and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
In most total knee arthroplasties (TKAs) for arthritic knees with intra-articular varus or valgus deformity, both alignment and ligament balance can be achieved with appropriate bone cuts and soft-tissue releases. However, TKA becomes technically challenging when knee arthritis is associated with an extra-articular deformity (EAD) of either the femur or the tibia. Such deformities are commonly caused secondary to trauma (malunion or non-union), previous osteotomy, metabolic causes such as osteomalacia or osteoporosis causing excessive bowing or stress fractures and congenital causes (Fig. 8.1). Stress fracture although uncommon is a frequent cause of tibial EAD in patients with knee arthritis.
Introduction
In most total knee arthroplasties (TKAs) for arthritic knees with intra-articular varus or valgus deformity, both alignment and ligament balance can be achieved with appropriate bone cuts and soft-tissue releases. However, TKA becomes technically challenging when knee arthritis is associated with an extra-articular deformity (EAD) of either the femur or the tibia. Such deformities are secondary to trauma (malunion or non-union), previous osteotomy, metabolic causes such as osteomalacia or osteoporosis causing excessive bowing or stress fractures and congenital causes (Fig. 8.1) [1–4]. Stress fracture although uncommon is a frequent cause of tibial EAD in patients with knee arthritis.




Fig. 8.1
Causes of extra-articular deformities in knees undergoing TKA. (a) Post-traumatic deformity in the distal ½ of the tibial shaft with broken nail in situ. (b) Post-traumatic deformity in the distal 1/3 of femur due to a malunited fracture with implant in the proximal ½ of femur. (c) Severe extra-articular deformity in the proximal end of the tibia secondary to high tibial osteotomy (HTO) with implant in situ. (d) Severe bowing of the femoral shaft probably secondary to osteopenia and/or osteomalacia compounding the knee deformity. (e) Stress fracture in the upper 1/3 of the tibial shaft causing varus deformity locally. (f) Proximal tibia varus. (g) Bowing of the proximal ½ of the femoral shaft secondary to probably a congenital cause
Options for dealing with such EADs during TKA include intra-articular correction along with bone resection and extensive soft-tissue release and staged or simultaneous corrective osteotomy at the apex of the EAD along with intra-articular correction. Conventional techniques, although effective in majority of such cases, may not be appropriate in selected limbs where the presence of hardware or excessive distortion of the femoral canal due to deformity may make the use of an intramedullary femoral guide difficult (Fig. 8.2) [4]. Recent reports describing the use of navigated TKA for knee arthritis with EADs have indicated good results with appropriate bone cuts and soft tissue releases [1, 5–8]. Navigation systems use the centre of the femoral head, the centre of the knee joint and the centre of the ankle to calculate the mechanical axis; help in avoiding excess bone resection; allow graduated measured soft-tissue release; and align the femoral component based on the mechanical axis derived from the femoral head centre and knee centre, bypassing the femoral extra-articular deformity. Hence, femoral EAD with distortion of the femoral canal and the presence of hardware especially in the distal half of the femur may be an appropriate indication for computer-assisted surgery in this subgroup of patients undergoing TKA. This chapter aims to outline the means of dealing with EADs during TKA.
Fig. 8.2
Excessive distortion of the femoral canal due to extra-articular deformity or presence of hardware makes the use of an intramedullary femoral guide challenging during conventional TKA. (a) Extra-articular deformity at the distal 1/3 of the femur due to a malunited fracture caused an extension deformity of the distal fragment. Use of an intramedullary femur guide rod (black line) will cause it to go posteriorly within the distorted canal. (b) Extra-articular deformity at the distal 1/3 of the femur due to a malunited fracture caused a varus deformity of the distal fragment. Use of an intramedullary femur guide rod (black line) will cause it to go laterally within the distorted canal. (c) An intramedullary nail previously used to fix a distal femur shaft fracture. This nail will have to be removed if an intramedullary femur guide rod needs to be used during conventional TKA
Pathoanatomy
Extra-articular deformities in knees which undergo TKA complicate the procedure in a number of ways. First, an EAD either in the tibia or the femur adds to the overall deformity in a limb already deformed due to knee arthritis (Fig. 8.3). Hence, realignment in such limbs will require extensive soft-tissue release and achieving medio-lateral balance will be challenging especially if there is a dearth of osteophytes and excessive lateral laxity (in a varus knee, or vice versa) at the knee. Such limbs are therefore cases which may require additional procedures such as lateral epicondylar or sliding medial condylar osteotomy to achieve optimum limb alignment and soft-tissue balance [9, 10]. Second, some of these limbs with associated EAD especially secondary to a previous surgical procedure (high tibial osteotomy or fracture fixation) have hardware in situ which makes use of conventional intramedullary alignment jigs challenging and may require hardware removal before the start of TKA (Fig. 8.2). Third, an EAD close to the knee joint may distort local bony anatomy and make optimum component alignment challenging to achieve. Finally, severe EADs, especially in the proximal tibia or distal femur, may require an additional corrective osteotomy performed either simultaneously with TKA or in a staged manner [1].
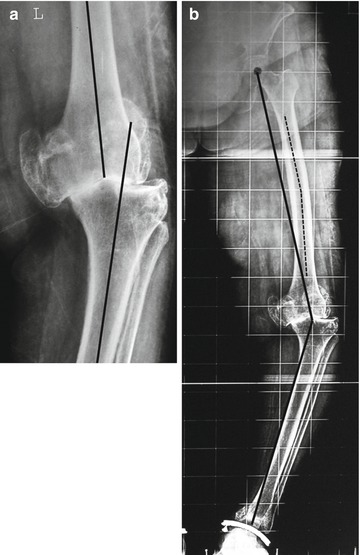
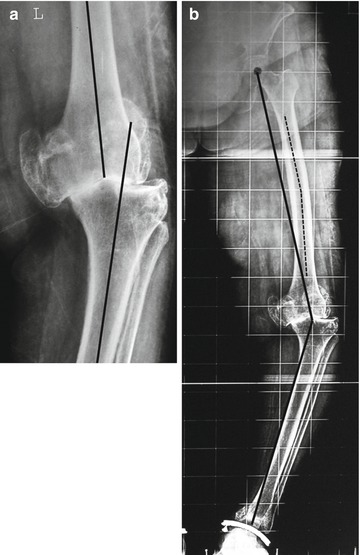
Fig. 8.3
A common cause of femoral extra-articular deformity in patients undergoing TKA – excessive coronal bowing of the femoral shaft. This adds to the overall deformity of the limb. (a) Standing knee anteroposterior radiograph showing a knee deformity of 15° varus (black line). (b) Standing, full-length hip-to-ankle radiograph of the same patient shows that the overall limb deformity (hip-knee-ankle angle) is actually 30° varus. Excessive coronal bowing of the femoral shaft (dotted line) at 12° in this case adds to the overall deformity of the limb which can be easily missed if only short knee films are used
The most common EAD encountered during TKA is excessive coronal bowing of the femoral shaft [1] (Fig. 8.3). A study published by the senior author reports the incidence of excessive coronal bowing of the femoral shaft at 15 % in arthritic knees which undergo TKA in Indian study population [11]. Similar findings have been reported in other study populations especially in Asians. Another common cause of EAD in the femur is a malunited fracture typically with hardware in situ. Similarly, in the tibia, the common causes of EAD include proximal tibia vara due to distortion and bony adaptation secondary to knee arthritis and/or metabolic causes, malunited fractures, stress fractures secondary to metabolic causes and deformity secondary to a previous high tibial osteotomy (HTO). As per the classification proposed by the authors (Table 8.1), tibial stress fractures in arthritic knees are primarily intra-articular or extra-articular type (Fig. 8.4) [2]. Based on the type of stress fractures, the surgical technique and implant used may vary during TKA.

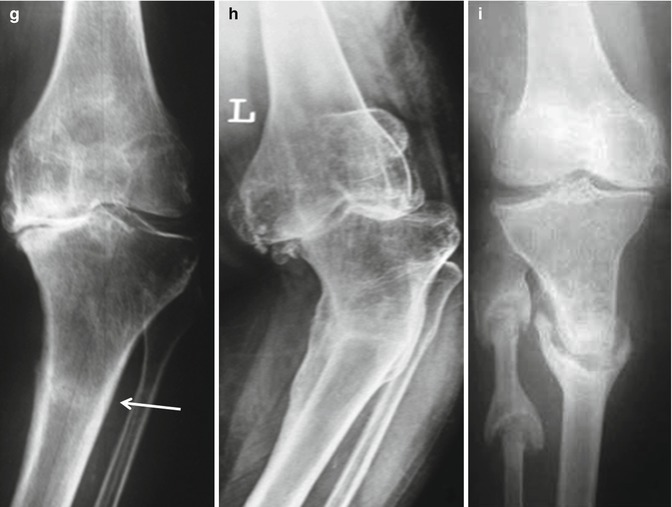
Table 8.1
Classification of tibial stress fractures in patients undergoing TKA
I. Intra-articular |
(A) Malunited |
(B) Ununited |
II. Extra-articular |
(A) Impending |
(B) Acute |
(C) United |
(D) Malunited |
(E) Ununited |

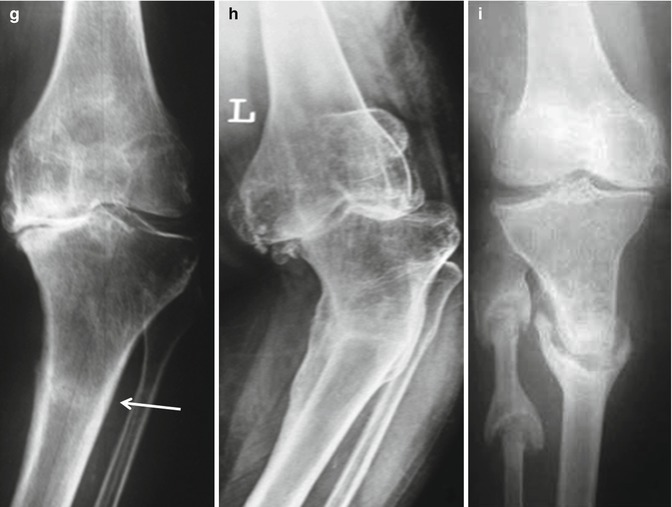
Fig. 8.4
Types of tibial stress fractures seen in knees undergoing TKA. (a) Type IA – Malunited intra-articular fracture (arrow). (b) Type IB – Ununited intra-articular fracture (arrow). (c) MRI of the same patient in (b) shows the extent of fracture and medial tibial bone defect (black arrow) caused by it. (d) Type IIA – Impending extra-articular fracture which is not obvious on plain knee radiograph. The patient had local tenderness on the anterior aspect of proximal 1/3 of the tibial shaft on clinical examination. (e) MRI of the same patient in (d) shows the stress fracture on proximal 1/3 of the tibial shaft (black arrow). Impending stress fractures can be diagnosed clinically and need an MRI for confirmation. (f) Type IIB – Acute extra-articular fracture of the proximal 1/3 of the tibial shaft (arrow). (g) Type IIC – United extra-articular fracture of the proximal 1/3 of the tibial shaft (arrow) which has healed without any local residual deformity. (h) Type IID – Malunited extra-articular fracture of the proximal 1/3 of the tibial shaft causing severe varus extra-articular deformity of approximately 37° at the fracture site. (i) Type IIE – Ununited extra-articular fracture of the proximal 1/3 of the tibial shaft
Post-HTO is a special category of tibial EAD which brings its own challenges while performing TKA. The issues which need to be dealt with during a post-HTO TKA include a previous skin incision, periarticular bony distortion, soft-tissue changes, implant in situ and patellar changes such as maltracking and patella infera (Table 8.2). Periarticular bony distortion secondary to a previous HTO include medial tibial bone loss and lateral femoral condylar deficiency, excessive medial or lateral and/or posterior or anterior sloping of tibial plateau, excessive medial or lateral and/or anterior or posterior translation of the proximal tibia and internal or external torsion of the proximal tibia (Fig. 8.5) [12, 13].

Table 8.2
Changes in the knee frequently encountered during post-high tibial osteotomy TKAs which can pose a challenge for the surgeon
Previous vertical skin incisions |
Patella maltracking, fibrosis around patellar tendon insertion, patella infera |
Implant in situ |
Tibial bone loss |
Decreased or increased tibial slope |
Medial or lateral translation of proximal tibia |
Anterior or posterior translation of the proximal tibia |
Internal or external torsion of the proximal tibia |
Medio-lateral soft-tissue imbalance |
Excessive posterior soft-tissue laxity |
Extra-articular deformity |

Fig. 8.5
Knee radiograph showing periarticular bony distortion secondary to a previous high tibial osteotomy (HTO). (a) Plain knee radiograph showing medial tibial bone loss (dotted arrow), lateral femoral condylar deficiency (dotted arrow) and bony overgrowth of the lateral tibia (solid arrow). (b) Posterior translation of the proximal end of the tibia (arrow). (c) Coronal angulation of the tibial plateau with implant in situ. (d) Severe extra-articular varus deformity of the proximal tibia with implant in situ. There is associated excessive lateral side soft-tissue laxity seen here as excessive opening of the lateral joint space (curved arrow). (e) Reverse sloping of the tibial plateau (dotted line)
Preoperative Planning
A full-length hip-to-ankle radiograph is necessary to plan for TKA in cases with femoral or tibial EAD. A thorough evaluation of soft-tissue balance under anaesthesia is also invaluable especially in knees which have been previously operated.
Femoral Extra-Articular Deformities
On preoperative standing, full-length hip-to-ankle radiographs, the proposed distal femoral cut is drawn perpendicular to the mechanical axis of the femur. If the EAD is close to the joint or is more than 20° in the coronal plane or if the plane of the distal cut is likely to compromise the attachment of the lateral collateral ligament on the lateral epicondyle, a corrective osteotomy is considered (Fig. 8.6) [1, 3]. In the presence of significant femoral bowing (as evidenced by an increase in the angle between the mechanical axis and the distal femoral anatomic axis), the distal femoral valgus resection angle should be measured preoperatively and proportionately increased during the procedure (Fig. 8.7) [14]. Severe femoral bowing with minimal osteophytes and severe lateral laxity with or without rigid medial soft-tissue contracture in varus arthritic knees should alert the surgeon that balancing and realignment may be difficult using only intra-articular correction and a sliding osteotomy of the medial condyle may be required (Fig. 8.8) [10].

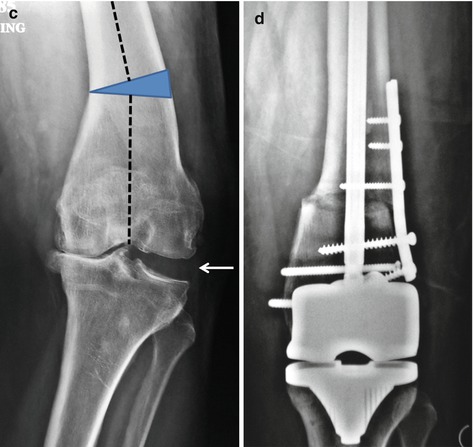

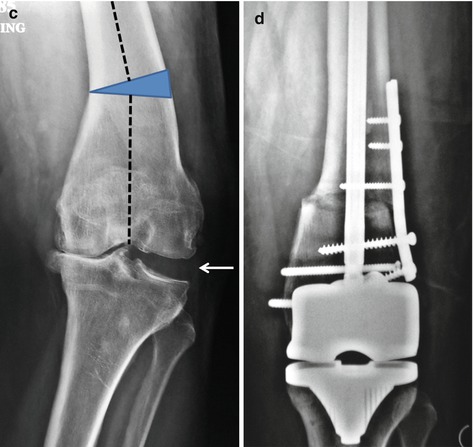
Fig. 8.6




Preoperative planning in a patient with a femoral extra-articular undergoing TKA. (a) Preoperative full-length anteroposterior radiograph of the femur showing extra-articular deformity of 15° secondary to malunited fracture of the femoral midshaft. Note that the proposed distal femoral cut (dashed line) drawn perpendicular to the mechanical axis of the femur will not compromise the attachment of the lateral collateral ligament (LCL) on the lateral epicondyle (asterisk) and a corrective osteotomy is not required here. (b) Preoperative standing, full-length hip-to-ankle radiograph of a patient with extra-articular deformity in the distal 1/3 femur due to malunited fracture. The limb deformity (hip-knee-ankle angle) in this patient was 22.5°, and the deformity in the distal 1/3 femur due to malunited fracture (white dashed line) was 12.5°. However, the proposed distal femoral cut (black dashed line) when drawn perpendicular to the mechanical axis of the femur showed that it would have compromised the attachment of the LCL on the lateral epicondyle (asterisk). (c) Standing knee radiograph of the same patient (b) showing excessive lateral side soft-tissue laxity seen here as excessive opening of the lateral joint space (arrow) and deficiency of osteophytes. Considering the severity and proximity of the extra-articular deformity (dashed line) to the knee joint, possibility of compromise of LCL with the distal femoral cut, significant lateral soft-tissue laxity and the deficiency of osteophytes, a lateral closing wedge corrective osteotomy at the distal femur will be required in this patient to restore limb alignment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








