I. Patellar Fracture
A. Anatomy—The patella is the largest sesamoid bone in the body. Its subcutaneous location leaves it susceptible to injury from direct blows (e.g., falls, dashboard injuries). Three-fourths of the patella’s proximal posterior surface is covered with some of the thickest articular cartilage found in the human body. Its articular surface is divided by a longitudinal ridge separating it into medial and lateral facets. The bulk of the quadriceps tendon inserts directly into the proximal pole. Longitudinal extensions of the quadriceps tendon pass medial and lateral to the patella and insert directly on the anterior tibia. A thin layer of the fibers pass anterior to the patella and becomes confluent with the patellar tendon. Deep, transversely oriented fibers pass from the femoral epicondyles to the patella, making up the patellofemoral ligaments.
B. Biomechanics—The extensor apparatus consists of the quadriceps muscle and tendon, the patella, and the patellar tendon. Secondary extensors of the knee include the iliotibial tract and the medial and lateral patellar retinacula. The patella functions to improve the lever arm of the extensor mechanism. Its contribution increases toward extension, increasing the force by nearly 30% at maximal extension. Through the patella, the quadriceps exerts an anteriorly directed translational force on the tibia that is exposed to complex loading consisting of tensile, bending, and compressive forces. The magnitudes of these forces vary with the degree of flexion, with maximal tensile forces occurring at 45° to 60° of flexion. Joint contact forces of 3.3-times body weight occur during stair climbing and up to 7.6-times body weight occurring during squatting. The size of the patellofemoral contact area is 2 to 4 cm2, or 13% to 38% of the articular surface, and is oriented in a transverse band through most of the range of motion.
C. Classification—Patellar fractures are most commonly classified based on the morphology of the fracture (Fig. 9-1). The most common mechanisms of injury consist of direct blows to the patella (e.g., dashboard injury), indirect trauma (e.g., sudden, rapid flexion of the knee against a maximally contracted quadriceps), or a combination thereof. Direct trauma typically results in minimally displaced comminuted fractures, whereas indirect trauma usually results in displaced transverse fractures. Osteochondral injuries that can occur with patellar dislocations usually involve the medial patellar facet. They are caused by impaction of the facet with the lateral ridge of the lateral femoral condyle, sometimes avulsing an osteochondral fragment from the lateral condylar ridge as well. A small, sometimes radiographically benign-appearing distal pole fragment, which can include a significant piece of articular cartilage, is termed a sleeve fracture; it occurs in the skeletally immature patient.
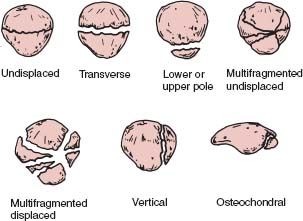
FIGURE 9-1 Classification of patellar fractures. (From Bedi A, Karunakar MA. Patella fractures and extensor mechanism injuries. In: Bucholz RW, Court-Brown CM, Heckman JD, et al, eds. Rockwood and Green’s Fractures. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010, with permission.)
1. History—A direct blow to the anterior knee or forced and rapid knee flexion against a contracted quadriceps, anterior knee pain, and an inability to forcibly extend the knee suggest the diagnosis.
2. Examination—Patients should be examined for an extensor lag or a palpable defect suggesting disruption of the extensor mechanism. The anterior knee soft tissues should be inspected, since they are frequently compromised after direct trauma. The knee and lower extremity should also be examined for any associated injury suggested by the mechanism of injury.
3. Imaging—The patella can be difficult to discern on anteroposterior (AP) radiographs. However, it is well visualized on lateral radiographs, and articular step-off and diastasis can be assessed. Tangential views can be useful for evaluating marginal or the rare vertical fracture. Bilateral films are useful when a bipartite (accessory ossification center) patella is suspected, since these rarely occur unilaterally (Fig. 9-2). Computed tomography (CT) is usually unnecessary. Magnetic resonance imaging (MRI) may be used to diagnose sleeve fractures. Bone scintigraphy may be useful for diagnosing occult fractures.
E. Treatment—Despite largely favorable results of both conservative and operative management of patellar fractures, some loss of knee flexion usually occurs; an increase of up to 40% in patellofemoral arthrosis may also occur.
1. Nonoperative treatment—Nonoperative treatment is indicated for nondisplaced fractures, which are defined as less than 2 mm of step-off and less than 3mm of diastasis without an extensor lag. Treatment consists of a long leg cylinder cast, weightbearing as tolerated for 4 to 6 weeks, and then careful progressive range of motion with subsequent quadriceps strengthening. Almost 90% of patients heal with normal or slightly impaired function.
2. Operative treatment—Operative treatment is indicated for displaced fractures with loss of extensor function. The goals of surgery should be preservation of patellar function and anatomic reduction of the articular surface. A longitudinal midline incision is recommended, as it is useful for other knee procedures in case they become necessary. A defect in the medial and lateral retinaculum is usually noted during exposure of the fracture, and it should be repaired with the fracture. The reduction should not be based on the anterior patellar cortex because significant plastic deformation can occur from the injury. Instead, the reduction of the articular surface can be inspected through a medial parapatellar mini-arthrotomy or with arthroscopic assistance. Additional injury to compromised soft tissues should be reduced by avoiding compressive dressings and prolonged contact with ice. Consideration should be given to aspiration of anterior hematomas if the skin is tense and surgery will be delayed. Several options for fixation are available (Fig. 9-3).
• Modified tension band wiring—Popularized by the AO/ASIF group, modified tension band wiring is indicated for distracted, transverse, and some comminuted fractures. It consists of provisional fixation of the fracture with two 2.0-mm Kirschner wires, followed by augmentation with an 18G wire passed around the Kirschner wires and across the anterior aspect of the patella to serve as the tension band component of the construct. The wire can be placed in a “figure-eight” or a circular fashion. The anterior tension wire then converts the distractive force across the anterior patella into compressive force on the articular side of the patella. This technique requires early motion to work properly. The most common technical error occurs when the tension wire is not brought into direct contact with the patellar poles. The intervening soft tissues gives way with loading, allowing the fracture to distract.
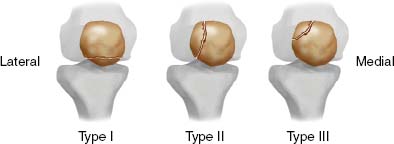
FIGURE 9-2 Saupe’s classification of accessory ossification centers of the patella. Type 1, inferior pole, 5%; Type II, lateral margin, 20%; Type III, superolateral pole, 75%.
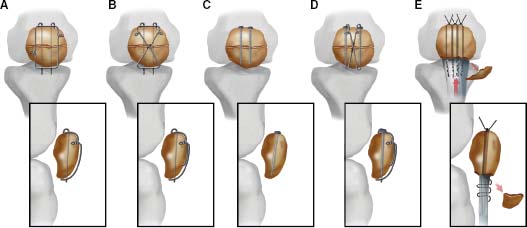
FIGURE 9-3 Techniques of patellar fracture fixation. A. Modified tension band wiring using a circular configuration. B. Modified tension band wiring using a figure-eight configuration. C. Lag-screw fixation. D. Combination cannulated lag screw and tension band wiring. E. Partial patellectomy. Note: The tendon is reapproximated at the level of the articular surface of the patella.
• Lag-screw fixation—Lag-screw fixation can be used to stabilize fragments in comminuted patellar fractures, thereby creating a fracture amenable to tension band wiring. It can be used as an alternative to tension band wiring, with comparable stability reported. There must be good quality bone for this technique to be used alone. There is concern that lag-screw fixation alone may be less able to withstand bending forces.
• Combination lag-screw fixation and tension band wiring—More recently, a technique combining cannulated lag-screw fixation and tension band wiring has been described. The fracture is initially stabilized with two 4.0- or 4.5-mm cannulated lag screws. An 18G wire is then passed through the center of the screw and across the anterior patella to act as a tension band. This technique results in a construct with a greater load to failure compared with either lag-screw fixation or tension band wiring alone.
• Partial patellectomy—Partial patellectomy is reserved for fragments not amenable to internal fixation. It usually consists of a comminuted distal pole and an intact proximal pole. The irreparable fragments can be resected, and the patellar tendon repaired with sutures through bony tunnels to the proximal fragment. The tendon should be repaired close to the articular surface to minimize articular step-off and prevent patellar tilt in the sagittal plane. A load-sharing wire passed through the patella and the tibial tubercle can be used to protect the repair. Problems with this technique include patella baja, altered patellar mechanics, weakened quadriceps, and decreased patient satisfaction rates.
• Total patellectomy—Total patellectomy may be the only alternative in severely comminuted displaced patellar fractures without any significant remaining articular fragments. The remaining defect can be repaired with a purse-string, vertical, or transverse closure. In addition, the repair may be reinforced with a quadriceps flap (Fig. 9-4). Loss of range of motion, extensor lag, quadriceps weakness, and discomfort after patellectomy are common.
F. Postoperative Management—Postoperative management includes initial immobilization and immediate weightbearing as tolerated. There is evidence that tensile forces across the patella are greater during attempts at nonweightbearing ambulation as the patient tries to keep the leg off the ground. Emphasis is placed on early range of motion (as the quality of fixation allows). Early range of motion is an essential principle in tension band fixation and is important in decreasing postoperative stiffness. The repair can be protected with the use of a locked hinge knee brace in which the amount of flexion is increased every 2 weeks (as the patient tolerates and as range of motion and quadriceps strength return).
G. Complications
1. Infection—Infection is rare. The risk may be increased by injury-compromised soft tissues and host factors.
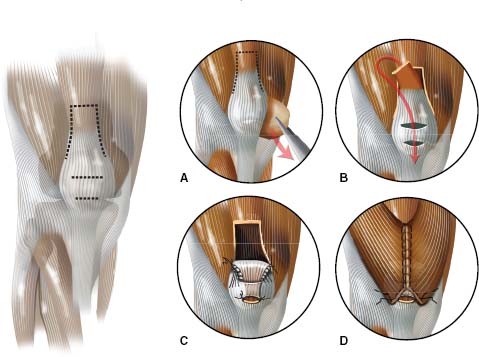
FIGURE 9-4 Miyakawa technique of patellectomy. A. Excision of the patella and outline of the incision in the quadriceps. B. Partial- thickness flap of the quadriceps tendon turned distally. C. Quadriceps flap passed through incisions in the area previously occupied by the patella. D. Proximal reconstruction with the vastus medialis obliquus and the vastus lateralis brought together over the quadriceps flap.
2. Loss of fixation—Loss of fixation may be secondary to underestimated fragment comminution most commonly involving the distal pole. If caught early, it can be treated with immobilization. If significant displacement occurs, partial patellectomy may be the best option.
3. Loss of range of motion—Slight loss of range of motion is common. The incidence can be reduced with secure internal fixation allowing early range of motion (within 1 or 2 weeks).
4. Posttraumatic arthrosis—Posttraumatic arthrosis is relatively common. One long-term study demonstrated a 70% incidence of arthrosis in patellar fracture compared with a 31% incidence in the contralateral, noninjured knee.
5. Nonunion—Nonunion was common when all patellar fractures were treated nonoperatively (up to 55%). With modern operative techniques, the nonunion rate is reported to be 1% or less.
6. Symptomatic Hardware—Symptomatic hardware is common secondary to the subcutaneous location of the patella.
II. Patellar Tendon Rupture
A. Overview—Patellar tendon rupture is an uncommon injury and in contrast to quadriceps tendon rupture, typically occurs in younger patients (younger than age 40). Thought to be the result of recurrent microtrauma and chronic tendon degeneration, patellar tendon rupture is associated with jumping sports (e.g., basketball), hence the term jumper’s knee. In face, in one large study, 97% of biopsy specimens from ruptured patellar tendons demonstrated degenerative changes such as mucoid degeneration and calcific tendinopathy. Most commonly, ruptures occur at the proximal insertion of the patellar tendon. Most often, they are unilateral but can occur bilaterally, especially in patients with impaired collagen strength (e.g., rheumatoid arthritis, systemic lupus erythematosus, diabetes mellitus, and chronic renal failure) and patients on systemic corticosteroid therapy. They also occur after local steroid infiltration. Another common mechanism for patellar tendon rupture may be direct trauma. In one study of 35 patellar tendon ruptures, 27 occurred in motorcycle accidents. Finally, patellar tendon rupture can occur as a complication of total knee arthroplasty, patellar tendon harvest for ligament reconstruction, and devascularization after lateral retinacular release procedures.
B. Anatomy—The patellar tendon is approximately 4 mm thick at the midsubstance and 5 to 6 mm thick as its insertion on the tibial tubercle. It narrows slightly from proximal to distal. The distal expansions of the vastus medialis and vastus lateralis form the medial and lateral retinacula, respectively. Some 70% to 80% of the dry weight of the patellar tendon is collagen, of which 90% is Type I and approximately 10% is Type III. The blood supply originates from the medial and lateral geniculate arteries and the recurrent tibial artery, which branches through the fat pad and retinaculum to enter the tendon at its proximal and middle portion. The proximal and distal insertions, being relatively avascular, are also the most common sites of rupture.
C. Biomechanics—The largest tensile stress within the tendon occurs at 60° of flexion and is estimated to be 3.2 times the body weight during stair climbing. Strain at the insertion sites is three to four times greater than that at the midsubstance.
D. Classification—Patellar tendon ruptures have been classified according to the morphology of the tear, the location of the tear, and temporal factors. One classification, based on the age of the tears, was found to be useful with regard to prognosis and treatment options. Acute tears, less than 2 weeks old, can be repaired primarily and have an excellent prognosis. In contrast, chronic tears, more than 2 weeks old, tend to require more extensive surgical procedures for repair and are associated with a more guarded prognosis.
E. Evaluation
1. History—Acutely, the patient usually gives a history consistent with forced knee flexion against a maximally contracted quadriceps. The patient may describe a ripping sensation or an audible pop associated with pain and an inability to immediately bear weight. Chronically, the patient may complain of weakness, instability, and an inability to fully extend the leg.
2. Examination—Acutely, a hemarthrosis, a palpable defect, patella alta, and either a partial or a complete active extension loss may be found. Chronically, the defect may be filled with organized reparative tissue; in addition, the patient may have significant quadriceps atrophy and a gait abnormality characterized by forward flinging of the affected leg during the swing phase.
3. Imaging—Plain radiographs are helpful, with the lateral view being most diagnostic because it can demonstrate patella alta (Fig. 9-5). The use of ultrasonography in the diagnosis of chronic tears of tendinitis has been described, but is operator dependent. MRI may be useful when another intraarticular injury is suspected or if the diagnosis is in question.
F. Treatment and Treatment Rationale—The treatment of patellar tendon rupture is surgical. Nonoperative treatment cannot restore complete extensor function.
1. Acute repair—Acute repair is most desirable because the tendon can usually be repaired primarily. This treatment is associated with the best restoration of function and overall outcome.
• Surgical technique—A midline longitudinal skin incision is used for the surgical approach and is extended to fully expose the rupture and either the patella or tibial tubercle depending on the site of rupture. The dissection is carried medially and laterally to expose the retinacular tears. The tendon is repaired using a No. 5 nonabsorable suture woven through the tendon using a Bunnell or Krakow technique, and the suture is then passed through bone tunnels at the approximate site (Fig. 9-6). Intraoperative lateral radiographs are recommended before final tightening of the sutures to verify proper position of the patella. The retinacular tears should be repaired as well. The repair can then be reinforced using an 18G cerclage wire (McLaughlin wire), umbilical tape, or a large suture proximal to the patella and through a bone hole in the tibial tubercle. An absorbable, braided polydioxanone (PDS) suture cable is preferred for this purpose (Figs. 9-7 and 9-8).
2. Late repair—Late repair is associated with a greater operative challenge and a worse outcome. Primary repair is often not possible after a delay of more than 6 weeks. After a delay of several months, a period of patellar traction may be needed to combat a chronic quadriceps contraction. With time, degenerative changes may occur within the patellofemoral articulation, and the ruptured tendon becomes contracted and bound in scar. Reconstructive choices include primary repair with hamstring or fascial lata autograft augmentation or in salvage cases, extensor mechanism allografts (Fig. 9-8 and 9-9).
G. Postoperative Management—Postoperative management includes immediate gentle passive range of motion followed by gentle active flexion at 2 weeks after surgery and active extension at 3 weeks. Initial toe-touch, protected weightbearing progresses to full weightbearing by 6 weeks. During this time, the repair is protected in a hinged knee brace, which is progressively opened as range of motion returns. Unrestricted activity is allowed after 4 to 6 months, when complete healing has occurred and quadriceps strength is within 90% of the unaffected extremity.
H. Complications—Knee stiffness and quadriceps weakness are the most common complications after patellar tendon repair. They can be combated with a well-supervised rehabilitation program emphasizing range of motion and quadriceps strengthening. Other complications include persistent hemarthrosis, rerupture, and patella baja.
III. Quadriceps Tendon Rupture
A. Overview—Quadriceps rupture, as opposed to patellar tendon rupture, typically occurs in older patients, over 40 years old (average 47 years), and is typically associated with preexisting tendinopathy. This condition results from repetitive microtrauma associated with jumping sports (e.g., basketball). The level of the tear is also associated with age. In one study, rupture at the tendon-bone junction occurred in 75% of patients over the age of 40, whereas midsubstance tears occurred in 71% of patients younger than 40 years. Bilateral ruptures have been reported in association with anabolic steroid use and chronic metabolic disorders such as diabetes mellitus, inflammatory arthropathies, and chronic renal failure.
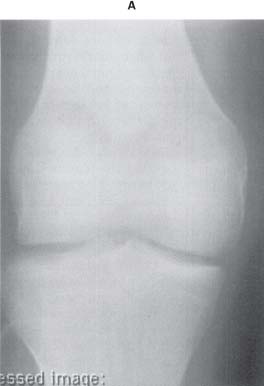

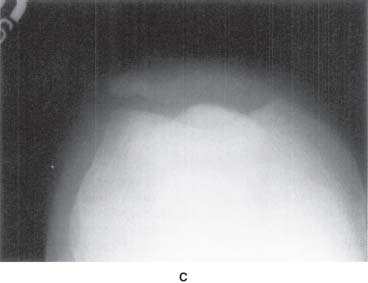
FIGURE 9-5 A and B. AP and lateral radiographs demonstrating a high-riding patella consistent with a patellar tendon rupture. Note the distal pole avulsion fragment. C. Sunrise view of the same knee. Note the absence of the patella in the trochlear groove.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







