and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
With rapid advancement in technology and materials in total knee arthroplasty (TKA), long-term survival and function of the total knee are increasingly more dependent on optimum surgical technique. Adherence to basic surgical principles ensures a successful outcome. Surgical technique in TKA is akin to a game of chess where every move has predictable and logical consequences. Hence, every step of the surgical technique needs to be well thought of before execution. The aim of the authors, like most surgeons, is to ensure a well-aligned, well-balanced and well-fixed TKA. Ligament balancing is an integral part of TKA, and soft-tissue release should follow a functional and anatomic rationale to achieve correct alignment and ligament balance throughout the range of flexion and extension. Any deviation from this principle may lead to stiffness, imbalance or instability during TKA.
Introduction
With rapid advancement in technology and materials in total knee arthroplasty (TKA), long-term survival and function of the total knee are increasingly more dependent on optimum surgical technique [1–3]. Adherence to basic surgical principles ensures a successful outcome. Surgical technique in TKA is akin to a game of chess where every move has predictable and logical consequences. Hence, every step of the surgical technique needs to be well thought of before execution. The aim of the authors, like most surgeons, is to ensure a well-aligned, well-balanced and well-fixed TKA. Ligament balancing is an integral part of TKA, and soft-tissue release should follow a functional and anatomic rationale to achieve correct alignment and ligament balance throughout the range of flexion and extension. Any deviation from this principle may lead to stiffness, imbalance or instability during TKA.
The two basic techniques commonly used in TKA are the measured resection technique and the gap-balancing technique. The authors have successfully used the gap-balancing technique in all their cases. This technique has proved reliable to achieve a well-aligned and well-balanced knee across various types and severity of knee deformity. The present chapter aims to outline the basic principles of TKA being followed by the authors. The chapter begins with a brief “disclaimer” listing the characteristic features of surgical technique being followed by the authors.
“Disclaimer”
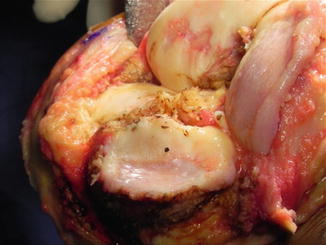
Only posterior cruciate-substituting (CS) TKAs have been used by the authors. The rationale of using only CS knees is based on the finding that the posterior cruciate ligament may undergo marked structural and functional deterioration in arthritic knees especially in severe grades of arthritis [4–7] and that the functional outcome and kinematics may be more predictable with a CS knee [8–10].
Tibial preparation is performed as the first step in the majority of the knees.
The gap-balancing technique has been used in all knees. Ligament balancing and gap balancing are done with balancing in extension first followed by femoral sizing and creating a flexion gap equal to the extension gap.
Ligament balancing is predictable and can be ensured throughout the full knee range of motion in most knees. The authors mainly check ligament balance in full extension and at 90° flexion (and can also now quantify it throughout knee range of motion using navigation). However, balancing around deep knee flexion is still an area of controversy and is unclear [11].
Only cemented components have been used in all knees, and all knees undergo patellar resurfacing.
Standard approach with medial parapatellar arthrotomy has been used in all knees.
Computer navigation described here is not only utilised to ensure accurate limb and component alignment but also to quantify ligament balancing and the amount of bone resection and soft-tissue release performed. Hence, navigation has been used by the authors more as a tool for verification where the computer navigation system provides real-time feedback of various surgical steps.
Ligament Balancing: The “Kaizen” Approach
Kaizen, Japanese for “improvement”, or “change for the better”, refers to philosophy or practices that focus upon continuous improvement of processes and techniques [12]. In simple language, this concept implies performing several small, continuous steps of improvement to achieve significant results [12]. The principles of ligament balancing we use during TKA are very similar to the Kaizen concept. Optimum limb alignment and soft-tissue balancing are achieved during TKA by executing several small, interrelated steps involving bone cuts and soft-tissue release and varying the size and position of the femoral component.
Basically, soft-tissue balancing in TKA involves achieving “equality and equipoise” (i.e. equal width and equal tension) between the medial and the lateral compartments within the extension or flexion gap and between the extension and flexion gaps. Hence, the two aims are to achieve a rectangular extension and flexion gap and a flexion gap equal in width to the extension gap. Soft-tissue releases to achieve balance in TKA involve deciding what to release, when to release and how much to release for a given knee deformity. It is crucial to keep in mind that intra-articular soft-tissue release and bone cuts are intended to deal with intra-articular deformities. Attempts to tackle an associated extra-articular deformity of the femur or tibia using this technique may involve significant release of important soft-tissue stabilizers of the knee joint like the collaterals which may subsequently result in imbalance. Hence, cases with a concomitant extra-articular deformity may require an additional procedure like corrective or epicondylar osteotomy [13].
How to Assess Soft-Tissue Tension?
Numerous devices have been described to assess soft-tissue tension during TKA. We use a tensioner made up of a single fixed tibial plate which sits on the tibial cut surface and two separate moveable plates for the medial and the lateral femoral condyles (Fig. 2.1a). These two femoral plates can be moved independently using a screw mechanism to increase or decrease the tension medially and laterally. In full extension, the aim while assessing ligament tension is to achieve a limb alignment as close to neutral as possible and equal tension both medially and laterally as assessed by the surgeon (Fig. 2.1b). The final stability is checked in full extension using spacer blocks where a valgus and a varus stress are applied to determine the degree of laxity (Fig. 2.1c). This step is again repeated in 90° flexion using the tensioning device and also using a spacer block with the AP cutting block in place (Fig. 2.1d, e). The aim is not only to ensure that there is optimum stability in full extension and 90° flexion but also to confirm that any opening on stressing is equal on both sides and which also springs back equally.
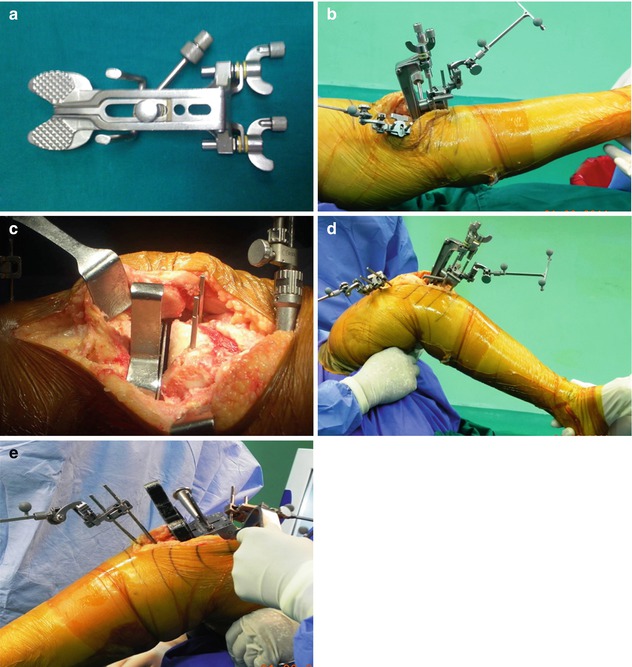
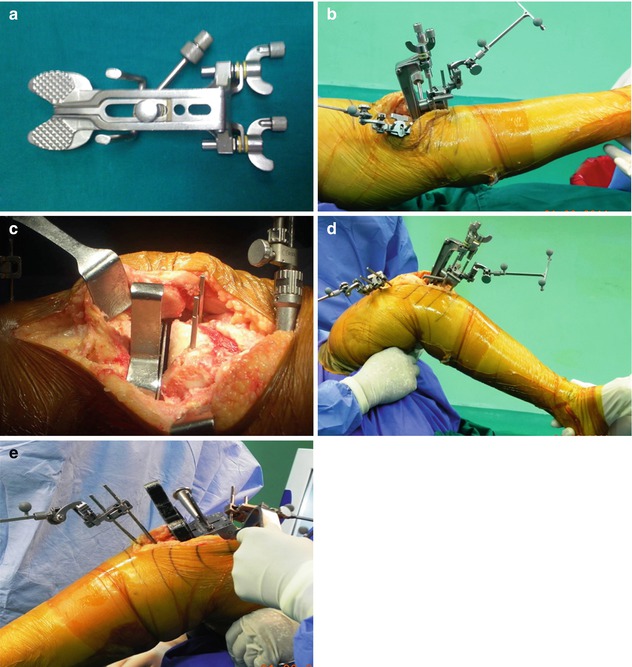
Fig. 2.1
Various steps for assessing soft-tissue tension during TKA. (a) Soft-tissue tensioner used by the authors during TKA. It is made up of a single fixed tibial plate which sits on the tibial cut surface and two separate moveable plates for the medial and the lateral femoral condyles. (b) Assessment of medial and lateral soft-tissue tension using the tensioner with the limb held in neutral alignment and the knee held in full extension. (c) Assessment of medial and lateral soft-tissue tension using a spacer block with the knee held in full extension. (d) Assessment of medial and lateral soft-tissue tension using the tensioner with the knee held in 90° flexion. Note that the thigh is supported by an assistant to nullify the effect of the weight of the limb during the assessment. (e) Assessment of medial and lateral soft-tissue tension using a spacer block with the knee held in 90° flexion. This is done before the posterior cut is performed with the femoral AP block pinned in place
What to Release?
Based on the type of knee deformity and the degree of initial soft-tissue imbalance, the site and the structures to be released vary from knee to knee. A thorough knowledge of what structures can be released during TKA for any given deformity is essential. For a varus knee, no release on the lateral side should be performed, and for a valgus knee the opposite is true. Similarly, for a knee with flexion deformity, posterior release is necessary, whereas in a hyperextending knee it should be strictly avoided. We completely avoid performing any sort of release of the collaterals and avoid completely releasing the pes anserinus or dividing the popliteus tendon. Most deformities and imbalance can be corrected releasing capsular structures and adhesions rather than the collaterals and supplementing these releases with osteotomies. It must be pointed out that the collateral ligaments themselves do not undergo contracture/shortening.
When and How Much to Release?
We follow a graduated, controlled and stepwise approach to soft-tissue release during TKA. Removal of osteophytes as the initial step considerably improves deformity and decreases the quantum of soft-tissue release required. A preliminary soft-tissue release is performed as part of exposure and following osteophyte excision. Rigid deformities may not be fully corrected with a preliminary release. Similarly, although soft-tissue release may achieve full correction of deformity, it may fail to achieve medio-lateral balance. Such cases with residual deformity or medio-lateral imbalance will require further, extended releases supplemented by a reduction osteotomy [14].
Equalising Medial and Lateral Gap in Extension
With the knee in full extension, the tibial and the distal femoral resection are made perpendicular to their respective mechanical axes (Fig. 2.2a). The aim is to create a rectangular extension gap equal on both medial and lateral side. However, despite accurate bone cuts, the extension gap may be unequal or quadrilateral owing to medio-lateral soft-tissue imbalance as determined by spacer blocks (Fig. 2.2b). This disparity needs to be rectified using appropriate soft-tissue releases to restore limb alignment and medio-lateral balance (Fig. 2.2c). The extent of medio-lateral soft-tissue disparity in extension after the bone cuts can be predicted using the joint divergence angle on preoperative full-length radiographs (see Chap. 1).
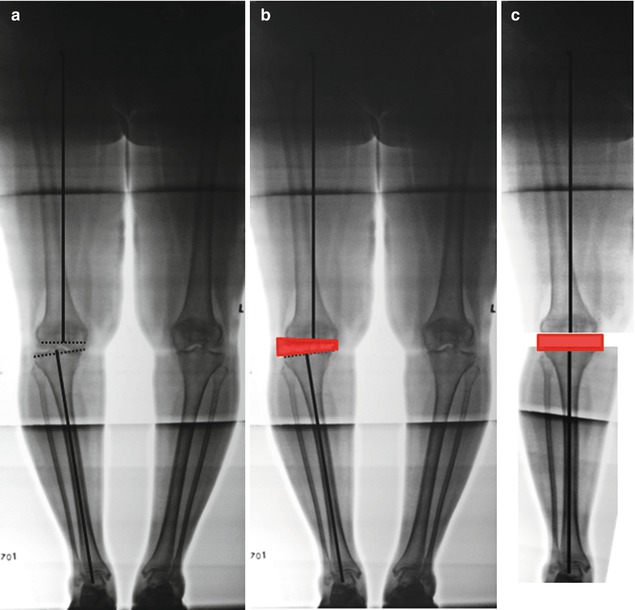
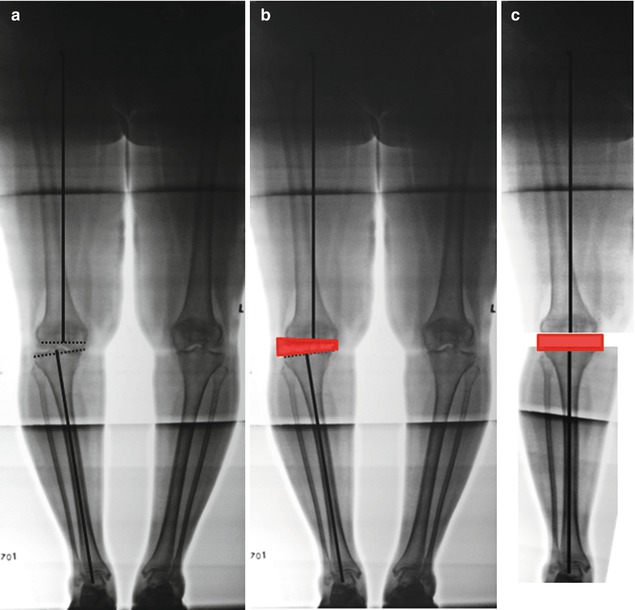
Fig. 2.2
Equalising medial and lateral gaps in full extension. (a) The tibial and the distal femoral resections (dotted lines) are made perpendicular to their respective mechanical axes (solid lines). (b) Despite accurate cuts, the resultant extension gap may be quadrilateral instead of rectangular due to medio-lateral soft-tissue imbalance as determined by a spacer block. (c) This requires appropriate soft-tissue releases to restore limb alignment and medio-lateral balance and a rectangular extension gap
Equalising Medial and Lateral Gap in 90° Flexion
With the knee in 90° flexion, the tibial and posterior femoral cuts should generally be parallel to the epicondylar axis and perpendicular to the anteroposterior axis of the femur (Fig. 2.3a). We mark the level of the tentative posterior femoral cut after assessing flexion gap balance using the tensioner (Fig. 2.3b, c). However, it is very important to achieve good medio-lateral balance in flexion before determining the level and performing the posterior femoral cut. In varus knees, if the posterior femur is cut in the presence of excessive medial tightness, then the femoral component may get placed in excessive external rotation and vice versa (Fig. 2.3d–e). Similar to when the knee is in full extension, the aim at 90° knee flexion is to create a rectangular flexion gap equal on both medial and lateral side. Hence, the determinants of flexion gap include distal femoral and tibial cuts, medio-lateral soft-tissue tension in 90° flexion, femoral component size and position and the tibial insert thickness.
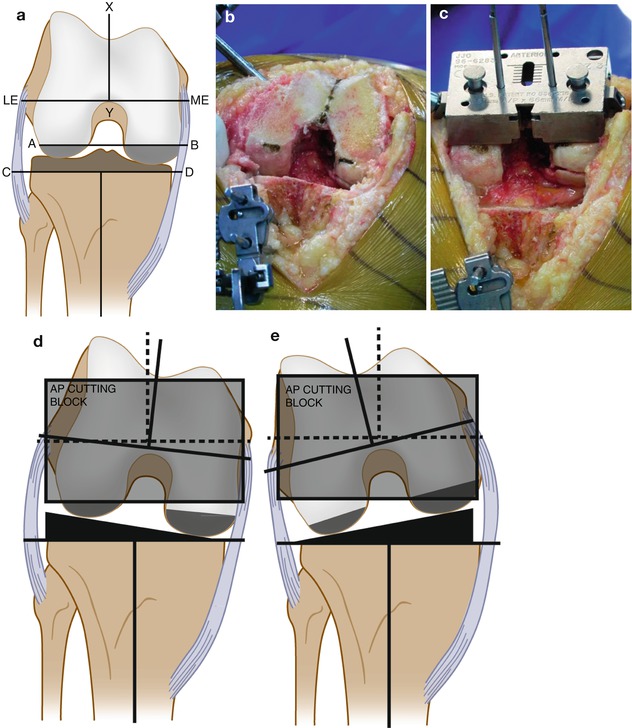
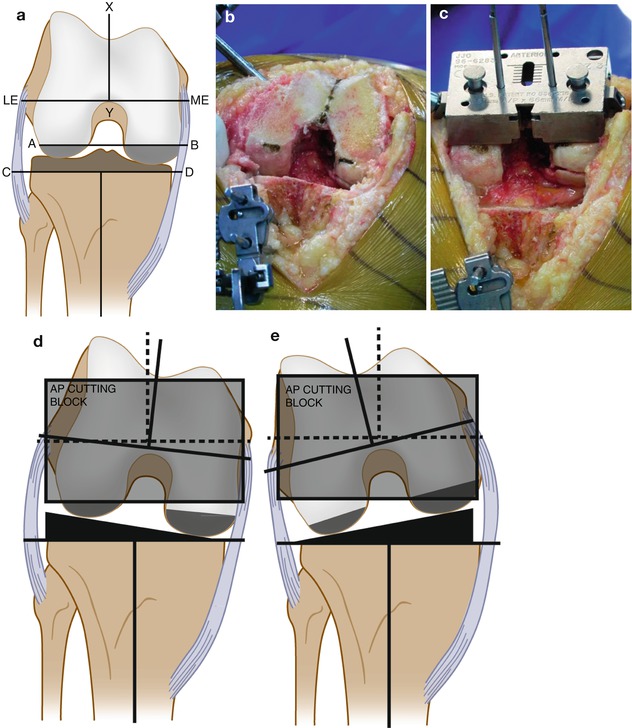
Fig. 2.3
Equalising medial and lateral gaps in 90° flexion. (a) Relation of various distal femoral rotational axes to the posterior femoral (line AB) and tibial (line CD) cuts with the knee in 90° flexion. The tibial and posterior femur cuts should generally be parallel to the epicondylar axis (line LE–ME) and perpendicular to the anteroposterior (AP) axis of the femur (line XY). (b) The tentative posterior femoral cut marked after assessing flexion gap balance using the tensioner and its relation to the AP axis. (c) The AP cutting block pinned in position and its relation to the previously marked distal cut. Note that the cutting block has been positioned based on “combined referencing”. (d) If the AP cutting block is placed and the posterior femur is cut in the presence of excessive medial tightness, then the femoral component may get placed in excessive external rotation. (e) Similarly, if the AP cutting block is placed and the posterior femur is cut in the presence of excessive lateral tightness, then the femoral component may get placed in excessive internal rotation
Equalising Flexion Gap to the Extension Gap
Based on our technique of creating the extension gap first, the way to flexion-extension gap balancing involves creating a flexion gap matching in dimension to the previously created extension gap. The key to achieving this is the size and position of the femoral component. Using the method previously described, the flexion gap is assessed using a spacer block with the AP cutting block of the estimated femoral component size pinned in place. This must have no slots posteriorly. Using a stylus or “angel wing”, we ensure that there is no notching. If the flexion gap is tighter for the corresponding spacer block used previously in the assessment of extension gap, the femoral component needs to be undersized or moved anteriorly in order to equalise the flexion-extension gaps. Slight flexion or posterior shift of the femoral component may also be helpful to tackle a flexion gap that exceeds the extension gap. However, the surgeon needs to be cautious in not overdoing this and causing either anterior notching or post impingement against the box in extension. The AP block is placed accurately before performing the anterior and posterior femoral cuts by using “combined referencing” where multiple references are used to ascertain the position of the AP cutting block and subsequently the femoral component (Fig. 2.4).
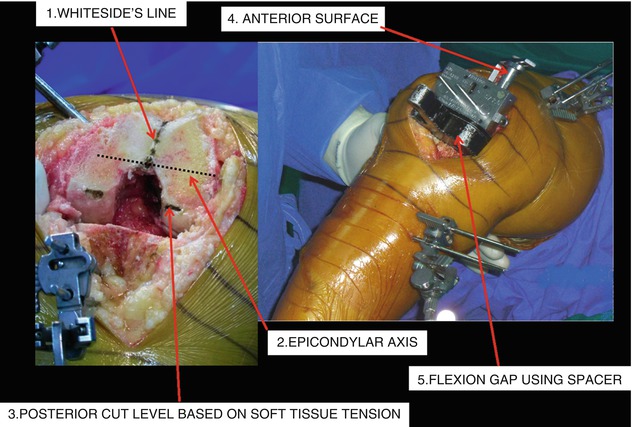
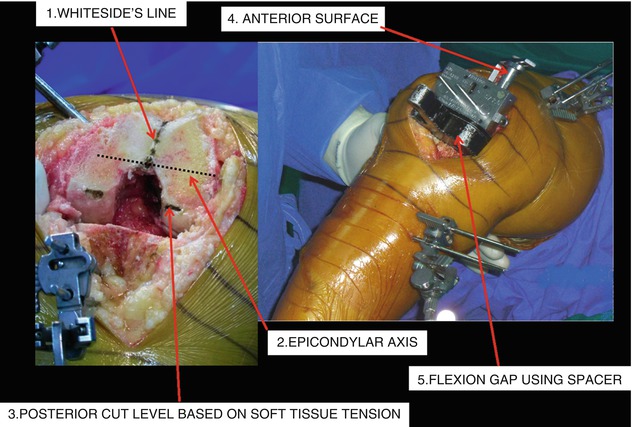
Fig. 2.4
The concept of “combined referencing” and its five components in order to accurately place the AP cutting block
Surgical Approach and Exposure
The authors use the classical anterior skin incision with the medial parapatellar arthrotomy to approach the knee. This approach has served us well in almost all of our TKA cases. Rare exceptions where an alternative approach was used include knees with severe valgus arthritis and patellar maltracking which required a lateral parapatellar arthrotomy and stiff arthritic knees where a tibial tubercle osteotomy was performed to improve exposure.
We use a pneumatic tourniquet in all our cases which is inflated before the incision is taken. The pressure set is typically 100 mmHg over the systolic pressure of the patient in thin or nonobese patients or 150 mmHg over and above if the patient is obese. Rarely, if the patient is morbidly obese and the thigh size is too big for the largest cuff, tourniquet is applied but inflated after all the bone cuts have been performed and just before cementing.
The tibial cut is always performed first in all our cases. Using seven simple steps during exposure will help in easily dislocating the knee and bringing the tibia forwards without having to perform excessive, unnecessary soft-tissue release or having to apply a Hohmann’s retractor on the posterior aspect of the tibia. This approach allows for laterally displacing the extensor apparatus (quadriceps tendon and patella) easily without having to evert the patella and adequately exposing the tibial articular surface to perform the tibial cut (Fig. 2.5). Like any surgical procedure, approaching the knee to perform TKA is facilitated by using the right surgical instruments. After the medial parapatellar arthrotomy, the following seven steps are performed to adequately expose the knee for TKA: