Fixation Through a Dorsal Approach for Small Proximal Pole Fragments
H. Kirk Watson
E. Aron L. Haass
Indications
The scaphoid, the most commonly fractured carpal bone, accounts for 60% of all carpal fractures (1). Approximately 95% of stable, undisplaced scaphoid fractures when treated with immobilization will go on to union. Delayed diagnosis, inadequate treatment, and complicated fracture patterns with displacement all contribute, however, to an increase prevalence of scaphoid nonunion (2,3,4). Of all acute scaphoid fractures nearly 25% involve the proximal scaphoid (Fig. 14-1) (5). The average time to union of an acutely fractured nonsymptomatic proximal scaphoid is 3 to 6 months with conservative immobilization. Chronic symptomatic nonunion of the scaphoid lasting longer than 3 to 6 months requires surgical intervention to achieve bony healing (6,7,8,9,10,11,12). Optimal management of scaphoid nonunion should include bone grafting.
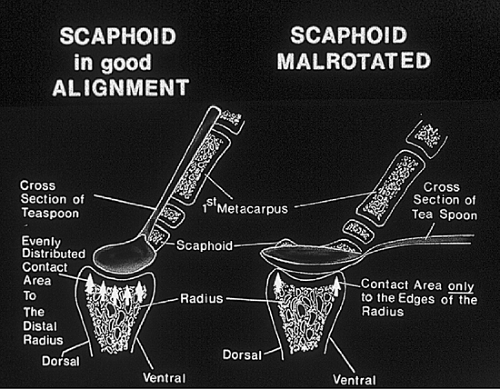
Scaphoid nonunion will lead to scapholunate advanced collapse (SLAC) wrist. The speed with which degenerative changes occur is based on the degree of rotation of the distal pole. The pattern of SLAC degeneration following rotary subluxation of the scaphoid (RSS) is well documented (13,14). If the scaphoid rotates abnormally with the proximal pole displacing from beneath the capitate, the situation is not unlike two spoons. So long as the handles remain together, any movement maintains congruous surface contact. If the handles are allowed to rotate 90 degrees to one another, the upper spoon will rise from the lower spoon and the edges of the lower spoon (radius) will wear on the central convex portion of the upper spoon (scaphoid) (Fig. 14-2). The lunate articulation with the radius is spherical, the oblong joint phenomenon above cannot occur and the joint is always preserved.
If we cut the scaphoid into two parts (scaphoid nonunion), the distal pole will rotate (now free of the lunate constraints) and destroy itself against the radius. The proximal pole will be treated as if it were a lunate. The proximal articular surface is spherical and will not be destroyed. The capitate will shear load the distal surface of the proximal pole and arthritis will develop here just as it does the distal lunate articulation in stage II SLAC. An issue, therefore, in scaphoid nonunion independent of symptoms is that all cases of scaphoid nonunion will develop SLAC wrist. This becomes of paramount interest when determining whether to bone graft a young asymptomatic man. This is one of the situations when hand surgery is indicated in an asymptomatic wrist.
Typically, however, scaphoid nonunions are symptomatic. There will be activity pain and postactivity ache. Postactivity ache is an indicator of the degree of synovitis produced by an activity (14). Postactivity ache of more than 6 hours means major synovial insult. On examination, the finger extension test (FET) is positive when load cannot be transmitted through carpals to radius. A negative FET means no radial wrist disease (15). This includes carpal fracture, carpal bosse, rotary subluxation of the scaphoid, scaphoid nonunion, Presiser or Kienböck, dorsal wrist syndrome, with or
without ganglion, Colles’ malunion, or gymnast wrist. The real value of the FET to the hand surgeon lies in its reliability when negative. The scaphoid shift may or may not be positive. Usually tenderness is found at the articular nonarticular junction (ANA) and periscaphoid synovitis.
without ganglion, Colles’ malunion, or gymnast wrist. The real value of the FET to the hand surgeon lies in its reliability when negative. The scaphoid shift may or may not be positive. Usually tenderness is found at the articular nonarticular junction (ANA) and periscaphoid synovitis.
Proximal pole nonunions are often more symptomatic than distal pole fractures because more of the scaphoid rotates. Because degenerative joint disease (DJD) always forms between the radius and the distal pole and never the proximal pole, removal of the proximal pole is not a solution. Any long-term effective treatment must address the distal pole rotation.
Treatment option no. 1 is fusion of the nonunion. The ligaments are intact between lunate and proximal pole and fusion reestablishes scaphoid stability and the best wrist.
Treatment option no. 2 is to fuse the scaphoidtrapeziumtrapezoid (STT) joint to control rotation of the distal scaphoid pole. This is most effective when there is a very small fragment of proximal pole, essentially a rotary subluxation of the scaphoid where the interosseous ligaments have ruptured taking a small piece of the proximal scaphoid with them. When the proximal pole is larger, then STT fusion with additional bone grafting of the nonunion is indicated.
Treatment option no. 3 (the first two options apply when there is no DJD): If degenerative changes have begun, the symptomatic relief can be achieved by excising the distal scaphoid. The wrist will not usually tolerate load because of the severe midcarpal collapse that occurs either into dorsal intercalated segment instability (DISI) or volar intercalated segment instability (VISI) depending on type of lunate (V or D type) present. This approach is reserved for less demanding wrists. Either way, the capitate displaces radially and sheer loading destroys the joint between the capitate and proximal pole just as it does the capitate-lunate joint.
A similar approach under this treatment option is to remove the radial styloid. This is effective if the fracture site is distal and only a small portion of the radial fossa is involved with the distal fragment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree