like the ankle sprain, this injury is graded as mild, moderate, or severe. Achilles tendinopathy is prevalent and potentially incapacitating in athletes involved in running sports. It is considered to be a degenerative, not an inflammatory condition (Kader et al 2002). Severe cases may respond to conservative care, but sometimes require surgical intervention. However, mild and moderate cases will respond to conservative care using the PRICES protocol. In addition, the use of temporary heel lifts will relieve some of the tensile stress in the tendon during recovery. If a heel lift is to be used it is important to note that there should be a lift of equal size under both extremities to avoid an artificial leg length inequality and potential injury to the joints further up the kinetic chain.
The exact aetiology and pathogenesis of tendon pain is not fully understood (Alfredson 2005; Shalabi et al 2004) and is undergoing much research at present. Recent studies have shown that there may be a genetic predisposition to suffering from a tendinopathy (Harvie et al 2004; Kannus & Natri 1997). Multiple intrinsic and extrinsic risk factors have been associated with achilles tendon injuries; suggesting this condition is complex and interactions between gene–gene and gene–environment are probably involved in the aetiology of these conditions (September et al 2007).
In association with tendon degeneration, there appears to be signs of neural inflammatory markers in nerves in close proximity to affected tendons (Hart et al 1995). The well-known neurotransmitter and potent modulator of pain in the central nervous system, glutamate, is found in high levels in painful tendons, but not in normal tendons (Alfredson et al 2001). In conjunction with neurovascular ingrowths into painful tendons as demonstrated by Bjur et al (2005), there is now evidence that neural pathways and neovascularization are associated with the pain of tendinopathy rather than just a simple case of tissue degeneration.
There appears to be a lack of research consensus on the efficacy of management of this achilles tendinopathy, but the lack of suitable evidence in support of a given management method does not necessarily imply a lack of clinical effectiveness (Andres et al 2008).
The following interventions have been demonstrated as providing clinical effectiveness:
The initial occurrence of an achilles tendon strain can subsequently result in chronic strains and/or tenosynopathy. When this occurs, the practitioner must consider the possibility of an underlying biomechanical weakness contributing to the chronicity of recurrent achilles tendinopathies. Chronic achilles tendinopathy (CAT) may result from chronic overuse of the tendon as a result of an underlying biomechanical weakness in foot and ankle function. Excessive and prolonged pronation through the rear foot is an example of this type of underlying biomechanical foot fault. As a result, the calcaneous undergoes excessive eversion during the gait cycle, causing a valgus stress through the medial aspect of the calcaneus and the distal attachment of the achilles tendon. This ultimately results in pain, oedema, and sometimes crepitus from overuse of the tendon and yields a tendinopathy. This overuse injury may be resolved with the use of the PRICES protocol, but will be recurrent if there is an underlying biomechanical weakness. The preferred option for the management of this condition is the addition of foot orthoses to the treatment plan (Alfredson & Lorentzon 2000). There is a further discussion of foot orthoses in the management of chronic overuse syndromes in the foot and ankle at the end of this chapter.
Plantar fasciitis
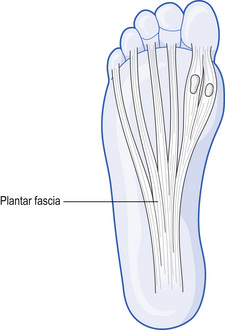
The plantar fascia is a connective tissue that is a cross between a tendon and a ligament. It attaches to the bottom of the heel and then spans the length of the foot, spreading out like a fan to connect with the distal metatarsals, as shown in Fig. 11.3. The function of the plantar fascia is to support the medial longitudinal arch (MLA) and control the pronation of that arch during normal gait.
When abnormal pronation occurs, the plantar fascia is repetitively and excessively stressed, causing a pain in the arch of the foot that is felt most keenly on the plantar and medial aspects of the calcaneus, at the calcaneal tubercle, although this pain can also extend along the full length of the foot. On histological examination, Lemont et al (2003) found increased fibroblasts, ground substance, and vascularity, but not significant inflammatory mediators.
In the light of any objective findings, including calf muscle length, talocrural hypomobility, forefoot pronation, and heel pain, treatment is encouraged to include a multifaceted approach that addresses underlying anatomical and biomechanical conditions (Dyck & Boyajian-O’Neill 2004). This can be the case with either an overpronated or oversupinated foot (Souza 2001); a classic sign of this condition is severe pain on walking in the morning that dissipates once the patient is up and moving about.
In addition to the PRICES protocol for the relief of symptoms, spray and stretch techniques that block the reflex spasm and sensation of pain have also been shown to be effective in the conservative treatment of PF. Other techniques, such as cross-friction, ischaemic compression, heat, and manipulation, are effective on their own, or in combination with the spray and stretch technique. Considering the referral pattern of trigger points (TrPts) of the gastrocnemius/soleus to the foot, passive stretching of these muscles leads to a better prognosis and reduces the likelihood of recurrence. Acupuncture has also shown to be effective with treatment of TrPts associated with PF (Steinmetz 1999). Taping techniques have been shown to be one of the most reliable and effective short-term treatments if used correctly. These can also be used to predict the success of orthotics and are important indicator of the specific goals of orthotic therapy (Cornwall & McPoil 1999). The inclusion of functional orthotic therapy (FOT) has been demonstrated to be an effective addition to management plans for acute and chronic PF (Bartold 2004; Dimou et al 2004; Martin et al 2001).
Metatarsalgia and Morton’s neuroma
Pain in the forefoot is often associated with, and is a precursor to, Morton’s neuroma. The patient will initially experience the insidious onset of forefoot pain that gets progressively worse if it goes untreated. If the condition is allowed to progress, this will eventually result in connective tissue formation (scarring) around the peripheral nerves of the foot, predominantly in the nerves between the second, third, and fourth digits of the foot. The patient may then experience paraesthesia in the toes along with secondary forefoot pain, referred to as entrapment neuralgia (Souza 2001).
The standard treatment involves the PRICES protocol with the addition of a metatarsal pad placed under the metatarsal arch to relieve pressure on the soft tissues between the distal metatarsals (Hassouna & Singh 2005; Nashi et al 1995). Footwear modifications may be required (e.g. a wider shoe) and wearing high-heeled shoes should be discouraged.
It is interesting to note that the underlying mechanism of this overuse injury is associated with overpronation through the rearfoot, midfoot, and forefoot changing the functional biomechanics of the metatarsal arch (Michaud 1997). Once again the incorporation of FOT along with pain management strategies can facilitate enhanced recovery.
Anterior and posterior tibial tendinopathy
Pain on the anterior or posterior aspect of the tibia is commonly referred to as ‘shin splints’. The posterior tibial muscle and tendon are attached along the posterior and medial aspect of the tibia, passing posteriorly to the medial malleolus and underneath the MLA and attaching to the plantar aspect of the tarsal bones of the foot, allowing it to support the MLA like a stirrup. The anterior tibial muscle and tendon are attached along the anterolateral aspect of the tibia and insert into the superior aspect of the mid-tarsal bones. When the muscle and tendon contract, there is a lifting of the superior aspect of the tarsal bones that contributes to the support of the MLA.
Bilateral asymmetrical pronation syndrome
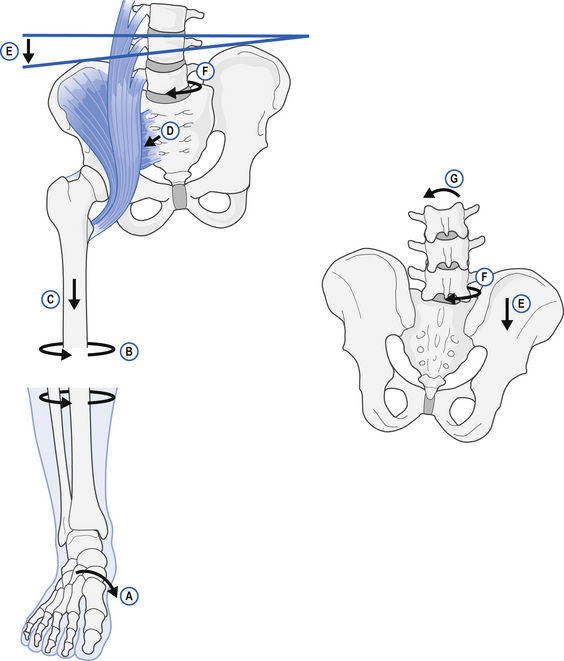
As noted above, many of these conditions are secondary to overpronation of the rear foot, medial longitudinal arch, or forefoot, secondary to faulty foot mechanics. The diagram in Fig. 11.4 demonstrates how rear foot and forefoot varus deformity present in the non-weight-bearing phase of the gait cycle becomes a valgus stress as the foot and ankle go from an inverted to everted position with weight-bearing. When this occurs repetitively, excessively, or for a prolonged period during a single gait cycle, the result is overuse of the soft tissues.
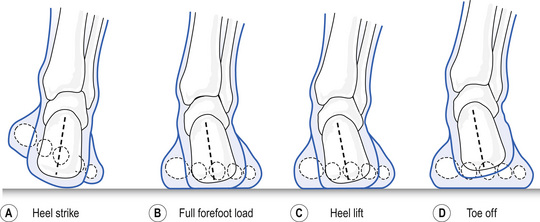
Figure 11.4 Stance phase motions. (a) Heel strike; (b) full forefoot load; (c) heel lift; (d) toe off.
This then is the underlying mechanism of the soft-tissue irritation in the plantar fascia that initially causes heel and arch pain; progressing to overstretching of the metatarsal arch and the development of metatarsalgia and eventually advances to Morton’s neuroma. Overuse of the anterior and posterior tibial tendons causes shin splints; excessive stretch of the medial aspect of the achilles tendon results in tendinopathy; and ultimately, this varus (inversion) to valgus (eversion) motion also contributes to torsional forces up through the kinetic chain of the knee, hip, and pelvic and spinal joints to cause chronic soft-tissue injury and joint dysfunction in these more proximal regions. The diagram in Fig. 11.5 illustrates how the overpronation in the foot:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree