Flexible Valgus Deformity
Kieran T. Mahan
K. Paul Flanigan
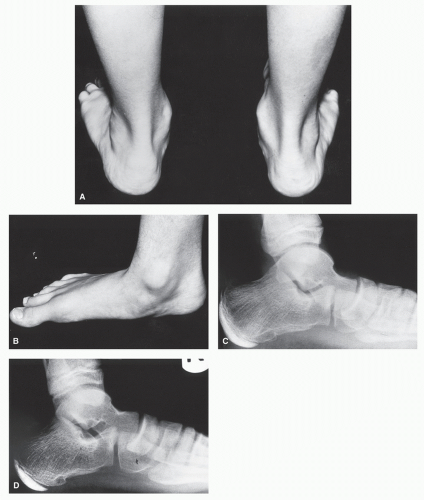
The flatfoot or pes valgus deformity is one of the most common problems challenging the foot and ankle surgeon today. From the pediatric calcaneovalgus to the adolescent tarsal coalition and “adult acquired flatfoot,” its importance and management have been the subject of debate for many years (1). When confronted with the pes valgus deformity, certain questions must be raised. Is a flatfoot or a pes valgus deformity a pathologic condition that affects foot function? If so, how can we determine which patients to treat and how aggressively to treat them? What is the difference between a benign flatfoot and a pathologic pes valgus deformity? In the pediatric population, it is difficult to predict which of the flatfeet will progress to the disabling end-stage pes valgus condition in the adult. Those authors who dismiss pes valgus deformity as trivial, normal, or something that is “outgrown” over time invariably neglect to connect this condition with the many disabling conditions it creates (Fig. 44.1). Is there any other structure in the body in which such a wide deviation from normal joint alignment is accepted as normal variation?
There are numerous causes of the pes valgus deformity (2). These include the following: congenital deformities such as talipes calcaneovalgus and tarsal coalition; structural pathology such as forefoot varus, flexible forefoot valgus, lower extremity torsional abnormalities, and metatarsus adductus; collagen disorders leading to ligamentous laxity; muscle-tendon imbalance resulting from equinus, injury, or degeneration; central and peripheral nerve pathology; and trauma.
Understanding that the pes valgus deformity can result in significant abnormality, the determination between physiologic form, requiring no intervention, and pathologic forms, often requiring treatment, becomes paramount. Subjective complaints are helpful in establishing the diagnosis of a pathologic pes valgus deformity; however, it is the objective presence of instability that is the major factor in securing the diagnosis as pathologic. The low arch foot is not at all synonymous with the unstable hypermobile pes valgus deformity. In their milder forms, some aspects of medial column instability, such as talonavicular or naviculocuneiform sags, an elevated first metatarsal, and increased talar declination, may represent variations of physiologic flatfeet. The presence of medial column instability may be less significant because of the medial column’s primary function as a pronating mobile adapter. Lateral column instability, abduction or dorsiflexion of the cuboid on the calcaneus, may be more indicative of a pathologic condition. Without a secure lateral column, the foot functions with significant instability as significant talonavicular subluxation may often accompany cuboid abduction. Therefore, pain and instability remain the primary indications for the treatment of the pes valgus deformity.
Historically, the mainstay stabilizing treatment for pathologic pes valgus has been the triple arthrodesis (3,4,5,6,7,8 and 9). In addition, numerous soft tissue (2,10,11,12 and 13) and osseous procedures (14,15,16,17,18,19,20 and 21) have been advocated over the years. In the past decade, the use of arthroereisis has gained increased popularity (22,23,24,25 and 26).
When surgery is necessary, the current trend is to reconstruct the valgus foot while preserving the major hindfoot joints whenever possible.
FUNCTIONAL ANATOMY
The pathoanatomy of pes valgus can only be understood if one has a working knowledge of physiologic biomechanics. It is important to appreciate that support and stabilization of the arch is multifactorial and depends on several factors including osseous architecture, intrinsic and extrinsic musculature, fascia, and ligaments of the joints constituting the arch. Both static and dynamic factors play important roles. Basmajian and Stecko (27) demonstrated through electromyographic studies that muscles do not significantly contribute to supporting the arch. In static stance, stability is primarily achieved through the osseous and ligamentous structures.
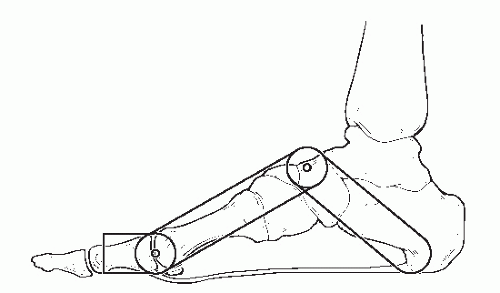
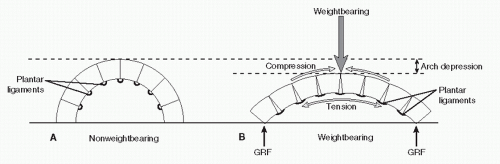
Classically, the arch has been likened to a truss and beam (28). A truss is composed of two struts connected by a tie rod. In the foot, the lesser tarsus and metatarsals compose the anterior strut, and the talus and calcaneus function as the posterior strut. The plantar fascia acts as the tie rod connecting the struts (Fig. 44.2). In stance, the talus or apex of the truss is loaded, and compressive forces are transmitted through the struts as they attempt to separate. The tie rod is placed under tension and resists the separation of the struts and collapse of the truss. An articulated beam can also be likened to the foot. When loaded, compression is generated on the dorsal of convex side and tension on the plantar or concave side. Collapse is resisted by plantar ligaments (Fig. 44.3).
The plantar fascia has long been considered an important structure in stabilizing the longitudinal arch. It is composed of three bands corresponding to the compartments of the foot (29). The medial and lateral bands serve as fascial coverings of the abductor hallucis and abductor digiti minimi muscles, respectively. The thick central band, or plantar aponeurosis, spans the entire length of the foot from the calcaneus to indirect attachments at the metatarsal heads and phalanges (30,31). The plantar aponeurosis is the major contributor to longitudinal arch stability.
The spring ligament has also been considered an important structure in stabilizing the longitudinal arch (32,33 and 34). The broad superomedial calcaneal navicular portion of the spring ligament possesses a triangular articular facet in the deep central portion of the ligament (33). The superomedial calcaneal navicular ligament provides the only medial to lateral articulation on the head of the talus and must contribute to stabilizing the head of the talus because of its articulation.
In gait, maintenance of the arch depends on both static ligamentous support and dynamic function of the plantar fascia, intrinsic muscles, and extrinsic muscles (27). The exact role of
the plantar intrinsic musculature to support the arch during gait remains largely unknown. Most of the plantar intrinsics are oriented parallel to the long axis of the foot and it is conceivable that their contracture can lend support to the arch. Intrinsic contraction acts to plantarflex the first ray, invert the calcaneus, and cause external rotation of the tibia (35). The net effect is supinatory effect on the foot and an increase in the height of the arch. In static stance, the intrinsics are inactive in normal persons and active in flat-footed persons (27,36,37). They are active earlier and longer in flat-footed patients when compared with physiologically normal patients (36). In particular, the abductor hallucis has been shown to provide consistent
support and elevation of the arch (35,38,39). Chronic arch pain and fatigue can largely be attributed to the increased activity of the abductor hallucis and intrinsic musculature in patients with pes valgus.
the plantar intrinsic musculature to support the arch during gait remains largely unknown. Most of the plantar intrinsics are oriented parallel to the long axis of the foot and it is conceivable that their contracture can lend support to the arch. Intrinsic contraction acts to plantarflex the first ray, invert the calcaneus, and cause external rotation of the tibia (35). The net effect is supinatory effect on the foot and an increase in the height of the arch. In static stance, the intrinsics are inactive in normal persons and active in flat-footed persons (27,36,37). They are active earlier and longer in flat-footed patients when compared with physiologically normal patients (36). In particular, the abductor hallucis has been shown to provide consistent
support and elevation of the arch (35,38,39). Chronic arch pain and fatigue can largely be attributed to the increased activity of the abductor hallucis and intrinsic musculature in patients with pes valgus.
The arch-supporting effect of extrinsic muscles can in part be explained by the moment arms of the tendons passing on the supinatory side of the subtalar joint axis (Fig. 44.4). The tibialis posterior has the longest lever arm and is the most efficient supinator (40). Its pivotal role in dynamic arch maintenance is well established. Contracture of the tibialis posterior does not just supinate the foot and elevate the arch but decelerates internal rotation of the lower leg. The excessive internal rotation of the leg forces the talus into adduction and because the ankle joint allows for little transverse plane motion, the result in stance is a pronated subtalar and midtarsal joint (41,42 and 43). The arch-stabilizing effect of the tibialis posterior can also be attributed to its extensive ligamentous support provided by its many deep insertions and its direct plantarmedial location to the spring ligament and talar head. The flexor digitorum longus has a longer moment arm than the flexor hallucis longus and likewise is more efficient in supporting the arch (40,44). In patients with pes valgus, the extrinsic activity of the soleus, tibialis posterior, tibialis anterior, and peroneus longus are increased during stance when compared to the normal foot (45).
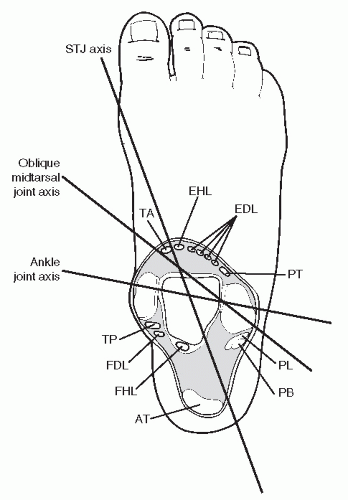 Figure 44.4 Cross-sectional diagram through the rearfoot illustrating the relationship of each tendon with the major rearfoot joint axis. AT, Achilles tendon; EHL, extensor hallucis longus; EDL, extensor digitorum longus; FHL, flexor hallucis longus; FDL, flexor digitorum longus; PT, peroneus tertius; PL, peroneus longus; PB, peroneus brevis; STJ, subtalar joint; TA, tibialis anterior; TP, tibialis posterior.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|