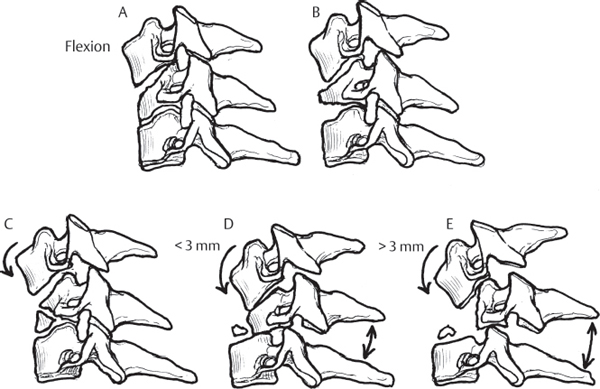
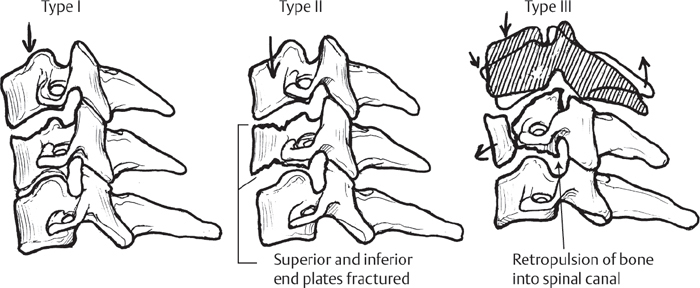
6 The classification of cervical spine injuries has evolved considerably in the last decade. Previous classification schemes have relied on assumptions based on imaging, injury mechanisms, and force vectors, with no one method being universally accepted. The most popular classification system used for compression injuries of the cervical spine was described by Allen et al. in 1982.1 This system is based on the interpretation of plain-film radiographs and clinical history and includes a comprehensive biomechanical classification system for each subtype of compression injury of the cervical spine. Compression-flexion injuries were most commonly due to motor vehicle or diving accidents. Adopting the terminology used for thoracolumbar fractures,2 the anterior column, consisting of the vertebral bodies and intervertebral disks, fails in compression, with variable failure of the middle column (posterior vertebral body) and posterior column (the facet joints and posterior ligamentous complex) in distraction. According to Allen and Ferguson, there are five stages of flexion-compression injuries (Fig. 6.1). Stage 1 involves rounding over of the superior endplate. Stage 2 involves further collapse of the endplate, with beaking, or anterior fracture, of the vertebral body. The middle and posterior columns are spared in these early stages. With progression to Stage 3, the well-known “teardrop” fracture is observed, with splaying of the posterior spinous processes and more significant coronal or sagittal fractures of the vertebral body. In Stage 4, there is mild (< 3 mm) retrolisthesis of the vertebral body into the spinal canal. The final stage, Stage 5, involves complete rupture of the posterior column in distraction, and retropulsion of bone into the spinal canal of 3 mm or more. These latter stages can also be termed cervical “burst” fractures. Fig. 6.1 Five stages of flexion-compression injuries. Vertical compression injuries are commonly caused by a direct blow to the head, such as occurs during a diving accident or from the largely abandoned technique of “spear-tackling” in football. In these injuries, divided into three stages by Allen et al.,1 failure occurs with progressive loading of a rigid segmental column (Fig. 6.2). Stage 1 involves a central depression fracture of the endplate. In Stage 2 injuries, both endplates are commonly involved, with fracture through the body. Injuries that involve displacement of the vertebral body into the spinal canal are classified as Stage 3, and are similar to the higher-stage flexion compression injuries. Lamina or facet fractures can occur in the higher stages. In 2007 the Spine Trauma Study Group developed a new classification system: the Subaxial Injury Classification (SLIC),3 which has since been validated as teachable and reproducible, with intra-observer reliability comparable to the Allen and Ferguson classification.4,5 This system offers a simple, reproducible way of incorporating information about the injury that is considered the most clinically relevant (Table 6.1). This classification system uses three main descriptors: injury morphology, integrity of the discoligamentous complex (DLC), and neurological status of the patient.3 The first category of injury morphology is compression, including loss of height and vertebral body fractures, and comprises injuries traditionally known as compression fractures, burst fractures, and “teardrop” fractures. Posterior or lateral element fractures can also occur if the spine experiences load in extension or lateral flexion. As the severity of the injury increases, the SLIC score increases as well. Translational injuries, including facet dislocations, are covered under a separate category. This system offers a more comprehensive and simpler method of classification than the Allen and Ferguson system. Fig. 6.2 Vertical compression fractures as staged by Allen and Ferguson.
Flexion-Compression Injuries of the Cervical Spine
![]() Classification
Classification
Points | |
Morphology | |
No abnormality | 0 |
Compression | 1 |
Burst | +1 = 2 |
Distraction (e.g., facet perch, hyperextension) | 3 |
Rotation/translation (e.g., facet dislocation, unstable teardrop or advanced stage flexion-compression injury) | 4 |
Discoligamentous complex (DLC) | |
Intact | 0 |
Indeterminate (e.g., isolated interspinous widening, MRI signal change only) | 1 |
Disrupted (e.g., widening of disk space, facet perch, or dislocation) | 2 |
Neurological status | |
Intact | 0 |
Root Injury | 1 |
Complete cord injury | 2 |
Incomplete cord injury | 3 |
Continuous cord compression in setting of neuro deficit (neuro modifier) | +1 |
Source: Vaccaro AR, Hulbert RJ, Patel AA, et al.: The Subaxial Cervical Spine Injury Classification System. A novel approach to recognize the importance of morphology, neurology, and integrity of the disko-ligamentous complex. Spine 2007;32:2367. Reprinted with permission.
 Workup
Workup
Spinal Imaging
Workup of these patients involves a careful neurological examination and appropriate imaging. While a thorough discussion of imaging requirements is outside the scope of this chapter, many trauma centers have adopted the use of computed tomography (CT) and magnetic resonance imaging (MRI) for all cervical spine injuries. When a fracture is identified, radiographs and possibly MRI of the entire spine should be obtained to rule out noncontiguous injuries. With more sensitive imaging, noncontiguous injuries have been found in up to 28% of patients.6
Treatment
Treatment is based on the neurological status as well as the amount of instability that results from the injury. The SLIC scale assigns points for each of the three components to give an overall stability assessment. In compression injuries, one point is given for a simple compression injury and two points for a burst component. In contrast to distraction and translational injuries, many compression fractures do not include injury to the DLC. In injuries without disruption of the DLC, no neurological injury is present, and according the SLIC scale, there is no significant instability present. These patients may be treated with a rigid orthosis or, infrequently, halo immobilization. Injuries with focal collapse and kyphosis due to disruption of facet capsules and the interspinous ligament result in higher SLIC scores. Although halo immobilization is an option for these patients, the alignment must be neutral or lordotic to avoid subsequent deformity.7 Higher-energy burst fractures, which under the Allen and Ferguson classification involve distraction of the posterior elements, include interspinous widening and segmental kyphosis (> 11 degrees); higher instability is reflected in a higher SLIC score due to DLC disruption (Fig. 6.3).
Neurological status is also used in stratifying instability, with the highest score going to incomplete spinal cord injury. The sum total of the three components of the SLIC scale is used to direct treatment, with surgery recommended for scores with total points > 5. This method resulted in agreement for surgery in 92% of cases.3 Confounding variables, such as ankylosing spondylitis, are also considered.
When angulation exceeds 11 degrees, or a neurological deficit is present, the SLIC score will be higher, and surgical treatment is generally recommended. Surgery may include an anterior corpectomy and instrumented fusion, or a combined anterior/posterior procedure.8 A technique for reduction of the fracture using a posterior-alone method has also been described.9 There is no widespread agreement on when supplemental posterior instrumentation and fusion are necessary, but we recommend this approach in cases where endplate integrity is compromised and/or posterior structures are completely disrupted.5,10
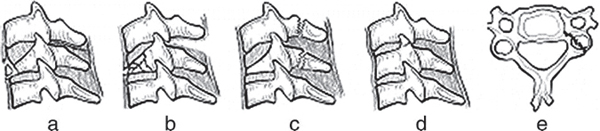
Fig. 6.3 SLIC classification for compression injuries: Simple compression morphology is identified by a visible loss of height in the anterior column (a). Compression may be accompanied by definite DLC disruption (b) or laminar fractures (c). Nondisplaced lateral mass and/or facet fractures are also compression injuries (d). Axial view of lateral mass fracture with vertical fracture line (e). (Reproduced with permission from Vaccaro AR, Hulbert RJ, Patel AA, et al. The Subaxial Cervical Spine Injury Classification System. A novel approach to recognize the importance of morphology, neurology, and integrity of the disko-ligamentous complex. Spine 2007;32:2367.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







