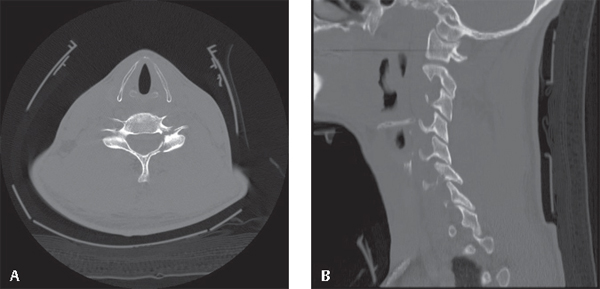
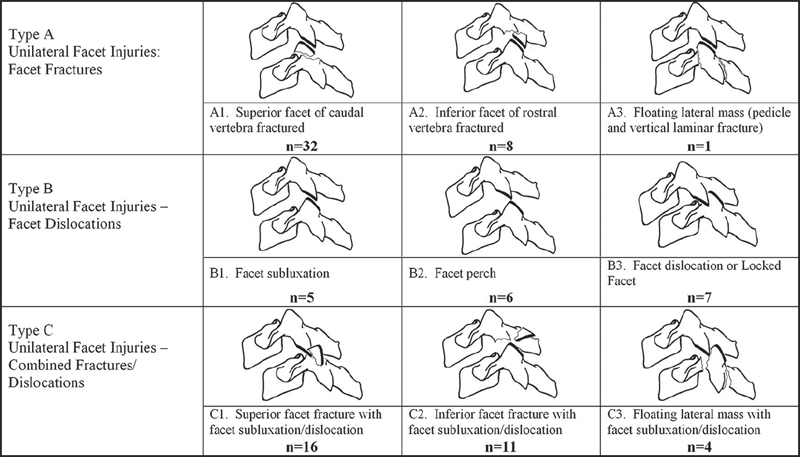
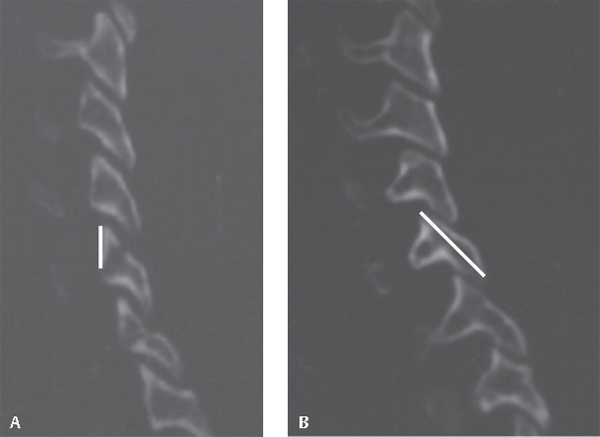
10 Facet fractures account for ~ 7% of all cervical spine fractures. Ninety percent of injuries occur at the C5–C7 levels. Isolated facet/lateral mass fractures of the cervical spine are rarely distinguished from subluxed, perched, locked, or dislocated facets in the literature. Subluxations and dislocations are commonly produced by a flexion moment, axial compression, and anterior shear, and may frequently be associated with neurological injury. The management of perched, locked, and dislocated facet injuries is addressed in Chapter 8. In contrast, isolated facet fractures are thought to be due to extension, side bending and rotation forces, or rotational forces on a flexed neck. The most common injury pattern is that of an undisplaced or minimally displaced superior facet fracture, followed by a more obviously displaced superior facet fracture. Facet fractures are often missed on initial presentation and may lead to axial neck pain, radiculopathy, or focal kyphosis if they displace. Acute instability may occur if associated with discoligamentous injury. Fractures of both the facet and pedicle/lamina result in fracture-separation/“floating” lateral mass, which is considered an unstable injury (Fig. 10.1). This presents a challenge because two motion segments are involved, although subluxation occurs most frequently at the more caudal of the two disrupted motion segments. Neurological injury may occur as a result of foraminal injury to a single nerve root. Patients with congenitally small or spondylotic spinal canals may exhibit signs of cord injury secondary to cervical hyperextension or associated traumatic disk herniation. There is no universally accepted classification for facet fractures of the subaxial cervical spine. Isolated facet fractures have been classified by Allen and Ferguson’s mechanistic system as stage I compression-extension injuries. This includes unilateral fractures with or without antero-rotary vertebral displacement. Fracture patterns may consist of linear, nondisplaced, compressive, or pedicle and laminar fractures producing a floating lateral mass. White and Panjabi did not specifically address facet fractures but defined clinical instability based on patterns of displacement (sagittal plane translation > 3.5 mm or kyphosis > 11 degrees), anterior/posterior column destruction, and clinical findings. The AO classification, based on mechanism of injury, was developed for the thoracolumbar spine but is often applied to the cervical spine. The AO classification is not really relevant to, nor has it been validated in, the subaxial cervical spine. Vaccaro described the Subaxial Injury Classification (SLIC) severity scoring system, which gives gradated points for injury morphology, discoligamentous injury, and neurological status. The SLIC system uses the aggregate score to direct management to either surgical or nonoperative paradigms. Kotani proposed a unique classification system for lateral mass fractures based on morphology (separation, comminution, split types and traumatic spondylolysis) based on a series of 31 patients. Dvorak classified unilateral facet injuries based on the presence of facet fracture, the degree and pattern of subluxation or dislocation, or the combined presence of fracture and subluxation or dislocation (Fig. 10.2). Fig. 10.1 Unilateral fracture involving both pedicle and lamina. (A,B) Axial CT scan demonstrating “floating lateral mass.” (B) Sagittal reformats demonstrating the “horizontalized” C6 facet/lateral mass complex. Facet fractures are most commonly the result of motor vehicle accidents, falls, or sports injury. Acutely, patients describe axial neck pain aggravated by neck movement. Transient or persistent radiculopathy due to impingement on the root in the intervertebral foramen may cause significant arm symptoms of pain, numbness, and weakness and may be the patient’s sole complaint. New radicular symptoms may develop in a delayed fashion due to progressive slip. Fig. 10.2 Classification system for unilateral subaxial facet injuries based on 90 unilateral facet injuries. Type A fractures may be treated nonoperatively with external orthosis and close follow-up if there is no kyphosis or displacement on upright radiographs. Type B and C injuries that are subluxed are generally treated operatively. Type C injuries associated with dislocation or locked facets are addressed in Chapter 8 of this volume. (From Dvorak MF, Fisher CG, Aarabi B, et al. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine 2007;32:3007–3013. Reprinted with permission.) Simple isolated facet fractures rarely present with spinal cord injury (SCI), although SCI may occur as a result of either a concomitant disk herniation at the level of the fracture, a congenitally narrow spinal canal, or the possibility that a nearly dislocated facet may have reduced and may masquerade as a less severe injury. Neck pain on palpation may localize the injury. Radiculopathy resulting in motor, sensory, and reflex loss should be elicited. Unexplained neurological deficits may be secondary to other noncontiguous injuries or possibly even a traumatic vertebral artery dissection. A careful examination of the visual fields and cerebellar and lower cranial nerve function may suggest a more central neurological etiology, which may have resulted from an embolic event. Facet fractures can easily be missed on screening radiographs. Understanding fracture morphology, associated vertebral body fracture, and involvement of the upper or lower facet complex can be achieved by reviewing both the axial and reformatted computed tomography (CT) scanning images. Evidence of discoligamentous injury (segmental kyphosis and vertebral translation) should be measured on sagittal reformatted CT images or on plain radiographs. Vaccarro predicted failure of nonoperative management if the craniocaudal height of the fracture fragment was > 1 cm or the ratio to the intact lateral mass was < 40% based on sagittal CT images (Fig. 10.3A,B). Magnetic resonance imaging (MRI) is the most reliable modality for identifying diskoligmentous injury, disk herniation, and neurovascular injury. CT or MR angiogram should be ordered if vertebral artery injury is suspected. The head and brain should be included in the imaging when there is suspicion of embolic events or a more central neurological deficit. Patients treated nonoperatively should be mobilized in an external orthosis. Upright radiographs and an assessment of the patient’s pain and clinical neurological status are an important component of clinical management. When there is an increase in the patient’s local neck pain, new or progressive nerve root deficit, radiographic evidence of vertebral translation of greater than > 2 mm, or significant segmental kyphosis, then the treating physician should consider the possibility of surgical management (Fig. 10.4A,B). MR imaging is useful to document discoligamentous injury. Fig. 10.3 (A,B) CT sagittal reformats. (A) Measurement of height of facet fracture. (B) Height of intact lateral mass. In this study, no patient with facet fracture height to intact lateral mass height ratio < 40% or absolute facet fracture height > 1 cm failed nonoperative management. (From Spector LR, Kim DH, Affonso J, Albert TJ, Hilibrand AS, Vaccaro AR. Use of computed tomography to predict failure of nonoperative treatment of unilateral facet fractures of the cervical spine. Spine 2006;31:2827–2835. Reprinted with permission.)
Facet Fractures
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
Special Diagnostic Tests
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







