7 Femoral Neck Fractures
Arthroplasty
The use of arthroplasty for the management of displaced fractures of the femoral neck is generating increasing interest.1 Because of the uncertainty of outcome following reduction and fixation of displaced femoral neck fractures, surgeons are increasingly turning to arthroplasty as a more certain procedure in terms of patient satisfaction and lower revision rate.2 Arthroplasty for femoral neck fractures is generally a more complicated surgical procedure than reduction and fixation, however, and meticulous attention to detail is necessary to ensure the success of the procedure.3
Indications
Arthroplasty is indicated for displaced intracapsular fractures of the femoral neck. In elderly patients with significant osteoporosis, arthroplasty is the operation of choice.4 The decision between unipolar or bipolar arthroplasty and total hip replacement should be made on the basis of the patient’s preoperative activity level or the presence of antecedent symptomatic hip arthritis. As a general rule, younger, more active patients have better outcomes with total hip replacement, thus making the slightly increased risk of complications with that procedure acceptable.5
Elsewhere in this text, the technique of internal fixation and its indications and complications are explored. Arthroplasty is a viable alternative to internal fixation for patients with completely displaced fractures, particularly in the presence of significant comminution or significant osteoporosis. The role of monopolar, bipolar, and total hip arthroplasty should be made on the basis of the surgeon’s experience, the availability of the implant, and the patient’s activity level rather than on patient age alone.6,7 Implant costs may also play a role in selection of treatment.
Bipolar and unipolar arthroplasty procedures have a significant advantage of increased stability as compared with total hip replacement.8 However, the introduction of highly cross-linked polyethylene has allowed for the use of thinner polyethylene inserts and therefore larger-diameter femoral heads in total hip arthroplasty. These improvements have increased the stability of that operation and decreased the risk of dislocation. The choice between cemented and cementless components largely depends on the surgeon’s preference, although in patients with extreme osteopenia with a large medullary canal, a cemented stem offers more secure fixation and the possibility of immediate weight bearing without concerns about prosthetic subsidence.9 However, cemented stems are recognized to pose a slight but definite increase in the risk of systemic fat embolization; they also prolong the operative procedure by approximately 10 minutes as compared with cementless stems.
Surgical approach is again dependent on the surgeon’s preference.10 The technique illustrated in this chapter is the posterior approach, but the direct lateral approach is also frequently used. The advantage of the direct lateral approach is the decreased rate of dislocation, particularly in patients who have preoperative or postoperative confusion or delirium. The disadvantage is the increased weakness of the abductors as a consequence of the approach that may increase or prolong a postoperative limp.
Imaging
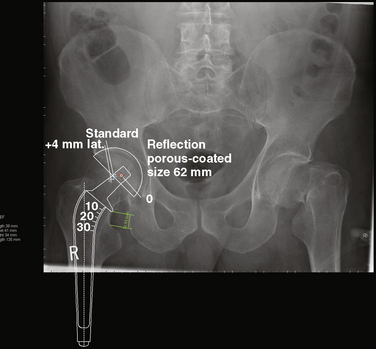
Plain radiographic films are adequate for decision making for this fracture. A true anteroposterior x-ray film of the hip, an anteroposterior radiograph of the pelvis, and a lateral radiograph of the hip are recommended. These studies demonstrate both the fracture pattern and the degree of displacement and provide important information about bone quality and the possibility of preexisting hip arthritis. Because leg length discrepancy following prosthetic replacement for femoral neck fractures is a potential problem, a radiograph of the opposite hip included in the anteroposterior pelvis study is helpful in templating to determine where the femoral neck cut should be made to minimize the possibility of leg length discrepancy (Fig. 7-1).
Surgical Technique
Anesthesia and Positioning
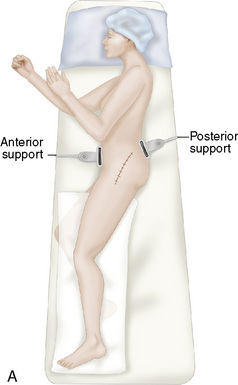
A pillow is placed between the patient’s legs with the contralateral hip and knee flexed slightly, and the upper body is secured with a safety strap and, if necessary, an axillary roll. The supporting pegs or rests should be sufficiently proximal to allow full hip flexion of the affected leg (Fig. 7-2).
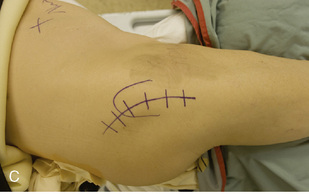
Exposure of the Femoral Neck and Removal of the Femoral Head
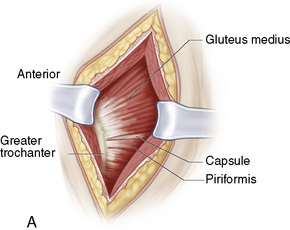
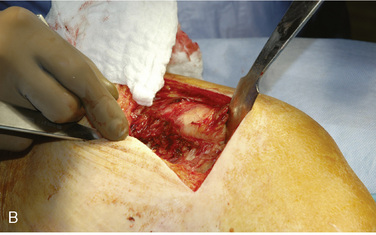
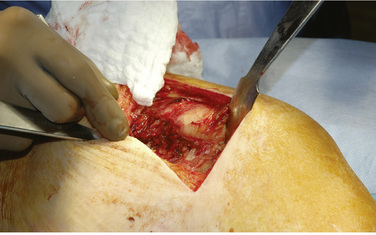
A lateral longitudinal incision is centered over the greater trochanter, with the proximal portion curved or angled slightly posteriorly. The overall length of the incision should be approximately 15 cm. The fascia lata is split distally in line with the femur, and the tensor and gluteus maximus muscles are split proximally in line with the muscle fibers. Care should be taken to separate the muscle fibers rather than cut them, to minimize bleeding (Fig. 7-3). The posterior edge of the gluteus medius is identified, a retractor is placed deep to this muscle, and the muscle is retracted anteriorly and superiorly.
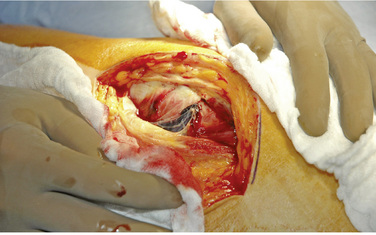
The trochanteric bursa should then be incised or excised to expose the posterior structures of the hip joint. The external rotators are usually covered with a thin layer of fat, which can be easily removed (Fig. 7-4). The leg should then be adducted and internally rotated to place the external rotators under tension (Fig. 7-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree