and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
A valgus arthritic knee, compared to a varus knee, offers its own challenges during total knee arthroplasty (TKA). A valgus knee is less commonly encountered in arthritic knees undergoing TKA and involves a distinctly different set of pathoanatomic structural changes when compared to a varus knee. The incidence of valgus arthritic knees in patients undergoing TKA is less than 10 % in the senior surgeon’s series [1, 2]. Restoration of optimal limb alignment and gap balance after TKA in valgus knees can be a formidable challenge because of several reasons. First, a surgeon may be less familiar with the surgical technique and soft-tissue releases involved and there is a paucity of soft-tissue structures available for release on the lateral side compared to the medial side. Second, there is a higher risk of common peroneal nerve palsy due to its proximity to lateral soft-tissue structures and stretching that may occur in correcting long-standing valgus deformity especially if associated with flexion deformity.
Introduction
A valgus arthritic knee, compared to a varus knee, offers its own challenges during total knee arthroplasty (TKA). A valgus knee is less commonly encountered in arthritic knees undergoing TKA and involves a distinctly different set of pathoanatomic structural changes when compared to a varus knee. The incidence of valgus arthritic knees in patients undergoing TKA is less than 10 % in the senior surgeon’s series [1, 2]. Restoration of optimal limb alignment and gap balance after TKA in valgus knees can be a formidable challenge because of several reasons. First, a surgeon may be less familiar with the surgical technique and soft-tissue releases involved and there is a paucity of soft-tissue structures available for release on the lateral side compared to the medial side. Second, there is a higher risk of common peroneal nerve palsy due to its proximity to lateral soft-tissue structures and stretching that may occur in correcting long-standing valgus deformity especially if associated with flexion deformity. Finally, osseous defects in the posterolateral aspect of the femur and tibia; hypoplastic lateral femoral condyle, an associated external rotation deformity of the distal femur or proximal tibia, and patellar maltracking may also be commonly encountered in valgus arthritic knees. Hence, a valgus knee is a different ball game when compared to varus arthritic knees, and this chapter aims to outline the management of the same with TKA.
Pathoanatomy
Valgus arthritic deformities commonly present with tightness of lateral soft-tissue structures which may be associated with varying degrees of laxity of the medial structures. Contracture of the iliotibial (IT) band, popliteus tendon, posterolateral capsule and popliteofibular ligament may be encountered in these knees (Fig. 4.1). We do not believe that the lateral collateral ligament (LCL) undergoes contracture and shortening. The surgeon should be aware which soft-tissue structures are taut in different positions of knee flexion and extension so that a calibrated, stepwise approach is followed during release and imbalance or instability avoided. Essentially, the LCL and popliteus tendon are taut in both flexion and extension, the IT band and posterolateral capsule are taut only in extension, and the popliteofibular ligament is taut only in flexion [3].
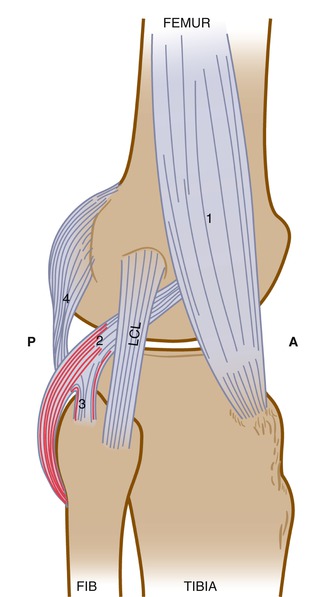
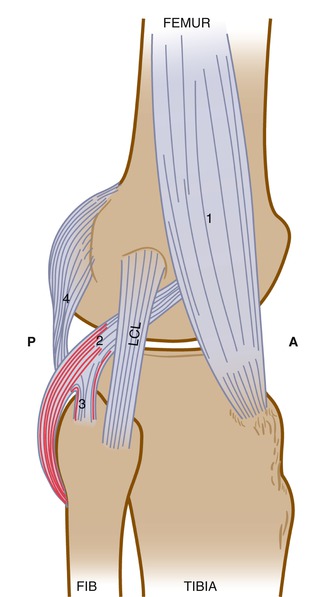
Fig. 4.1
Soft-tissue structures on the lateral and posterolateral aspect of the knee joint which may require release during TKA in a valgus arthritic knee. 1 Iliotibial band, 2 popliteus tendon, 3 popliteofibular ligament, 4 posterolateral capsule. A anterior, P posterior, LCL lateral collateral ligament
In addition, there may be asymmetric wear or hypoplasia of the posterior condyles with excessive wear of the posterolateral condyle of the femur and/or tibia (Fig. 4.2a, b) [4]. This is important to note intraoperatively as using the posterior femoral condyles as a reference to place the AP cutting block may cause excessive resection from the posterior femoral condyle laterally, thereby resulting in excessive internal rotation of the femoral component and patellar maltracking. Using the AP axis (as described by Arima and Whiteside [5]) as an alternative to achieving proper femoral component rotation is also fraught with risk especially if the patella is maltracking and leads to more lateral wear of the trochlear groove (Fig. 4.2c). Hence, the transepicondylar axis (TEA) is preferred by the authors in severe valgus deformities as a landmark for determining femoral rotation. Patellar maltracking, commonly seen in severe valgus deformities (Fig. 4.2a), is usually the consequence of an excessive Q angle due to valgus malalignment, excessive external tibial torsion and excessive tightness of the lateral retinaculum [6]. Valgus knees may also be associated with external rotation deformity of the proximal tibia due to a tight iliotibial tract [6]. Lastly, the valgus arthritic knee just like the varus knee may also be associated with a sagittal plane deformity such as flexion or hyperextension deformity or an extra-articular deformity which may further complicate the surgical technique. Most patients with a valgus deformity at the knee have associated hindfoot valgus (flatfeet) (Fig. 4.3) and even distortion of the midfoot [7, 8]. The authors have reported that despite restoring the hip-knee-ankle (HKA) axis in such patients, the ground mechanical axis may still pass lateral to the centre of the knee joint, and this may need to be factored in while deciding what should be the final knee alignment during TKA [7].
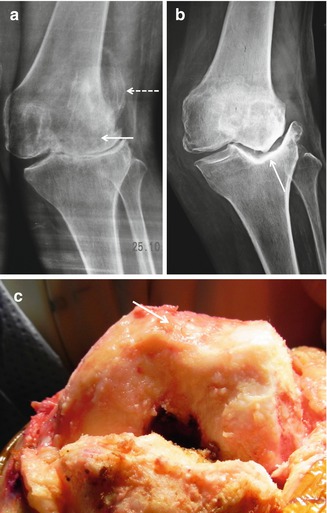

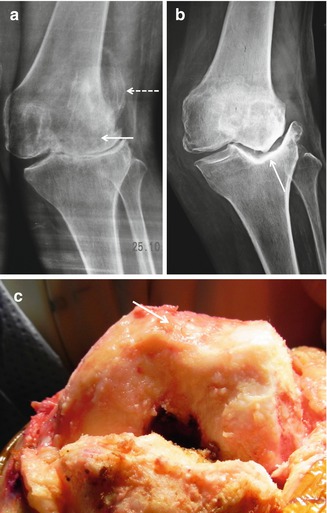
Fig. 4.2
Common pathoanatomic findings in a valgus arthritic knee. (a) Hypoplasia and distortion of the lateral femoral condyle (solid arrow) with associated patellar maltracking (dashed arrow) as seen on an anteroposterior standing knee radiograph. (b) Significant bone loss from the lateral tibial condyle (arrow) as seen on an anteroposterior standing knee radiograph. Note the large osteophyte on the lateral margin of the tibial plateau which must be excised before any soft-tissue release. (c) Intraoperative finding showing significant erosion and distortion of the femoral trochlear groove (arrow) due to severe patellofemoral arthritis and significant patellar maltracking. Using the anteroposterior axis as reference to determine femoral rotation in this case is risky

Fig. 4.3
Bilateral valgus knees associated with significant hindfoot valgus
Valgus knees form a spectrum of deformities with important differences which impact surgical technique. All valgus knees are not alike! Ranawat et al. [9] had classified valgus arthritic knees into three major variants based on the degree of deformity, status of medial collateral ligament (MCL) and the amount of lateral release required – variant 1 showing minimal valgus deformity and medial soft-tissue stretching; variant 2 showing substantial deformity (>10°), bone loss and medial stretching; and variant 3 showing severe deformity and osseous deficiency with an incompetent medial soft-tissue sleeve. The authors have modified this classification to include six types of valgus knees based on (1) severity and correctibility of valgus deformity, (2) associated flexion, hyperextension or extra-articular deformity and (3) status of the medial collateral ligament (MCL) (Table. 4.1, Figs. 4.4, 4.5, 4.6, 4.7, 4.8 and 4.9).
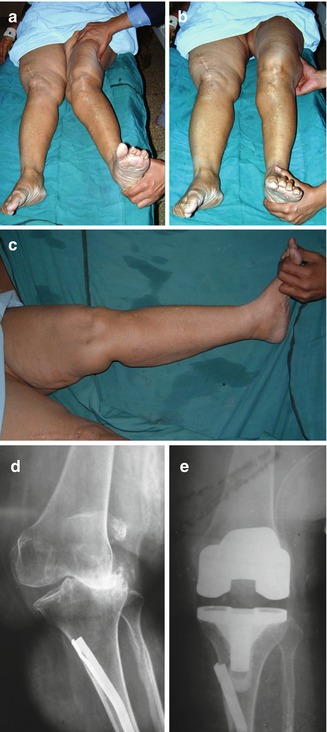
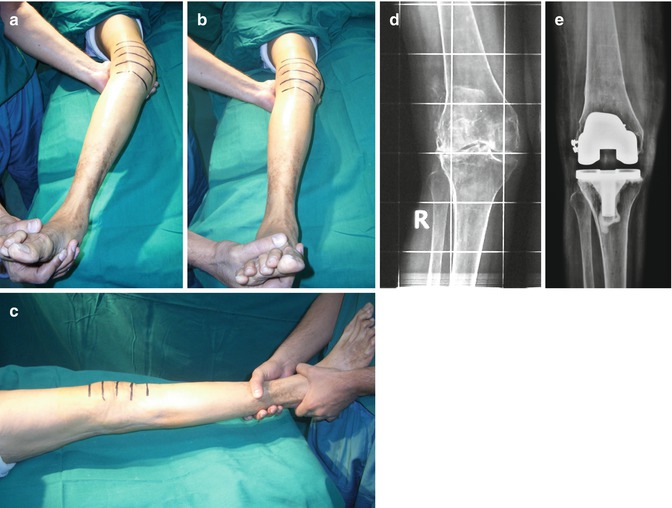
Table 4.1
Classification of valgus knees
Type 1: Correctible valgus, no associated deformity, MCL intact |
Type 2: Rigid valgus, no associated deformity, MCL intact |
Type 3: Valgus with hyperextension deformity, MCL intact |
Type 4: Valgus with flexion deformity, MCL intact |
Type 5: Severe valgus with incompetent MCL |
Type 6: Valgus with extra-articular deformity |
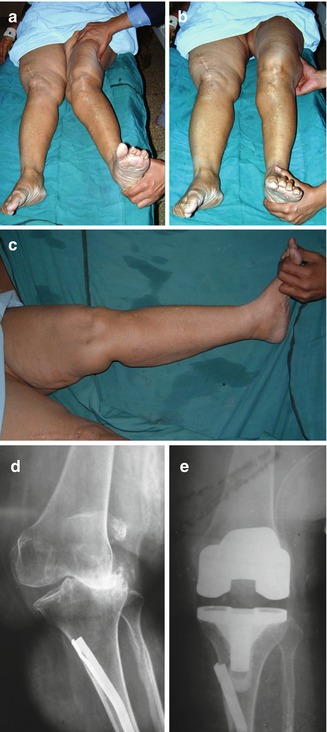
Fig. 4.4
Type 1 valgus deformity. (a) Clinical photograph showing maximum valgus deformity with a valgus stress applied with patient under anaesthesia. (b) Clinical photograph showing complete correctibility of valgus deformity with a varus stress applied with patient under anaesthesia. (c) Clinical photograph showing no associated flexion or hyperextension deformity with patient under anaesthesia. (d) Preoperative standing anteroposterior knee radiograph showing the valgus deformity. (e) Postoperative standing anteroposterior knee radiograph showing restoration of knee alignment with a cruciate-substituting design
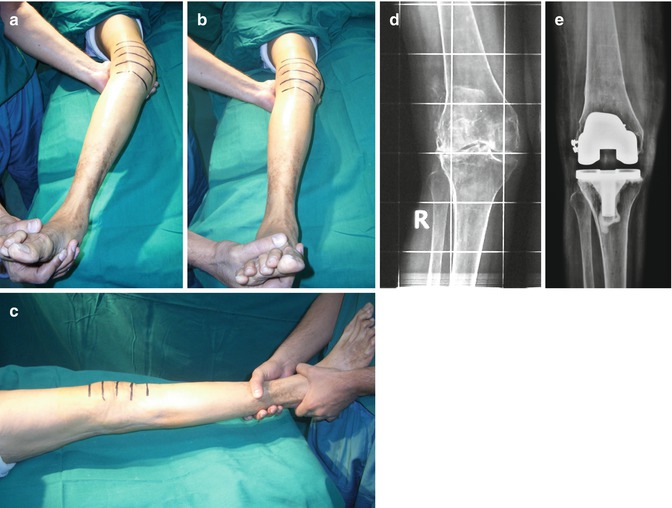
Fig. 4.5




Type 2 valgus deformity. (a) Clinical photograph showing maximum valgus deformity with a valgus stress applied with patient under anaesthesia. (b) Clinical photograph showing partial correctibility of valgus deformity with a varus stress applied with patient under anaesthesia. (c) Clinical photograph showing no associated flexion or hyperextension deformity with patient under anaesthesia. (d) Preoperative standing anteroposterior knee radiograph showing the valgus deformity. (e) Postoperative standing anteroposterior knee radiograph showing restoration of knee alignment with a cruciate-substituting design. A lateral epicondylar osteotomy (LEO) was required in this case due to the rigid nature of the deformity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








