Femoral Revision
Allograft Prosthetic Composites and Proximal Femoral Replacement
Paul Tee Hui Lee, Oleg A. Safir, Catherine F. Kellett, David J. Backstein and Allan E. Gross
Key Points
Introduction
Revision total hip replacement (THR) in patients with severe proximal femoral bone loss is difficult. Bone loss extending more than 5 cm distal to the lesser trochanter precludes the use of most conventional THR techniques. Salvage procedures such as excision arthroplasty have shown poor results.1,2 Arthrodesis is difficult to achieve.3 Viable options include the use of allograft prosthetic composites, proximal femoral replacements, and impaction bone grafting techniques. The use of allograft prosthetic composites and proximal femoral replacements will be discussed in this chapter.
Proximal femoral replacement (PFR) is defined as a metal femoral implant, proximally connected to a femoral head to articulate with the acetabulum and distally fixed to the host femur. It may be cemented or uncemented, modular or nonmodular. Historically, proximal femoral replacement was used after tumor resection.4 The initial designs were cobalt-chrome monoblock with segmental length increments cemented into the distal femur. Later developments included modularity to better accommodate leg length and porous coating to promote bony ingrowth at the junction with extracortical bone bridging, although this concept has not been shown to occur with predictability even with bone grafting. Indications recently have been expanded to include non-neoplastic conditions such as failed THR with massive proximal femoral bone loss and periprosthetic fractures.
Allograft prosthetic composite (APC) in revision THR is defined as a long femoral stem prosthesis that is proximally incorporated into a proximal femoral bone allograft. This technique has gained popularity over the past decade with several encouraging longer-term reports.5–10
When comparing APC with PFR, the advantages for using PFR include easier availability without the need for access to banked bone, easier implantation without the need for expertise in the use of massive bone allografts, and shorter operative duration with potentially lower blood loss and infection rates. Patients with PFR are generally allowed to bear weight earlier in the postoperative period and have less demanding postoperative rehabilitation programs.
Revision THR with PFR, however, is associated with higher dislocation rates.11,12 PFR provides poor attachment of host bone and soft tissue, leading to weaker abductors and a higher rate of Trendelenburg limp.13 There is also the disadvantage of violating the host distal femoral canal with reaming for stem cementation or press-fitting, which is undesirable with regard to bone preservation, especially in younger higher-demand patients. In terms of survivorship, reports have suggested higher rates of loosening and failure with PFR.13,14
The use of APC has the potential to restore proximal femoral bone stock and minimize host distal canal violation to preserve bone stock to aid future reconstructions. By avoiding cementing or significant reaming for press-fitting the implant distally, the distal host canal is relatively preserved. The use of proximal allograft aids host bony and soft tissue attachment, in particular the host greater trochanter. When the host greater trochanter is destroyed, the use of proximal femur-abductor tendon allograft facilitates host abductor tendon repair. APCs with trochanteric and abductor repairs have lower rates of abductor impairment, limping, instability, and dislocation compared with PFR.11–13
Indications and Contraindications
Indications
The general indication for the use of APC or PFR is significant proximal femoral bone loss of greater than 5 cm distal to the lesser trochanter. Bone loss may be caused by tumor resection, previous THR infection, periprosthetic fracture (e.g., Vancouver B3), or osteolysis.
In general, APC is used in younger, higher-demand patients, who will potentially require multiple revisions.
Contraindications
Patients with absolute general contraindications to APC and PFR include those who are medically unfit for major surgery, those with unresolved superficial or deep hip infection, and patients who will not be cooperative with the postoperative rehabilitation program. Another contraindication is the ability to reconstruct the femur using alternate techniques, such as modular tapered fluted stems. Relative general contraindications include morbid obesity and poor central or peripheral perfusion. After radiation therapy, APC should not be used because of poor potential for healing at the host-allograft junction. In this setting, PFR is preferred. Finally, lack of familiarity with the technique and limited experience in revision total hip arthroplasty on the part of the surgeon or the surgical team are contraindications to these complex techniques; such cases should be referred to centers with more experience with these techniques.
Of note, prerequisites for the use of APC include access to the bone bank, expertise in the use of massive structural allografts, and patient commitment to the postoperative rehabilitation program. Failing that, the alternative—use of PFR—is advised.
Preoperative Planning
Because the use of PFR is technically similar to that of most distal fixation stems, with the exception of the need for fixation of the hip abductors to the stem, we will focus on the technical details associated with APC.
Allograft Prosthetic Composites
Allograft Availability
We recommend acquiring fresh-frozen allograft from a tissue bank that is accredited by the American Association of Tissue Banks.15 In general, these allografts are irradiated for sterility and are stored at −70° C.
Preoperative planning is required so the correct sizes of allograft and implant can be ordered. Anteroposterior (AP) pelvis and full femur radiographic views with a calibrated radiographic marker are obtained to estimate the length and diameter of the graft and implant required. The allograft length is estimated from the length of the proximal femoral deficiency. This usually correlates with the distance from the center of rotation of the hip joint to the level in the distal femur where adequate bone stock is present to support the allograft. This estimation should take into account apparent leg length discrepancy due to stem subsidence or periprosthetic fracture. A graft that is substantially longer than estimated is ordered to allow for intraoperative adjustments, and should account for at least a 3- to 5-cm step cut at the allograft host-bone junction. The estimated stem length should be generously longer than the estimated graft length, and the anticipated stem tip is more than 4 to 6 cm away from the knee joint.
The graft canal diameter is usually narrower than the host canal, which is often widened by cortical thinning from osteolysis and cavitation around previous loose femoral components. Avoid choosing a graft with an outer diameter that is substantially narrower than the host to reduce the risk of unstable intussusceptions and uncontrolled subsidence postoperatively. Ideally, the outer diameters of the graft and host should be matched at the distal graft-host junction for optimal junctional stability. However, using a slightly narrower graft to telescope into the host distal femoral canal by 1 to 2 cm and ensuring initial junctional fixation stability may enhance union and long-term stability (Fig. 99-1).

Figure 99-1 Preoperative (A) anteroposterior (AP) and (B) lateral distal femoral radiographs showing uncontained severe proximal femur bone loss.
Ruling Out Infection
Preoperative workup should exclude infection using serologic inflammatory markers (C-reactive protein [CRP], erythrocyte sedimentation rate [ESR]). If necessary, other workup as discussed elsewhere in this book may be necessary. The operation should not be booked until the surgeon is reasonably certain that infection is not a cause of failure.
Equipment and Implants
Patients with severe proximal bone loss who requires revision THR usually have multiple previous hip surgeries with poor soft tissue function and increased risks of instability and dislocation. We often consider the potential need for using large bearings or constrained liners. In patients with poor abductor function and destroyed greater trochanter, we would also consider the use of proximal femur-abductor tendon allograft for attaching host abductor tendons.
Leg Length Discrepancy
Preoperative assessment for leg length discrepancy will guide the amount of leg lengthening during surgery. Apparent leg length difference measured clinically is correlated with radiographic assessment. Significant fixed flexion or adduction contracture may require release intraoperatively. Our guidelines for safe limb lengthening with regard to risk for sciatic stretch are 4 to 5 cm in previously equal limbs (e.g., before periprosthetic fracture) and 2 to 3 cm in previously unequal limbs (e.g., persistent shortening after THR for severe congenital hip dislocation).
Description of Technique
General Setup
Prophylactic intravenous antibiotics are administered before urinary catheterization is performed. The patient is secured in the lateral decubitus position with protection to pressure areas.
To reduce operative time, the graft is prepared by part of the team on a separate surgical table while the revision surgery is being performed.
Initial Graft Preparation
Microbiological culture specimens are taken before the allograft is thawed in 5% povidone-iodine solution and stripped of soft tissues.
The femur neck is cut just proximal to or even at the base of the lesser trochanter to facilitate implant insertion and version adjustment.
Leg lengthening is affected not by the level at which the neck is cut but by the length of the allograft prosthetic composite, which is determined by the level at which the distal allograft is cut. The allograft should initially be cut long to allow for adjustments.
Because the success of the procedure depends on union at the distal graft-host junction, a stable graft-host junction is crucial. Stability is achieved largely by a stepped or oblique graft-host reciprocating osteotomy. An oblique osteotomy is technically easier to achieve and allows adjustments in rotational alignment without major changes to the osteotomy.
The greater trochanter is excised to allow reattachment of the host greater trochanter. In the absence of host greater trochanter, the allograft greater trochanter is preserved along with a cuff of abductor tendons to which the host abductors can be attached.
The canal is then reamed. We use straight, rigid reamers because we prefer straight stems. Flexible reamers can be used for bowed stems. The canal is reamed just wide enough to accommodate the stem and a 2-mm cement mantle. Care is taken to avoid over-reaming, which leads to disproportionate graft resorption. A thin rim of cancellous bone is preferably preserved for cement-bone interdigitation. We use a long stem, usually 13 to 14 mm in diameter (CRC, Zimmer, Warsaw, Ind), or a modular ZMR (Zimmer) with distal nongrit blasted flutes, which is also proximally narrow. A large-diameter stem for distal press-fit requires excessive graft reaming because the canal is usually narrower than host distal femur. We believe that distal stem press-fit is not essential for construct stability. We achieve stability by cementing the stem to the graft but not the distal host femur, allowing compression and micromotion at the host-graft junction to promote union. The allograft is then returned to the povidone-iodine bath until the main surgical team has finished preparation of the host-femoral junction, at which time a reciprocal and matching cut is made in the allograft at the appropriate location, and the allograft prosthetic construct is trialed, before the definitive stem is cemented into the allograft.
Surgical Approach
We use a lateral longitudinal skin incision and try to incorporate previous scars. For a loosened stem, a trochanteric slide approach in conjunction with a lateral longitudinal femoral split is usually sufficient for good exposure to the acetabulum and femur. The greater trochanteric-abductor unit can be reattached later to the proximal femoral allograft.
We have modified the trochanteric slide by leaving the posterior 1 cm of the greater trochanter, posterior capsule, and external rotators intact with the shaft to decrease the risk of posterior dislocation.16
Because the greater trochanter is usually very thin in the setting of proximal femoral deficiency, care is taken to maintain continuity with the abductors and vastus lateralis to decrease the risk of subsequent trochanteric escape.
The vastus lateralis is then partially detached laterally from the lateral intermuscular septum by blunt dissection to the intended level of distal femoral osteotomy. This level is determined during preoperative planning and intraoperatively by identifying the extent of femoral deficiency where healthy distal femur starts. Care is given to cauterize the perforating vessels away from the septum to avoid vessel retraction, difficult hemostatic control, heavy blood loss, and postoperative hematoma formation.
The trochanteric fragment is then reflected anteriorly and the lateral proximal femur is split longitudinally in the coronal plane to the intended level of the distal femoral osteotomy. At this level, a transverse saw cut is made halfway through the diameter of the femur from lateral to medial, taking care to keep the medial half of the femur intact.
With multiple osteotomes fitted through the lateral longitudinal split and engaging the undersurface of the anterior femoral cortex, the anterolateral proximal femur is pried forward; similarly, the posterolateral proximal femur is pried backward—akin to an open book—from the lateral aspect of the femur. At the level of the transverse cut, care is taken to leave the medial aspect of the femur intact to fashion a step-cut or oblique-cut osteotomy with optimal host bone preservation. The length of the step- or oblique-cut should be at least 2 cm (Figs. 99-2 and 99-3).
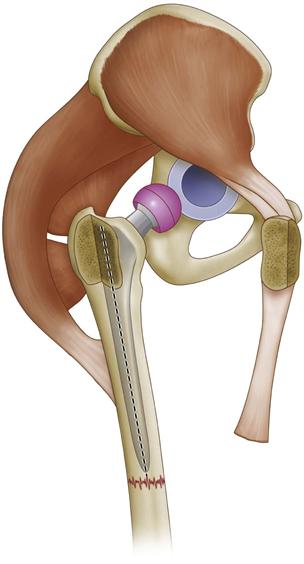
Figure 99-2 The external rotators remain attached to the femur when the posterior 1 cm of the greater trochanter is left attached to the femur. (Redrawn from Kellett CF, Boscainos PJ, Maury A, et al: Proximal femoral allograft treatment of Vancouver type-B3 periprosthetic femoral fractures after total hip arthroplasty: surgical technique. J Bone Joint Surg Am 89[Suppl 2, Pt 1]:68–79, 2007.)
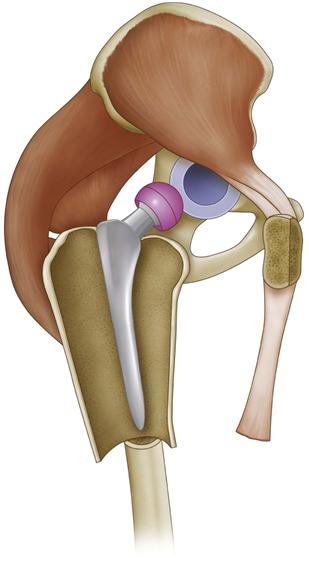
Figure 99-3 Lateral cortex osteotomy of the proximal part of the femur. (Redrawn from Kellett CF, Boscainos PJ, Maury A, et al: Proximal femoral allograft treatment of Vancouver type-B3 periprosthetic femoral fractures after total hip arthroplasty: surgical technique. J Bone Joint Surg Am 89[Suppl 2, Pt 1]:68–79, 2007.)
Any residual host proximal femur is preserved with soft tissue attached to serve as vascularized autograft for wrapping around the distal allograft-host junction to promote union. Any residual host proximal femur is also wrapped around the proximal allograft. The proximal host femur does not replace the proximal allograft, but union at this interface may reinforce the allograft. The success of the allograft prosthetic composite is determined by the critical union at the distal graft-host junction and not at the host-graft interface proximal to the junction because usually very little proximal host bone is available to wrap around the proximal allograft.
Leg Length Reference and Monitoring
A Steinman pin is inserted over the iliac crest and is referenced to a fixed point in the host distal femur for leg length monitoring during the operation. The distal reference point should be in healthy host bone distal to the allograft and marked by a drill hole. The distance from the Steinman pin to the distal reference point is measured. Preoperative leg length differences can be used to guide leg length adjustments during surgery.
At this point, the hip is dislocated and the old loosened femoral component usually is easily removed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








