, Ratna Johari2 and Shalin Maheshwari2
(2)
Pediatric Orthopedics, Childrens’ Orthopedic Centre, Mumbai, India
Take-Home Message
The most common cause of a late failure after initial club foot correction with Ponseti casts is poor compliance with the Denis Browne brace.
Most club feet treated with the Ponseti method (up to 90 %) require percutaneous Achilles tenotomy at the time the final cast is applied.
Anterior tibial tendon transfer (split or whole transfer) is needed in one third to one half of club feet treated with the Ponseti method.
Definition
Club foot is a congenital foot deformity consisting of hindfoot equinus and varus as well as midfoot and forefoot adduction and cavus. It is more common in males and is the most common birth defect (1 in 750 live births).
Aetiology
Considered to be multifactorial
Mechanical block by extrinsic pressure in utero
Primary germ plasm defect in the talus
Retracting fibrosis—myofibroblast contraction
Neurogenic theory—increased type 1 muscle fibres in the calf muscle
Myogenic theory—atrophy of leg muscles
Hypotrophic anterior tibial artery
Genetic factors
Pathoanatomy
The talus is smaller, and there is short talar neck. There is medial and plantar deviation of the anterior end of the talus. Talar neck body axis is reduced to less than 90°.
The axes of the anterior and middle facet of the calcaneus create a more acute angle than a normal foot, with the anterior facet oriented inward. Calcaneus is medially rotated and pronated.
There is talonavicular subluxation. The navicular is displaced medially over the head of the talus. The forefoot deformity is the result of medial displacement of the navicular.
Although the entire foot is supinated, the forefoot pronation relative to the hindfoot causes the cavus.
Among the various structures that may be abnormal and contribute to the deformity are the gastrocnemius–soleus and the tibialis posterior. These muscles may be contracted.
Other soft-tissue contractures, including the joint capsules, develop subsequently. In longstanding cases, adaptive bony changes ensue.
Evaluation
Common clinical findings are a small foot, small calf and slightly shortened tibia, and the skin creases medially and posteriorly.
Nonidiopathic club feet must be identified. Club feet associated with arthrogryposis, myelodysplasia, diastrophic dysplasia and amniotic band syndrome are resistant to casting treatment.
Radiography: Minimal ossification of the foot in the newborn limits the utility of radiographs. In both the AP and lateral views of a club foot, the talus and calcaneus are less divergent and more parallel (smaller talocalcaneal angle) than normal.
Classification
Dimeglio Classification
Each major components of club foot (equinus, heel varus, medial rotation of carpopedal block, forefoot adduction) are given points accordingly.
−20° and 0°: 1 point
0–20°: 2 points
20–45°: 3 points
45–90°: 4 points
Additional 1 point each are added for the following:
Deep posterior crease
Medial crease
Cavus
Poor muscle condition
Grade I: if score less than 5
Grade II: if score is 5–9
Grade III: if score is 10–14
Grade IV: if score is more than 15
Pirani Scoring
Each component may score 0, 0.5 or 1. This includes the following:
Hindfoot contracture score
Posterior crease
Empty heel
Rigid equinus
Midfoot contracture score
Medial crease
Curvature of lateral border
Position of the head of the talus
Treatment
Nonsurgical—the Ponseti serial casting.
Outcome is much better than with historical casting techniques (80–90 % success versus 10–50 %).
Sequence of deformity correction is cavus, adductus, varus and finally equinus (CAVE).
Important Ponseti casting concepts:
Forefoot is supinated, not pronated.
Lateral pressure is applied to the neck of the talus only.
Long-leg casts.
Weekly cast changes.
Percutaneous Achilles tenotomy is frequently done before final cast application to address residual equinus (up to 90 % of feet).
The most common cause of failure after initial correction with the Ponseti casting is poor compliance with the Denis Browne brace. Recommended use is 23 h/day for 3 months after casting and then at night for 2–3 years.
Anterior tibial tendon transfer (split or whole transfer) is needed in one third to one half of club feet treated with the Ponseti method.
Surgical
Complete posteromedial release indications: persistent deformity after casting, syndrome-associated club foot and delayed presentation (older than 1–2 years of age). Secondary or residual deformities may require surgical intervention.
Hindfoot varus
<2–3 years: Modified McKay procedure
3–10 years: Isolated heel varus—Lateral closing wedge osteotomy of the calcaneus. Short medial column: Dillwyn Evan’s procedure—this consists of medial and posterior release with calcaneocuboid fusion. Long lateral column: Lichtblau procedure—consists of resection of the lateral end of the os calcis.
10–12 years: Triple arthrodesis
Equinus: Mild to moderate deformity—tendo-Achilles lengthening and post-capsulotomy of the ankle and subtalar joints. Severe deformity—Lambrinudi procedure
Complications
Vascular compromise—immediate placement of cast in neutral position predisposes to this complication.
Injury to infant’s tarsal bone—transaction of the head of the talus and sustentaculum tali can occur during capsulotomies.
Injury to posterior tibial physis, distal fibular physis or first metatarsal physis.
Bibliography
1.
Bensahel H, Guillaume A, Czukonyi Z, et al. Results of physical therapy for idiopathic clubfoot: a long-term follow-up study. J Pediatr Orthop. 1990;10:189–92.
2.
Carroll NC. Pathoanatomy and surgical treatment of resistant clubfoot. Instr Course Lect. 1988;37:93–106.
3.
Dimeglio A, Bensahel H, Souchet P, et al. Classification of clubfoot. J Pediatr Orthop B. 1995;4:129–36.
4.
Ippolito E, Ponseti IV. Congenital clubfoot in the human fetus. A histological study. J Bone Joint Surg Am. 1980;62:8–22.
5.
Ponseti IV. Congenital clubfoot: fundamentals of treatment. Oxford: Oxford University Press; 1996.
2 Metatarsus Adductus
Ashok Johari3 , Ratna Maheshwari3 and Shalin Maheshwari3
(3)
Pediatric Orthopedics, Childrens’ Orthopedic Centre, Mumbai, India
Take-Home Message
Metatarsus adductus is a medial deviation of the forefoot with normal alignment of the hindfoot.
Avoid treating a deformity which spontaneously improves.
Most cases of metatarsus adductus improve; those that improve need no active treatment.
Correction of the deformity should be considered for cases that do not resolve, particularly if the deformity is severe.
Definition
In children born with this foot deformity, the forefoot is deviated inward relative to the hindfoot. Some authors distinguish between metatarsus adductus and metatarsus varus by the degree of rigidity of the deformity, the latter being the stiffer type.
Aetiology
Intrauterine compression has been long presumed as the cause.
Abnormal insertion of tibialis posterior on first cuneiform, or peroneal weakness with overactive tibialis anterior.
May be associated with torticollis and developmental dysplasia of the hip.
Pathophysiology
Shape of medial cuneiform found to be altered, with medial deviation of articular surface
Adduction of metaphysis of the second through fifth metatarsal
Radiography
Medial deviation of metatarsals at the tarsometatarsal level (see Fig. 1)
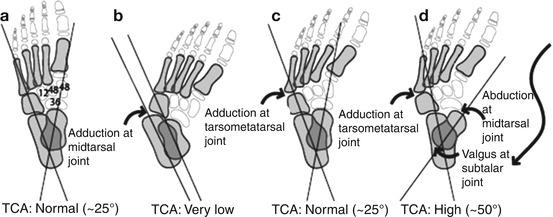
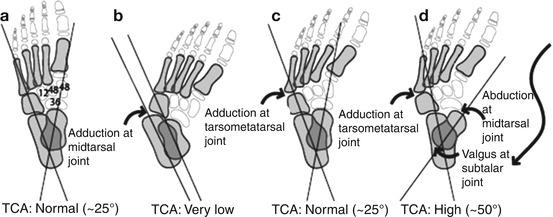
Fig. 1
Talocalcaneal angle in various foot deformities. (a) In the normal foot—the T–C angle is around 25°. (b) In a club foot—The T–C angle is very low. (c) In metatarsus adductus—the T–C angle is normal; however, there is adduction at tarsometatarsal joints. (d) In skewfoot—the T–C angle is very high, with adduction at tarsometatarsal joints
Classification
Bleck Classification
Mild: Forefoot can be clinically abducted to the midline of the foot and beyond.
Moderate: Flexibility to allow abduction of forefoot to the midline, and not beyond.
Rigid: The forefoot cannot be abducted at all.
Treatment
Nonsurgical
Spontaneous resolution of metatarsus adductus occurs in 90 % of children by age 4 years.
Passive stretching is recommended for mild deformity but does not improve final outcome.
Serial casting is useful in children between 6 and 12 months of age with moderate deformity. Unlike cast treatment for club feet, the fulcrum for applying an external rotation torque when moulding the cast is located over the cuboid.
Surgical
Surgery is indicated only in children with severe deformities uncorrected by conservative measures or when there are problems with shoe wear and pain or objectionable appearance.
2–4 years: Tarsometatarsal capsulotomies and/or abductor hallucis release.
>4 years: A medial column lengthening (opening wedge osteotomy of cuneiform) and lateral column shortening (closing wedge of the cuboid) produce good results with fewer complications.
If the child has a skewfoot (hindfoot valgus in addition to the metatarsus adductus), then hindfoot osteotomy is required in addition to the midfoot osteotomy.
Complications
Recurrence is the most common complication.
Bibliography
1.
Asirvatham R, Stevens P. Idiopathic forefoot-adduction deformity: medial capsulotomy and abductor hallucis lengthening for resistant and severe deformities. J Pediatr Orthop. 1997;17:496–500.
2.
Heyman CH, Herndon CH, Strong JM. Mobilization of the tarsometatarsal and intermetatarsal joints for the correction of resistant adduction of the fore part of the foot in congenital club-foot or congenital metatarsus varus. J Bone Joint Surg Am. 1958;40:299–309.
3.
Ponseti IV, Becker JR. Congenital metatarsus adductus: the results of treatment. J Bone Joint Surg Am. 1966;48:702–11.
3 Congenital Vertical Talus
Ashok Johari4 , Ratna Maheshwari4 and Shalin Maheshwari4
(4)
Pediatric Orthopedics, Childrens’ Orthopedic Centre, Mumbai, India
Take-Home Message
The diagnosis of the vertical talus should prompt the orthopaedic surgeon to look for neural tube defects or arthrogryposis.
Early use of nonoperative treatment (usually manipulation and serial casts) in combination with limited surgery appears to be an evolving general principle in the management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






