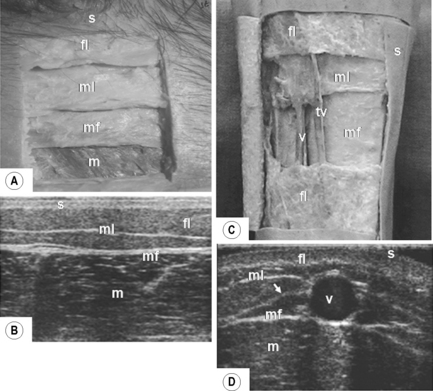
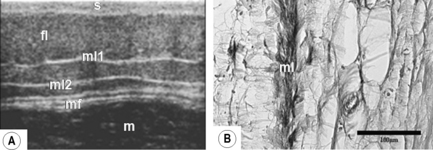
1.3 Fascia superficialis Skin, comprising epidermis and dermis, covers the whole surface of the body and is its largest organ. Immediately subjacent is an enveloping layer of dense and areolar connective tissue and fat called the superficial fascia (synonyms – fascia superficialis, hypodermis, subcutaneous tissue, tela subcutanea) (Standring et al. 2008; Langevin & Huijing 2009). Being co-extensive with the skin, it too comprises a very considerable tissue mass that conveys blood vessels and nerves to and from the integument. The subcutaneous tissue connects the skin to the underlying dense deep fascia which invests muscles and aponeuroses throughout the body. Skin, with the subjacent superficial fascia, provides a protective cushion for the musculoskeletal framework over which they slide. Sheets of collagen fibers coupled with elastin facilitate this mobility (Kawamata et al. 2003). The spaces between the collagen sheets facilitate sliding, whilst stretching results in realignment of collagen fibers within the sheet. Skin shape and position are restored by elastic recoil. The tortuosity of blood vessels and nerves through superficial fascia allows them to accommodate stretching. Van der Wal (2009) considers fascia as a connective tissue continuum throughout the body. Thus subcutaneous connective tissue provides a unique general pathway through and between regions which blood vessels, nerves and lymphatics can traverse (Wood Jones 1946; Benjamin 2009). Its widespread distribution, its mechanical role, and the ability of fibroblasts to communicate via their gap junctions, suggest fascia may form a bodywide mechanosensitive integrating signaling system analogous to that of the nervous system (Langevin 2006) and relevant to interpreting fibrositis. Fiber bundles (retinaculae cutis) traverse the subcutaneous layer from dermis to deep fascia, strengthening their connection. The subcutaneous tissue can be differentiated into a bulky superficial fatty layer, panniculus adiposus, and a deeper, mostly vestigial layer, panniculus carnosus (McGrath et al. 2004). Within the fatty layer itself, a membranous component can also be recognized. Classically, this is seen in the lower abdominal wall as the fascia of Camper (superficial fatty layer) and of Scarpa (deeper membranous layer) (Standring et al. 2008). Recent studies (Abu-Hijleh et al. 2006) indicate that the membranous layer has a much wider distribution in the body than suggested by earlier studies (see below). The fat cells are aggregated into clumps or lobules by fibrous septa. In the adult human the vast majority of the fat is of the white type, with only a very small amount of the energy-rich brown fat. About 20% of body weight in a healthy adult male is white fat and it comprises up to 25% in females. Subcutaneous fat accounts for about 50% of total fat storage in the body. The storage is dynamic, the fat itself within the cells being renewed every 2–3 weeks. The amount and distribution of the fat varies with age, sex, and site. In infants and young children its distribution is quite uniform through all regions (except for the suctorial pad in the cheek). It increases steadily in amounts throughout early childhood. In adults the number of fat cells remains constant, the actual number being established during childhood and adolescence and under genetic control. Nevertheless, it has been found that approximately 10% of fat cells are renewed annually in adults (Spalding et al. 2008). In old age there is a decrease in fat. Concerning the sexes, subcutaneous fat is thicker in females, as evidenced by their smoother body contours. Measurements of subcutaneous tissue in the anterolateral aspect of the thigh recorded a depth of 0.74 cm in males and 1.74 cm in females (Song et al. 2004). Using an objective assessment of limb subcutaneous tissue elasticity by an indentation technique, Zheng et al. (1999) noted that the tissue thickness increases by 26% when the underlying muscle contracts. With regard to site differences, fat is particularly thick in the buttocks, hips, waist, thighs, soles, palms, breast, and cheeks. It is thinnest or absent in eyelids, lips, pinna (excluding the lobule), external nose, penis, scrotum, and labia minora. A distinct membranous layer in the superficial fascia in restricted areas of the body, including the lower anterior abdominal wall (Scarpa’s fascia), and perineum (Colles’ fascia) is well documented. A membranous layer is also present in relation to the saphenous veins (Caggiati 2000, 2001). More recently, a well-defined membranous sheet was found in the superficial fascia of many regions of the body (Abu-Hijleh et al. 2006; Fig. 1.3.1), its arrangement and thickness varying according to gender, region, and the surface studied. This sheet is more prominent on the posterior aspects of the trunk and extremities than on the anterior. In certain regions, such as the periphery of the female breast, arm, back, and thigh there may be more than one membranous layer separating the fat into two or more layers (Fig. 1.3.2). The superficial fascia in the face differs from other regions. Macchi et al. (2010) have shown that the superficial fascia has a laminar connective tissue layer (the superficial musculoaponeurotic system, SMAS; Mitz & Peyronie 1976). It is interposed between superficial and deep fibroadipose layers. The superficial layer connects the dermis with the superficial aspect of the SMAS. The deep layer connects the deep aspect of SMAS to the parotid–masseteric fascia. Adipose lobules occur within both layers. 1. Interstitial fluid: Subcutaneous tissue contains a rich plexus of lymphatics and lymphatic capillaries. There is a dynamic balance between production of tissue fluid from blood capillaries and its absorption into subcutaneous lymphatics. Drainage is assisted by contraction in underlying muscles. Normally there is a negative pressure of − 2 or − 3 mmHg (Sven & Josipa 2007), which is influenced by external atmospheric pressure acting on the skin surface. Disturbances in the normal dynamics of tissue fluid formation may increase the pressure, fluid accumulating and resulting in edema, the distribution of which is influenced by posture. It may be shown by “pitting” of the skin in response to locally applied pressure. Conversely, fluid may be lost, as in severe dehydration. 2. Force absorption: Subcutaneous mixtures of “fibroadipose tissue” function as important pressure absorbers withstanding compressive and shearing forces on the body surface (Benjamin 2009). The best examples are seen in the palm of the hand and sole of the foot, particularly the fat-pad of the heel where strong fibrous septa pass from the dermis deeply to the plantar aponeurosis, dividing the fat into clearly defined compact lobules. 3. Thermal insulation: Subcutaneous fat insulates the body against heat loss. The greater the thickness of fat, the more effective is the insulation. This is particularly important in warm-blooded terrestrial animals. 4. Energy source: Subcutaneous fat provides a very significant reserve of stored energy (Marks & Miller 2006). The source of energy is triglyceride, which contains oleic and palmitic acids present in the fat droplets of the adipocytes. In severe starvation the body’s subcutaneous fat is utilized, resulting in tissue shrinkage. Brown fat, which is more abundant in newborns, provides a rapid source of energy and heat. 5. Vascular arrangements: Superficial veins lying in the subcutaneous tissues may be quite large and easily visible, especially in limbs, where they are available for intravenous injection or transfusions. Studies on the saphenous veins in the lower extremities indicate that they lie interfascially rather than subfascial (Papadopoulos et al. 1981; Caggiati 2001). Each vein lies within a compartment delimited by two fasciae: the muscular fascia deeply and the membranous layer superficially. The two fuse peripherally, forming a deep compartment of the hypodermis resembling an “Egyptian eye” shape when viewed by ultrasonography (Fig. 1.3.1) (Caggiati 2000; Abu-Hijleh et al. 2006). Within their compartments the veins are anchored by a connective tissue lamina. Tributaries of the saphenous veins course superficial to the membranous layer in the subdermal fatty layer (Fig. 1.3.1) (Caggiati 2001; Abu-Hijleh et al. 2006), lacking fascial wrapping in contrast to the main veins. A similar arrangement exists along the cephalic vein and its tributaries in the upper extremity (Abu-Hijleh et al. 2006). There are also fascial canals in the fingers (Doyle 2003) containing digital vessels and nerves.
Introduction
Gross structure and distribution
Components and their relation to function
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine