Femoral Neck Fracture
Thuan V. Ly and Marc F. Swiontkowski
Key Points
• Variables such as time to surgery, role of capsulotomy, and the method of fixation remain debatable.
Introduction
Intracapsular femoral neck fractures are common in the elderly population after a simple fall.1 However, femoral neck fractures in physiologically young adults are less common and represent approximately 5% of the total.2–4 These younger patients are active, have minimal medical problems, and have good bone quality. Femoral neck fracture in these young patients generally occurs after a motor vehicle accident or other high-energy mechanism. It is important to understand the osseous and vascular anatomy, the mechanism of injury, associated injuries, the fracture pattern, and the goals of treatment. Although achieving anatomic reduction and stable internal fixation is imperative, other treatment variables, such as time to surgery, the role of capsulotomy, and fixation methods, are debated. Knowledge of treatment options and potential complications is beneficial in understanding and managing femoral neck fracture in young adults.
Anatomy
Femoral head blood supply comes from three main sources: the medial femoral circumflex artery (MFCA), the lateral femoral circumflex artery (LFCA), and the obturator artery.5–8 The largest contributor to the femoral head, especially the superolateral aspect of the femoral head, is the MFCA.8 The lateral epiphyseal artery complex originates from the MFCA and courses along the posterosuperior aspect of the femoral neck before supplying the femoral head. Terminal branches supplying the femoral head are intracapsular; thus disruption or distortion of these terminal branches likely plays a significant role in the development of osteonecrosis.9–12 Variables that have been hypothesized as contributing to femoral head osteonecrosis include vascular damage from the initial femoral neck fracture,4,12-15 the quality of reduction or fixation of the fracture (restoring flow to the distorted arteries),4,16-20 elevated intracapsular pressure (tamponade from blood),12,21-26 and the position of the implants.27
Indications/Contraindications
Poor bone density, multiple medical problems, and propensity to fall are major risk factors for a femoral neck fracture in elderly patients. In the physiologically young adult, a substantial axial load with the hip in an abducted position is the mechanism that will produce a displaced femoral neck fracture.4,16 Clinical evaluation of these patients should include a thorough trauma workup, as they frequently have other injuries.16,28-30 Diagnosis and treatment of femoral neck fractures in young adults should be done immediately after other life- and limb-threatening injuries are managed. Patients with displaced femoral neck fracture will have a shortened, flexed, and externally rotated lower extremity. For incomplete or nondisplaced fracture of the femoral neck, internal rotation of the limb and heel-strike usually will produce pain in the hip and groin region.
Preoperative Planning
Radiographic evaluation should include anteroposterior (AP) and lateral plain radiographs of the entire femur, as well as an AP radiograph of the pelvis. The fracture pattern seen in young adults is different than that of elderly patients. Elderly patients with poor bone quality or a low-energy injury usually sustain an intertrochanteric hip fracture or a subcapital femoral neck fracture. A transverse fracture pattern with impaction at the fracture site is common. In young adults with better bone quality, higher-energy mechanisms of injury usually cause a basicervical or more distal neck fracture. This occurs from an axially loaded, high-energy force onto an abducted hip. The fracture pattern has a tendency to be more vertically oriented and biomechanically more unstable.31–35 These characteristics have important implications for obtaining and maintaining stable fixation, both of which are necessary for healing to occur.
Despite known limitations, femoral neck fractures in elderly patients are frequently described using the Garden classification.36,37 In this age group, treatment is often based on whether the fracture is nondisplaced or impacted (grades I and II) or displaced (grades III and IV). The Garden classification is not as useful for describing femoral neck fractures in young adults. Pauwels’ classification31 (Fig. 44-1) is more descriptive for young adults with femoral neck fractures. The fracture pattern can indicate the relative stability of the fracture and can predict the difficulty of obtaining stable fixation. A femoral neck fracture line less than 30 degrees from the horizontal plane is a Pauwels’ type I, one that has an angle with the horizontal between 30 and 50 degrees is a Pauwels’ type II, and one that has an angle greater than 50 degrees is a Pauwels’ type III. The type I femoral neck fracture has greater intrinsic stability. Type III femoral neck fractures, the least stable, are seen in young adults more frequently than in the elderly. Type III fracture patterns are more difficult to treat and are associated with increased risks of fixation failure, malunion, nonunion, and osteonecrosis, probably because of greater shear at the fracture site related to the vertical nature of the fracture line.31–35
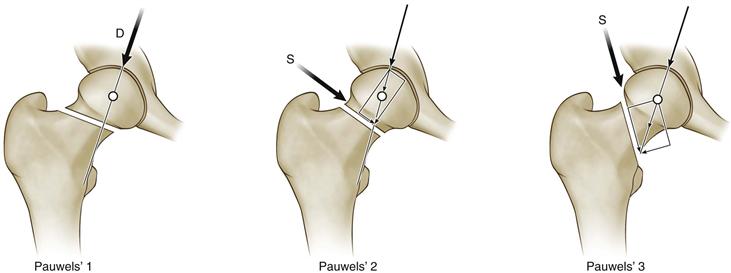
Figure 44-1 Pauwels’ classification. (Modified with permission from Bartonicek J: Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma 15:358–360, 2001.)
Principles of Management and Treatment Algorithm
The authors generally consider patients younger than 65 years old as “young” and those over 75 years old as “elderly.” Patients between 65 and 75 years of age are judged to be young or elderly based on their “physiologic” age. Those who are active and have high functional demands, have good bone quality, and have minimal medical problems are considered “young”; those who have low functional demands (use assistive device for ambulation), chronic illness, or poor bone quality are considered “elderly.”
For the elderly patient, goals include restoring mobility with weight bearing as tolerated and minimizing complications associated with prolonged bed rest. The patient’s age and functional demand make preserving the femoral head less important. A hemiarthroplasty or a total hip replacement often accomplishes this best.38–41
In the physiologically young and active adult, the goals are to preserve the femoral head, avoid osteonecrosis, and achieve union. Avoiding an arthroplasty is highly desirable. It is generally agreed that anatomic reduction with stable internal fixation is paramount for a good outcome. Nevertheless, other issues such as closed versus open reduction, the role of capsulotomy, and time to surgery remain controversial. Method of fixation is also a variable, but it is less controversial.
Fracture pattern alone determines the treatment of nondisplaced fractures. These include both valgus impacted (Garden grade I) and complete but nondisplaced (Garden grade II) femoral neck fractures. They should be treated with internal fixation.42,43 Nonoperative management of nondisplaced femoral neck fractures is associated with higher complication rates and increased risk for displacement.42 Patients should be transferred carefully over to the fracture table to avoid further displacement of the femoral neck fracture. Internal fixation in situ with three cannulated cancellous screws is recommended (Figs. 44-2, 44-3, and 44-4).

Figure 44-2 Anteroposterior radiograph of pelvis, demonstrating displaced right femoral neck fracture.
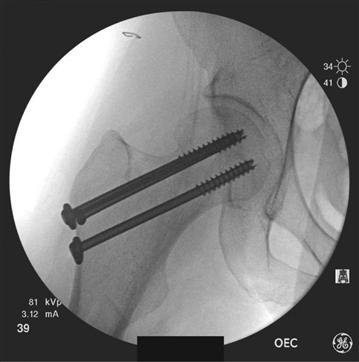
Figure 44-3 Intraoperative C-arm images. Anteroposterior view shows internal fixation with three cancellous screws in an inverted triangle configuration.
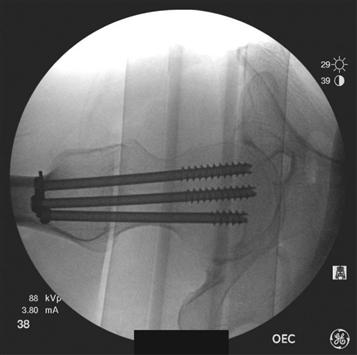
Figure 44-4 Intraoperative C-arm images. A lateral view emphasizes the spread of the three cancellous screws for optimal fixation.
Patient selection for internal fixation can be more difficult with displaced fracture variants.44 Factors to consider when deciding whether to proceed with open reduction and internal fixation of displaced femoral neck fractures include the patient’s chronological and physiologic age, level of activity, bone quality, associated comorbidities, and fracture pattern and characteristics. Although multiple treatment algorithms have been used and published, the best protocol remains debatable.44–49 It is generally recommended that displaced femoral neck fractures in patients who are physiologically younger than age 65 years should have an open reduction and internal fixation. Patients over the age of 75 years with low-energy injuries, poor bone quality, and displaced subcapital fracture patterns should be considered candidates for hemiarthroplasty or total hip arthroplasty (THA) to avoid the higher rate of secondary operations.50 As for patients between the ages of 65 and 75 years, the trend in the treatment algorithm is to perform a THA, especially if they are active and have high functional demands.51–53
Arthroplasty has been reported to have less revision surgery, more rapid mobilization, and better function.39,50,52 Bhandari and associates50 published a meta-analysis comparing internal fixation with arthroplasty (hemiarthroplasty, bipolar arthroplasty, and total hip arthroplasty) for treatment of displaced femoral neck fractures. They reviewed 14 studies with a total of 1933 patients. They concluded that performing arthroplasty for displaced femoral neck fracture reduced the risk of secondary operation. Secondary operation after internal fixation was often a result of nonunion and avascular necrosis. However, infection rate, blood loss, and operative time were increased in the arthroplasty group. More recent randomized controlled trials by Blomfeldt and colleagues39 and Keating and coworkers52 also reported a decrease in reoperation rate with arthroplasty. Blomfeldt and associates39 evaluated outcomes at 4 years of mentally competent, relatively healthy elderly patients who underwent internal fixation or THA for displaced femoral neck fracture. The rate of reoperation was 47% for internal fixation and 4% for THA. Using the Charnley score and the EuroQol-5D (EQ-5D) index to assess hip function and health-related quality of life, respectively, investigators concluded that THA performed better. Keating and colleagues52 randomized 207 patients and compared reduction and fixation, bipolar hemiarthroplasty, and THA. They reported reoperation rates of 39% for the fixation group, 9% for the THA group, and 5% for the hemiarthroplasty group. Arthroplasty was found to have better functional outcomes as measured by a hip rating questionnaire and the EQ-5D index.
Hemiarthroplasty is the preferred treatment for low-functioning community or nursing home ambulatory patients. Performing hemiarthroplasty in more active, mobile, and independent living older patients raises concerns for acetabular erosion, as well as poor functional and pain ratings. Baker and coworkers38 randomized 81 active individuals to THA or hemiarthroplasty for displaced femoral neck fracture. At a mean follow-up of 3 years, fewer complications, improved walking distances, and a higher Oxford Hip Score were noted for the THA group. More than 60% of living patients in the hemiarthroplasty group showed acetabular erosion on radiograph. In another randomized controlled trial, Blomfeldt and associates52a compared bipolar hemiarthroplasty with THA for displaced femoral neck fracture in active and lucid patients. They showed that THA resulted in better hip function (Harris Hip Score) but no significant difference in the health quality-of-life measure between the two groups. In summary, evidence suggests that THA is the better treatment for displaced femoral neck fracture in the right patients. These include patients >65 years of age who are competent, active, and community ambulatory, with preexisting hip disease (osteoarthritis, rheumatoid arthritis).53,53a
The author’s preferred treatment algorithm is to perform arthroplasty for patients age >65 years with poor bone quality and a high degree of comminution. THA is preferred for patients who are community ambulators who are lucid, independent, and have a life expectancy >5 years. Hemiarthroplasty is ideal for patients who are low-demand, minimal ambulators who have cognitive impairment and a short life expectancy. No evidence indicates superior function or durability of bipolar as compared with unipolar, and unipolar is more cost-effective. Cemented stems are recommended for patients with poor bone quality or low demand. The authors reserve uncemented stems for patients with good bone stock who have higher functional demands and are younger.
Description of Technique(s)
Surgical Approach
After the patient is medically optimized, surgical fixation of the femoral neck should proceed expeditiously. The injured limb should be left shortened and externally rotated while surgery is awaited. Several authors have shown that intracapsular pressure changes vary with hip position in femoral neck fracture.22,26,54 Intracapsular pressure is greatest when the hip is in extension with internal rotation, and decreases significantly when the hip is in flexion with external rotation. Preoperative skin traction is ineffective in reducing pain and avoiding complications.55–58
Closed reduction is attempted by flexing the hip to 45 degrees with the hip slightly abducted, then extending and internally rotating the leg while applying longitudinal traction. The quality of the reduction is judged on the basis of the fluoroscopic image before percutaneous fixation is performed. Only an anatomic reduction should be accepted; otherwise proceed with an open reduction and internal fixation.45,59,60 The authors’ preference is to have the patient in the supine position, on a radiolucent table, with the leg draped free, but some prefer to have the patient in traction on a fracture table. The supine position provides optimal visualization for fracture reduction and ease of fluoroscopic imaging; in addition, other orthopedic or surgical teams can address associated injuries with the patient supine.
If open reduction is required, then a Watson-Jones approach is used61,62 (Fig. 44-5). A straight lateral incision is made over the lateral proximal femur. Proximally, the incision is curved anteriorly toward the gluteal pillar of the ilium. The tensor fascia is retracted anteriorly while the gluteus medius is retracted posteriorly. The pericapsular fat is then swept off to allow visualization of the anterior hip capsule. The vastus lateralis can be slightly elevated off the greater trochanteric ridge for further visualization. A T-capsulotomy, with release of the capsule of the intertrochanteric ridge, is performed in line with the femoral neck. This allows decompression of the hematoma and direct visualization of the femoral neck fracture. The edges of the capsule can be tagged with a suture for retraction. Inserting a small, pointed Hohmann retractor outside the capsule onto the anterior part of the acetabular rim can aid in visualization.
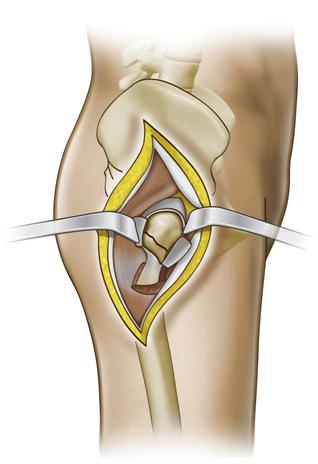
Figure 44-5 Watson-Jones anterolateral exposure to the hip for open reduction of femoral neck fracture. The interval between the tensor fascia and the gluteus medius is exposed. T-capsulotomy with visualization of the femoral neck fracture. (Redrawn from Swiontkowski MF: Intracapsular hip fractures. In Browner BD, Jupiter JB, Levine AM, Trafton PG [eds]: Skeletal trauma, basic science, management, and reconstruction, ed 3, Philadelphia, 2003, Saunders, p 1735.)
For the reduction, a bone hook or a 5-mm Schanz pin can be applied to the distal segment of the fracture. The bone hook can be placed onto the greater trochanter for lateral traction, and the lower extremity can be manipulated and externally rotated. This will disimpact the fracture and facilitate reduction with an internal rotation maneuver. Alternatively, place a Schanz pin from anterior to posterior several centimeters distal to the fracture site. This can aid in manipulation of the distal fragment. For the proximal segment, 2-mm Kirschner wires can be inserted into the femoral head, functioning as joysticks to lift the proximal fragment anteriorly and to reduce the fracture. Once the femoral neck fracture is anatomically reduced by direct visualization of the anterior cortex and is confirmed by fluoroscopic imaging, a Weber clamp or 2-mm Kirschner wires can provisionally hold the reduction (Figs. 44-6, 44-7, 44-8, and 44-9). Definitive fixation can be attained with three cannulated or noncannulated cancellous screws (Fig. 44-10). Closure starts with loose reapproximation of the capsule with nonabsorbable sutures. The fascia and subcutaneous tissue are closed over a drain with absorbable sutures, followed by dermal sutures or staples for the skin. Another approach using a modified Smith-Peterson surgical exposure has been described.63 This allows direct access to and visualization of the femoral neck fracture, especially the subcapital region. However, a separate incision is required for implant insertion.

Figure 44-6 Anteroposterior radiograph of pelvis, displaced right femoral neck fracture from motor vehicle accident.

Figure 44-7 Intraoperative C-arm images. Anteroposterior view demonstrating utilization of 5-mm Schanz pin and Weber clamps to reduce the femoral neck fracture.

Figure 44-8 Intraoperative C-arm images. Lateral view demonstrating utilization of 5-mm Schanz pin and Weber clamps to reduce the femoral neck fracture.

Figure 44-9 Anteroposterior radiograph showing a healed femoral neck.
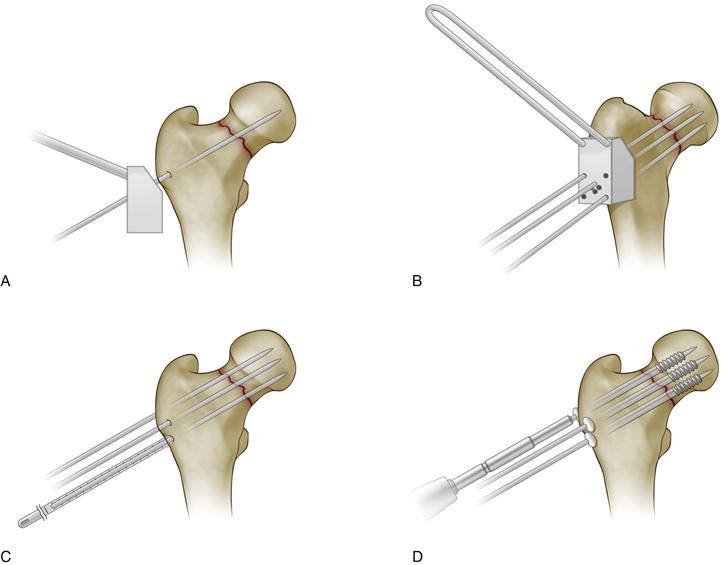
Figure 44-10 Internal fixation of a femoral neck fracture with a cannulated screw system. A and B, Reduction is confirmed and three parallel guide wires are placed using the guide and fluoroscopic control. C, Lengths of the wires are measured. D, Screws are inserted over the guide wires to a preselected depth. (Redrawn from Swiontkowski MF: Intracapsular hip fractures. In Browner BD, Jupiter JB, Levine AM, Trafton PG [eds]: Skeletal trauma, basic science, management, and reconstruction, ed 3, Philadelphia, 2003, Saunders, p 1737.)
Variations/Unusual Situations
Ipsilateral femoral neck fracture can occur in 2% to 6% of all femoral shaft fractures.64–71 These concomitant ipsilateral injuries can be challenging to reduce, and the best methods of fixation are debatable.64,66,71 The femoral neck fracture is often a Pauwels’ type III and nondisplaced. Treatment of the femoral neck should be a priority in the sequence of managing this combination. Methods of fixation include sliding hip screw (SHS) and a long side plate, cancellous screws or an SHS and a retrograde intramedullary nail or plate fixation of the shaft fracture, cephalomedullary (second-generation) nails, and a proximal femoral locked plate. A recent retrospective review of 40 patients with ipsilateral femoral neck and shaft fractures suggested that the preferred method is open reduction and internal fixation of the femoral neck with cancellous screws or SHS and retrograde nailing of the shaft fracture. This method resulted in greater accuracy of reduction and improved healing of fractures.65
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








