Fig. 19.1
(a, b) Suspected femoral neck fracture X ray (a), CT (b)
19.5.3 Magnetic Resonance Imaging (MRI, MRT)
MRI is rarely indicated, generally only if a fracture cannot be detected using CT scan (1–2 %). Undoubtedly, the MRI is not a first-line diagnostic tool. If it is performed earlier than 5–6 h after the accident, it can be falsely interpreted as negative.
Other diagnostic methods such as conventional X-ray tomography, scintigraphy, and ultrasound examination are obsolete. They do not play a role in routine diagnostics and are not used. About 1 % of all femoral neck fractures are not detectable at all; they manifest after days or weeks with the classical clinical image.
19.6 Classifications [6, 7]
19.6.1 Garden Classification (Fig. 19.2)
This classification is based on the degree of the displacement of the fracture fragments in a.p. and axial X-rays [6, 7].
Garden I: “incomplete,” valgus impacted fracture, the femoral head is attached in valgus like a mushroom cap on the femoral neck. A fracture is considered as compressed if the a.p. X-ray shows a valgus displacement of the femoral head without any axis deviation in the axial plane. If the axial X-ray reveals an antecurvatum (more often) or a retrocurvatum (less often) and if the fracture gapes, it is still reasonable to categorize it as an incomplete fracture. An exact interpretation of the x-rays is crucial for the adequate choice of treatment. Conservative therapy can only be applied for fractures with compression on both planes.
Garden II: “complete” fracture of the femoral neck. It is detectable on the X-rays in two planes, without any axis deviation in the two planes.
Garden III: partially displaced fracture. The femoral head and neck are misaligned, the axis proportions have changed, but both fragments are still in contact. Therefore, a reduction using simple procedures seems to be possible.
Garden IV: completely displaced fracture. Fracture surfaces of the femoral head and neck are completely dislocated. Reduction is hardly possible or can only be achieved with great difficulty.
The Garden classification reflects the probability of vascular damage resulting from the fracture type. It could be an indicator of avascular necrosis of the femoral head, a long-term consequence of the femoral neck fracture because the degree of the displacement correlates with the degree of blood supply dysfunction of the femoral head. As a consequence, the probability of the development of an avascular necrosis is low in a Garden I fracture and high in a Garden IV fracture.
Because there is no linear relationship between displacement and blood supply dysfunction, the Garden alignment index was introduced. For its calculation, the angles between the trajectory course in the femoral head and those axis that are generally used to describe the hip joint (CCD) have to be measured. The likelihood of the development of a femoral head necrosis is directly proportional to the magnitude of the angle in a.p. view and to the deviation of the angle from the straight line in the axial view. If this deviation exceeds 20–30°, the incidence of a femoral head necrosis has to be assumed.
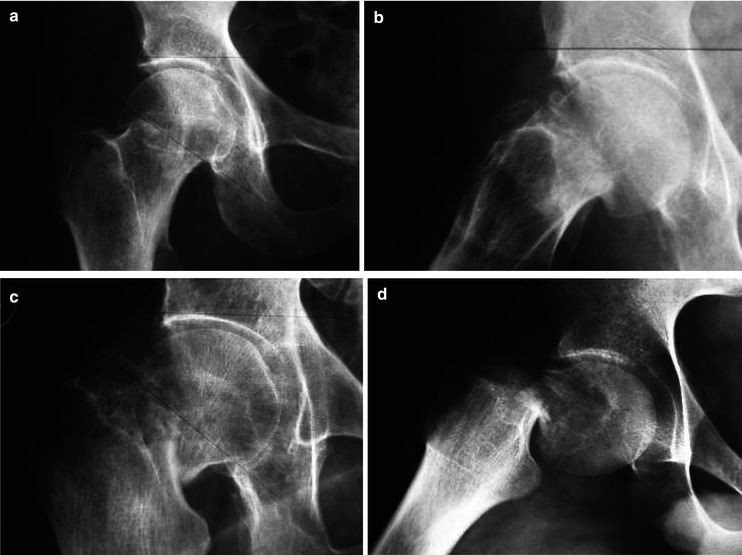
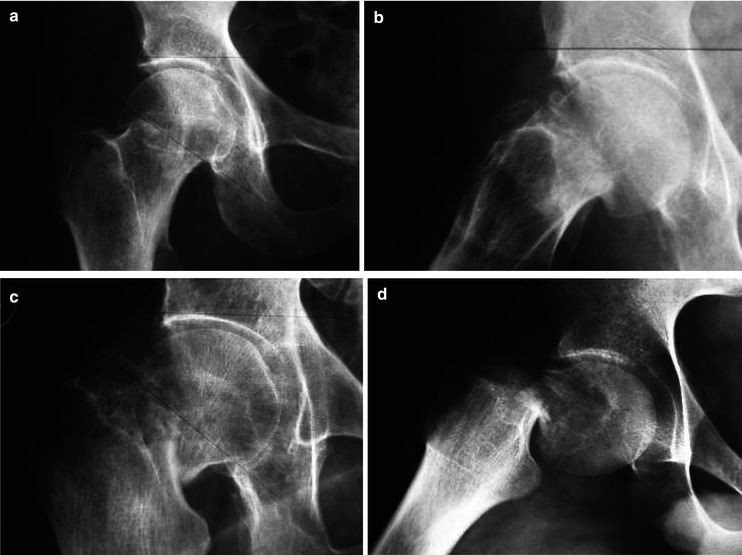
Fig. 19.2
Garden classification [6]: (a) In valgus impacted. (b) Undisplaced. (c) Displaced, fracture surfaces are partial in contact. (d) Displaced, fracture surfaces have lost their contact
19.6.2 Pauwels Classification
This classification describes the mechanical stability of femoral neck fractures with the aim of predicting the probability of the development of a pseudarthrosis (nonunion) or of a femoral head necrosis. The basic principle of this assessment is the Pauwels angle, which is formed between an imaginary horizontal line drawn through the acetabular roofs, for example, and the line drawn through the fracture planes. The magnitude of this angle is inversely proportional to the stability of the fracture. The incidence of nonunion and probably of avascular necrosis of the femoral head is low in pointed angles, whereas the possibility of both complications increases with the magnitude of the angle [11].
Pauwels I: The Pauwels angle is 30°.
Pauwels II: The Pauwels angle is 50°.
Pauwels III: The Pauwels angle is 70°.
The Pauwels angle can only be determined reliably from optimal a.p. images. The first X-rays usually cannot be made, because of immense pain, in the correct a.p. position of the pelvis and of the affected leg; the accurate evaluation of the angle is impossible and therefore unreliable. To be able to determine the treatment of choice, the X-rays must be carried out under completely pain-free circumstances. As a consequence, this classification cannot be considered as an indispensible decision-making aid (Fig. 19.3).
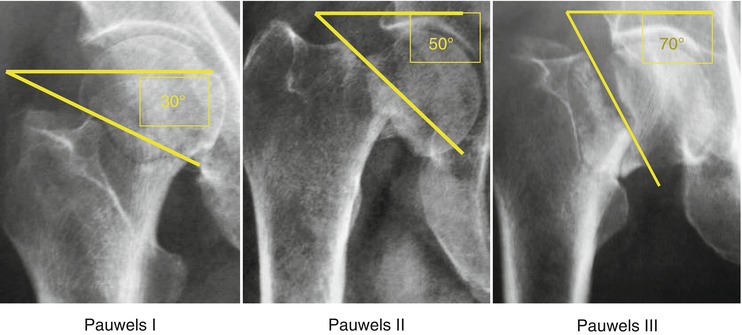
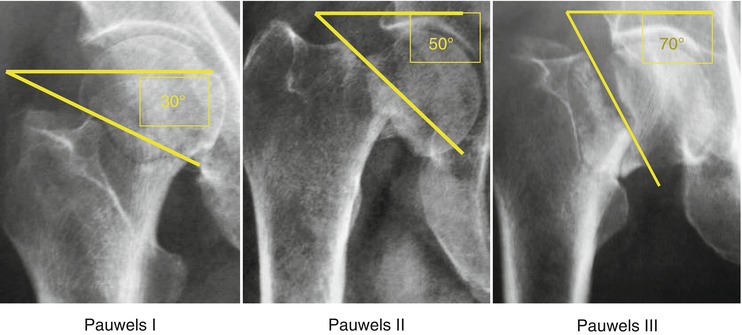
Fig. 19.3
Pauwels classification [11]: (I) The angle between a horizontal line and the fracture line is around 30°. (II) The angle between a horizontal line and the fracture line is around 50°. (III) The angle between a horizontal line and the fracture line is around 70°
19.7 Treatment of Femoral Neck Fractures
19.7.1 Conservative Treatment
19.7.1.1 Indication
Conservative treatment is only indicated in Garden I fractures or in all other fracture forms, if the patient’s general health status does not allow surgical or anesthesiological intervention.
19.7.1.2 Complications
Conservative treatment is connected to all the risks and dangers of long-term bed rest: development of decubiti (sacral, back, and heel), urinary tract infection, pneumonia, pulmonary and cardiac insufficiency, thrombosis and pulmonary embolism. Preventive measures like infection prophylaxis, breathing therapy, and physiotherapy in bed should be prescribed in order to impede the development of thrombosis, decubitus, and infection.
19.7.2 Femoral Head–Preserving Treatment Methods
19.7.2.1 Indication
There is an absolute indication to treat femoral neck fractures surgically. In younger patients (with a biological age between 60 and 65 years), a higher degree of displacement of the fracture fragments is tolerated for head-preserving osteosynthesis. If the femoral head remains vital and heals in a correct position, the patient will have long-term benefits with no further need of any intervention. If not, a corrective surgery using a total hip prosthesis can be performed later on without endangering the patient with good general health status. The usage of a primary total hip arthroplasty in young patients most likely provokes further surgeries with increasing risk of associated complications.
19.7.2.2 Timing of Surgery
The osteosynthesis has to be performed as early as possible after the accident. Surgery performed within 6 h combined with secure stabilization of the femoral neck fracture enables an optimal initial situation resulting in the best achievable outcome.
19.7.2.3 Anesthesia
There are three methods of anesthesia to choose from:
General anesthesia with orotracheal intubation, or larynx mask
Epidural anesthesia or spinal anesthesia
Nerve block anesthesia or local anesthesia
The method of choice depends on the patient’s general state of health, comorbidities, patient positioning during surgery, and length of surgery, as well as on the anesthesiologist’s preference.
19.7.2.4 Operative Techniques
The primary aim of the surgery is an anatomical reduction, which can either be achieved by exposing the fracture through an anterolateral approach to the hip joint (open reduction technique) or by positioning the patient on a traction table with manipulation on the affected leg (closed reduction). A valgus position (hat on the hook) of the femoral head is not desirable for the following reasons:
An overcorrection of the alignment index according to Garden has an adverse effect and corresponds with a bad result, comparable to avascular necrosis of the femoral head.
An intact joint capsule in combination with valgus position of the femoral head can cause obliteration or pinching of the vessels that run cranially on the corticalis or in the joint capsule.
In general, the advantages and disadvantages of the closed method are at equilibrium. However, the closed method is less stressful for the patient and it probably shortens the length of the surgery. Requirements for the usage of the closed method are the availability of a traction table and at least one image intensifier; two image intensifiers facilitate reduction control significantly.
Because of repetitive burden, direct and indirect radiation exposure to the surgical team should be measured by digital dosimeters. The single exposure of a patient can be disregarded because it is small; additionally, all parts of the body lying outside the operation area are protected by lead covers.
After appropriately analyzing the fracture, an accurate assembly of the traction table is crucial because excessive traction might damage the n. ischiadicus and especially the n. peroneus. In rare cases, an anatomical reduction cannot be achieved using the closed method, therefore causing the need to proceed to an open version. Tolerating an incomplete or insufficient reduction is a mistake.
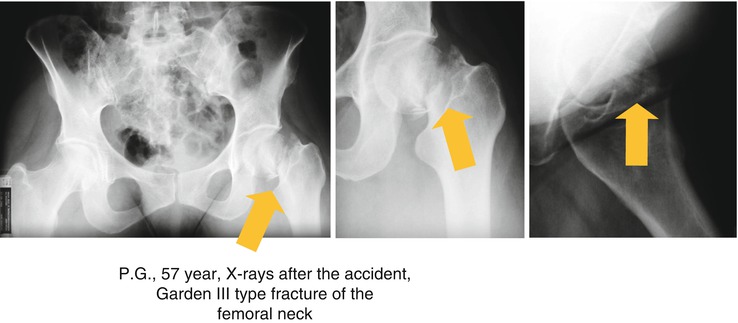
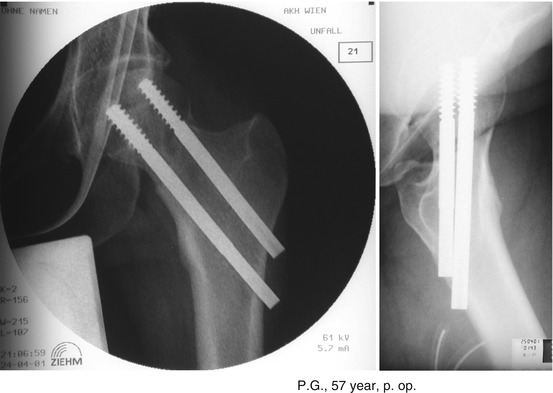
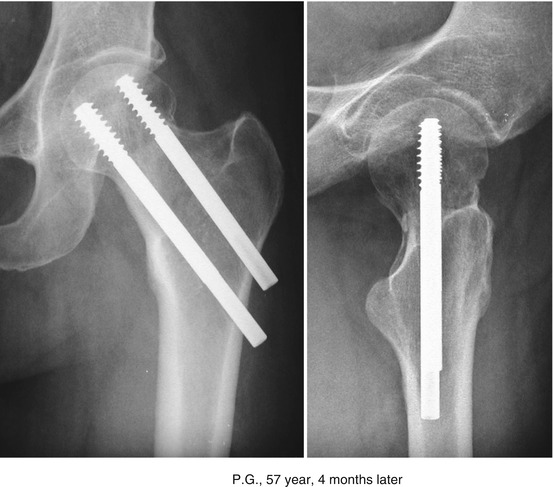
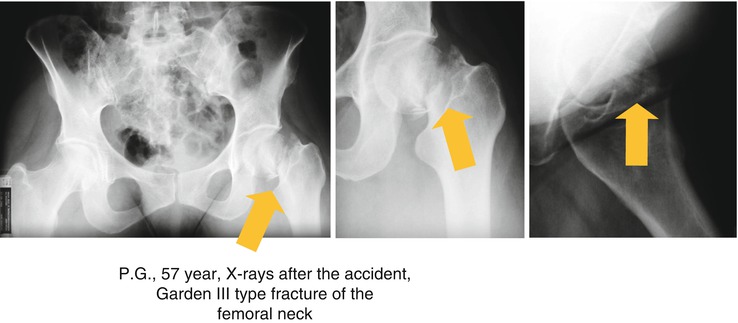
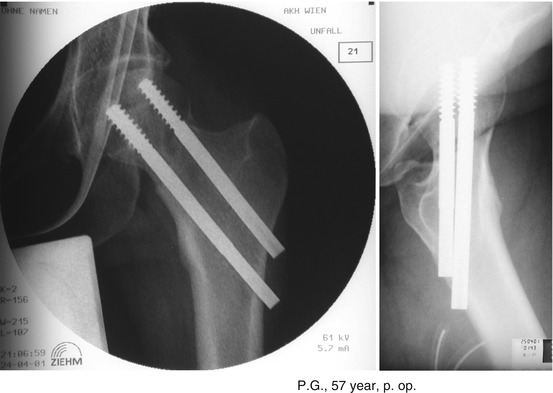
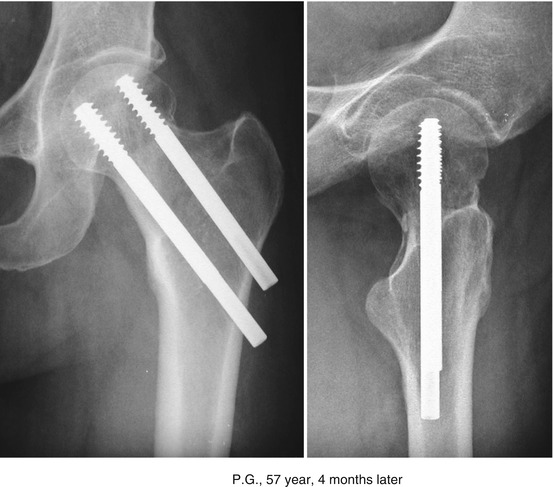
Fig. 19.4
Femoral neck fracture – Type Garden III – Head saving procedure with two cannulated screws. (1) X-rays after the accident. (2) X-rays postoperative 6 h later. (3) X-rays 4 months later. The fracture is consolidated
Screws
After anatomical reduction of the fracture, three to four cancellous bone screws are applied parallel through laterally placed stab incisions on the skin. In the case of using four screws, each of them is placed in the middle of the four quadrants; in the case of using only three screws, they are positioned like an upright triangle, with two screws in the middle of the two caudal quadrants. The position of the screws must be parallel to the femoral neck axis at an angle of approximately 130° to the femoral shaft axis according to the CCD angle. To achieve an optimal position of the implants, cannulated screws are preferred. With their use, it is easier to position the guide wires and, if necessary, to change their position without any damage. Furthermore, target devices for proper placement are available. Classical cancellous bone screws have a core diameter of 4.5 mm and an external one of 6.5 mm; the length of the screw thread used is 15 mm or 30 mm.
The screws must be inserted in a way that their thread is only located in the head fragment, allowing the lateral part of the screw to glide in the trochanteric region. In consequence, repetitive compression force on the head will not be hindered and a fracture gap between the fragments can be prevented. For better anchorage of the screw in the bone, the tips should be placed as close as possible to the subchondral surface of the head (2–3 mm distance). In order to achieve sufficient compression of the fracture areas, washers should be used in combination with conventional spongiosa screws. Compression forces on the fracture side provoke a shortening of the femoral neck length resulting in a protrusion of the screws over the lateral corticalis, which can be seen on the X-ray after several weeks or months.
In addition to the classical spongiosa screws, special femoral neck screws for treating femoral neck fractures are offered by several manufacturers (Fig. 19.4). These special cannulated shaft screws with an exterior diameter of 7.5–9.5 mm do not have a head. Their thread length is less than 20 mm. Little holes are situated in the pitch of screw thread to enable drainage of the intraosseous hematoma or edema. The cannula and holes are furthermore designed for inserting hook-pins, which can be driven into the spongiosa at the tip of the screw. This can clearly enhance the stability of the screw anchorage.
With screws of larger diameter (8.5 mm and 9.5 mm), two screws are generally used to stabilize the fracture. The cranial screw should be inserted as high as possible in the a.p. view. In the axial view, it should be placed slightly anterior to the middle of the femoral neck. The caudal screw should be positioned as low as possible, close to the Adam’s arch in the a.p. view and posterior to the middle of the femoral neck in the axial view. The correct position of the two screws should prevent their diagonal displacement, which can be caused by rotation of the head fragment. Many of these screw systems can be complemented with a one-hole side plate. Connecting of the peripheral screw end with the plate should counteract a secondary varus displacement of the head fragment.
The Dynamic Hip Screw [16, 17]
After reduction of the femoral neck fracture, the axis of the femoral neck has to be elongated virtually to the skin level of the lateral side of the thigh, indicating the correct starting point for an incision of 10–15 cm length. After splitting of the fascia, the origin of the vastus lateralis on the septum intermusculare is dissected from posterior to anterior and perforating vessels of the septum are ligated. With the help of the target device, a 2-mm guide wire with a threaded end is drilled from the lateral corticalis into the anatomical middle of the femoral head until the tip lies in a subchondral position. Afterwards, length measurement has to be made to evaluate the intraosseus distance from the lateral corticalis to the surface of the femoral head, keeping in mind that a 5–10 mm gap between the tip of the screw and the surface of the head should be preserved. In the case of less distance to the surface, cracks of the cartilage can occur, causing an intraarticular bleeding. If the screw tip is further away than 10 mm, the anchorage in the femoral head fragment could be too short and therefore too weak, eventually resulting in a lateral slipping of the screw. After choosing the adequate screw length, the triple reamer is set to the length of the implant selected.
After the triple reamer, the tap is used. According to better bone quality, the risk of an unintended rotation of the head fragment increases, resulting in a destruction of all remaining connections between the head and the neck fragment. To avoid this mischance, a second guide wire can be inserted parallel to the first one in a way that there is enough space between them to not impair further operative procedures. As a next step, the head screw has to be implanted in a way that the screw thread is solely situated in the head fragment. Then the usually used two-hole DHS plate is slid onto the screw until it has full contact with the lateral corticalis. Finally, the plate is fixed with the designated number of corticalis screws. The head screw can now be pulled into the sleeve until the desired compression between the fracture fragments is achieved, aiming to counteract a secondary contortion of the head fragment in the course of time. Because this compression screw will loosen during healing, it should be removed immediately after completion of this step. Subsequently, cyclic load should enhance further compression. Wound closure has to be performed according to the generally valid guidelines. Postoperatively, X-rays in two planes should be performed to verify the correct placement.
19.7.2.5 Special Aspects of Garden Fractures [12, 13]
In case of correct radiologic diagnosis of the impaction (see Classification), Garden I fractures detach between 41 and 52 % of the time, resulting in a dramatic impairment of the prognosis with regard to the vitality of the femoral head. As a consequence, head-preserving osteosynthesis is counterproductive. A secondary displacement is observed in 10 % of the patients under the age of 70 years and in 42 % of the patients over 70 years. Therefore, in order to improve the results, these fractures must be treated surgically as early as possible. Postoperative mobilization should be carried out according to the usual criteria. Of course, patients who are classified as inoperable have to be considered as an exception (Table 19.1).
Table 19.1
Treatment algorithm – femoral neck fracture (FNF)
FNF | Garden I, Garden II | Garden III, Garden IV |
|---|---|---|
Diagnosis | X-ray, CT, MRI | X-ray |
Conservative therapy | Garden I + bad general condition | Bad general condition |
Head saving procedure | Yes | Age dependent |
Time of surgery | Acute! | Acute! |
Open reduction | Exceptional, not needed as a rule | Exceptional, not needed as a rule |
Closed reduction + fracture table | As a rule | As a rule |
Intracapsular hematoma | Evacuation age dependent | Evacuation age dependent |
Hemi-arthroplasty (HHP) | No | Age dependent |
Total arthroplasty (HTAP, HTEP) | Exceptional | Age dependent |
Ambulation – weight bearing | From case to case | From case to case |
19.7.2.6 Postoperative Treatment
Postoperative treatment consists of wound care, thrombosis prophylaxis, mobilization, and X-ray control.
Younger patients can normally be mobilized with toe-touch weight bearing (10–15 kg load). The reason for this regimen without complete non-weight bearing is the possible negative effect on the healing process caused by distraction of the fracture surfaces as a result of a freely suspended leg.
X-Ray Control
This has to be performed in two planes after mobilization (2–5 days postoperatively), after 14 days, and then every 4 weeks until osseous healing of the fracture is evident. Afterwards, follow-up X-rays are only indicated in the case of apparent or increasing discomfort.
19.7.2.7 Complications
Wound Hematoma
In very rare cases, wound hematomas are pronounced enough to necessitate revision. If the surgical wound is tense, if excessive bloody drainage is observed, or if blood loss is detected compared to the postoperative lab control, a wound revision has to be performed, being aware of the clotting status. All wound layers have to be opened and irrigated, thoroughly searching for the source of bleeding. A tissue or swab sample for bacterial-microbiological examination is necessary. After drainage of each layer and wound closure, consecutive monitoring is obligatory. Furthermore, antibiotic prophylaxis is recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








