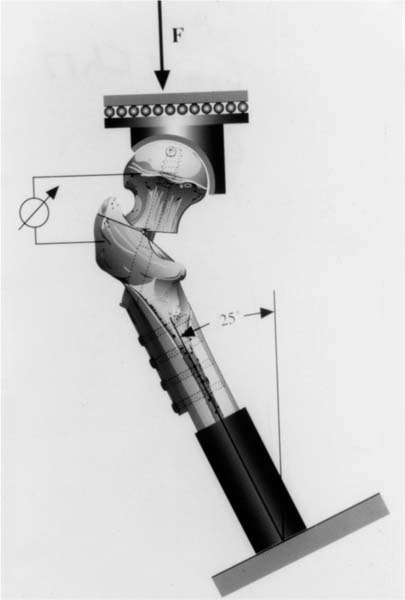
Chapter 17 In the last 20 years, the number of femur fractures close to the hip has risen substantially, which is mainly due to the change in the age pyramid and the resulting increase in osteoporosis.1 Unstable intertrochanteric fractures in particular are very common in elderly people and pose a special problem because of the presence of advanced osteoporosis with a reduced mechanical bone quality, which makes it more difficult for implants to bond to bone in a sufficiently stable manner.1–3 The most frequently applied osteosynthesis technique for intertrochanteric fractures involves the dynamic hip screw (DHS, Synthes). Complication rates of up to 20% are reported for unstable femur fractures.4–6 A common complication with mechanically weak osteoporotic bones is the migration of the screw through the femoral head, perforating the joint and causing the femoral head to tilt into a varus position.4,7 A reinforcement of the mechanically weak bone is desirable to avoid such implant migrations in the osteoporotic bone. Adjunctive osteosyntheses such as those performed since the 1970s with the aid of polymethylmethacrylate (PMMA) bone cement can increase the primary stability.8–12 There have been endeavors for some years to replace the PMMA bone cement with new cements as the PMMA cement releases monomers, undergoes fibrous sheathing, and does not form a permanent bond with the adjacent bone in vivo. More favorable possibilities present themselves with a new cement on a glass-ionomer basis,13 which promises a chemical bond with the bone and thus a better and long-lasting adhesion to bone. However, before conducting in vivo trials, we had to establish whether an increased primary stability of the implant’s bond with the osteoporotic bone could be achieved with the aid of the new cement. The experimental investigations were performed on eight pairs of female cadaver femurs, with an average age of 76.9 (range 62 to 87) years. The mean degree of osteoporosis according to Singh was 2.9 (range 2 to 3). The average CCD angle was 120 ± 4.8 degrees. The femurs had been stored frozen at –30°C and were thawed at 37°C for 12 hours before the start of the experiment and were kept wet with Ringer’s solution. Glass-ionomer cements have been used for dental fillings for some 20 years; however, the experience so far with regard to applications in trauma surgery and orthopaedics is still inadequate. The cement consists of two components that have to be mixed in a fixed proportion before use. The powder consists of a calcium-aluminum-fluorosilicate glass with a particle size of 0.1 mm. The liquid component consists of an aqueous solution of a polycarbonic acid (acrylic acid-maleic acid copolymer) and tartaric acid. The setting reaction is an exclusively ionic reaction and is based on a neutralizing reaction between the polycarbonic acid and the alkaline glass powder. The cured glass-ionomer cement (Ionos, Munich) consists of a solid insoluble aluminum-calcium-polycarboxylate matrix in which the glass particles and water molecules are embedded. Compared to the conventional PMMA bone cement, the glass-ionomer cement has the following advantages: • Ionic setting takes place, without any appreciable rise in temperature, in the physiological temperature range. • Practically no loss of volume occurs during setting. • It constitutes a hydrophilic system that can produce ionomeric bonds with the calcium in the bone. Due to the glass portion, the cement’s resistance to pressure (110 MPa) is markedly higher than its flexural strength (19.8 MPa). As mixing must be performed in a precisely dosed proportion, the two components are supplied by the manufacturer in premeasured single-use packaging. After blending in a special mixer (Rolomix, Ionos, Munich), a manipulation time of some 4 minutes remains until curing. For the stabilization of the intertrochanteric model fractures, we used DHS (Synthes) with an angle of 135 degrees and lengths of 95 to 105 mm. To guarantee a good distribution of the glass-ionomer cement when screwing the DHS into the femoral head, a groove of 2 mm width and 3 mm depth was cut into the thread part, parallel to the screw’s axis, across the entire length of the thread. To obtain experimental conditions as standardized as possible, the DHS implants were first implanted on the intact bone without cement, according to the recommendations of the AO, using the original set of instruments. Subsequent radiological checks performed in two planes showed that all the screws had been put in place close to the calcar in such a way that their tips were located in a central position in the femoral head, directed against the dorsal-caudal quadrant, and within 5 to 10 mm of the cortex layer. The implants were then removed again and standardized fracture conditions produced by osteotomies. The first osteotomy was performed at an angle of 45 degrees to the longitudinal axis of the femoral shaft from medial above the lesser trochanter to lateral toward the greater trochanter (Fig. 17–1). A deficient medial support was simulated with a second osteotomy running from the center of the osteotomy area to a point below the lesser trochanter (Fig. 17–1). This produced an instability of the kind developed under clinical conditions when a medial fragment is blown out. The two fragments of the femur were then stabilized with the DHS. FIGURE 17–1 Diagram of test setup for the dynamic load test of the proximal femur with an unstable intertrochanteric fracture with deficient medial support and osteosynthesis with DHS. (Reprinted from Claes et al. Unfallchirurg 1995;98:118–123, with permission from © Springer-Verlag.) We randomly selected one bone of each pair for additional cement fixation. With these bones, 6 g of glass-ionomer cement was injected into the screw hole of the femoral head with an injection gun before the DHS was put into place. The fragment was repositioned, then the screw was screwed in and the osteosynthesis completed. For clamping into a materials testing machine, the distal end of the femurs were embedded in steel cylinders with plastic (Technovit 3040, Heraeus Kulzer, Wehrheim, Germany) up to 2 cm below the end of the DHS plate. With the aid of these cylinders, the femurs were fixed in the clamping device of the materials testing machine (Zwick 1454, Einsingen, Germany) at an angle of 25 degrees to vertical in the frontal plane (Fig. 17–2
FIXATION OF UNSTABLE
OSTEOPOROTIC INTERTROCHANTERIC
FRACTURES USING THE DHS AND
A GLASS-IONOMER CEMENT
TESTING OF THE SYSTEM
ANATOMICAL SPECIMENS
GLASS-IONOMER CEMENT
IMPLANTS
FRACTURE MODEL
DYNAMIC LOAD TEST
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree