Chapter 133 Extensor Mechanism Disruption After Total Knee Arthroplasty
Disruption of the extensor mechanism after total knee arthroplasty (TKA), although still feared, should not be considered untreatable. Demanding but proven surgical techniques can restore durable function. Nonetheless, extensor loss still rivals deep infection as the worst outcome of a knee replacement and the challenge is clear—this structure sustains huge tensile loads.120
The true scale of ruptured extensor mechanism complicating TKA is difficult to quantify. In 1999, Aracil et al2 reported 5 cases out of 312 primary TKAs (1.6%). The relative contribution of extensor failure in failed TKAs varies. Data from the 2006 North American Knee Arthroplasty Revision Study identified 6 revisions of 290 that were done for a ruptured extensor (2.1%).92 One study reported in 1999 that significant extensor lag—from rupture, patella baja, or patellectomy—accounted for 6.6% of revisions.99 The results of first-revision arthroplasty for a ruptured extensor mechanism are inferior to revision knee arthroplasty in general, and this complication is particularly problematic in failed revision knee arthroplasty surgery.104
Although extensor mechanism rupture is a recognized cause of knee arthroplasty failure,76,111 it does not appear in most national joint registries. Data from Australia list up to 27 categories of failure requiring revision arthroplasty, but not extensor mechanism deficiency.4,5 The New Zealand Registry79 lists 19 modes of failure and a British community registry41 lists 11, but neither specifies extensor mechanism rupture. Our understanding would improve if this mode of failure were included in diagnostic schemes of how knees fail.77
Extensor mechanism complications, including maltracking, patellar component wear and loosening, patellar fracture, and extensor rupture, have all been reviewed.* This chapter, like other reviews, focuses exclusively on problems that separate the quadriceps muscle from the tibial tubercle.†
Anatomic Location of Extensor Rupture
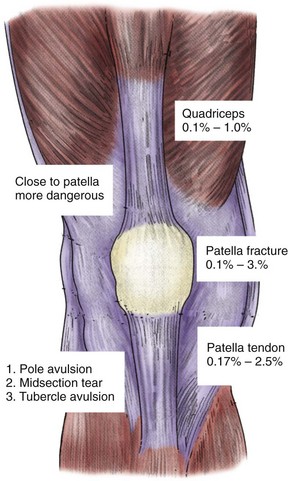
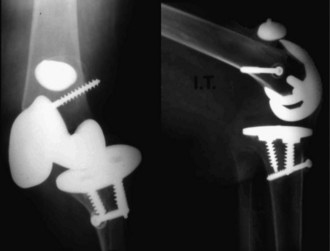
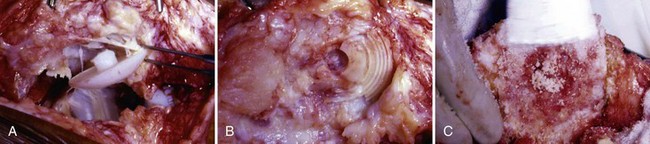
Although we generally think of the patellar tendon when extensor rupture complicates TKA, failure may occur anywhere from the quadriceps muscle to the tibial tubercle. The anatomic location (quadriceps tendon, patellar bone, or patellar tendon) has implications for prevention, prognosis, and treatment (Fig. 133-1). Transverse patellar fractures that disrupt the extensor mechanism are usefully included with soft tissue ruptures because the usual fracture care is not applicable in the presence of an arthroplasty. If extensor rupture is associated with sepsis18,33,34,68,78 or instability,75,98 more complex procedures, including concurrent revision, will be required (Fig. 133-2).
Quadriceps Tendon Rupture
Incidence and Prevention
The quadriceps tendon is the least common site of extensor disruption. Lynch and colleagues69 have cited a 1.1% incidence (3 of 281) of quadriceps tendon rupture after TKA. This figure, from 1987, is probably high by current standards. Dobbs and associates31 have identified 24 of 23,800 primary TKA patients (0.1%) from the Mayo Clinic with a partial or complete quadriceps tendon rupture. The actual risk nationwide probably lies somewhere between 0.1% and 1.0%.
Systemic factors beyond the control of the surgeon may increase the risk for quadriceps tendon rupture. Rheumatoid arthritis,36 diabetes mellitus, chronic renal failure, obesity, and hyperthyroidism are risk factors for quadriceps tendon rupture, with or without knee arthroplasty.31,46,102,105 Aggressive resection of patellar bone at the time of resurfacing may compromise the attachment of the quadriceps tendon to the patellae; a lateral patellar retinacular release that extends proximally and then medially across the tendon may increase the risk.69 Patellectomy to treat complications of TKA has resulted in quadriceps tendon rupture in two of nine cases.23
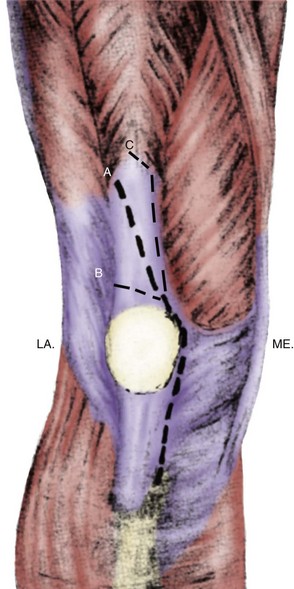
An insidious cause of quadriceps tendon rupture may be the location and orientation of the arthrotomy. If the popular medial parapatellar approach strays transversely across the quadriceps tendon, especially if it is close to the proximal part of the patella, many if not all the longitudinal fibers of the tendon will be transected, with little soft tissue for repair. Such an arthrotomy will be held together only by sutures until the surgery heals (Fig. 133-3).
An arthrotomy that transects the quadriceps tendon medially to laterally has been recommended (called the wandering resident approach because of its inadvertent origins) for difficult exposures.48 It seems best, with this approach, to cross the tendon proximally to the patella to maintain a long section for side to side closure. In this respect, the wandering resident approach resembles the quadriceps snip,3,7,39,47,74 which does not seem to risk quadriceps tendon rupture. Ideally, none of the longitudinal fibers in the structures (e.g., quadriceps tendon, patella, patellar tendon and its attachments to the patella and the tibia) that resist the huge tensile force in normal knee function would be transected by the surgical approach.51
Treatment
Few quadriceps tendon ruptures after TKA have been reported. A technique described by Scuderi95 in 1958 for the treatment of quadriceps tendon rupture in the absence of knee arthroplasty (turning the superficial portion of the tendon back down onto the patella) was applied successfully by Fernandez-Baillo and colleagues36 to a TKA patient. This repair was reinforced with Dacron tape and the knee immobilized in a cast for 6 weeks. Sinha and coworkers100 have described attempted primary repair and Achilles tendon reconstruction for ruptured quadriceps tendons, with mixed results. The Leeds-Keio prosthetic ligament has been used2 and extensor mechanism allografts, originally described for insufficiency resulting from patellectomy and rupture or avulsion of the patellar tendon, work well to repair the quadriceps tendon (Fig. 133-4).18,32,78
Dobbs and colleagues31 reported good results with conservative treatment of partial quadriceps tendon tears. By contrast, 7 of 11 complete tears treated surgically, without supplementary biologic tissue, suffered poor outcomes and a high complication rate. The technique in 10 was adapted from Scuderi’s 1958 surgery,95 with or without drill holes in the patella; 2 were reinforced with Marlex mesh (CR Bard, Murray Hill, NJ), which is recommended and illustrated in that report. Complications in the surgical cases were legion: four with rerupture, one with recurvatum (suggesting extensor insufficiency) and instability, and two with deep periprosthetic infection necessitating resection arthroplasty that ended in amputation for one patient. Motion was maintained in the four successful cases, with 0 to 10 degrees of extensor lag and flexion ranging from 60 to 125 degrees. In one patient, a revision knee arthroplasty was performed concurrently. The results with extensor mechanism allograft reconstruction are superior.78
Incidence and Prevention of Transverse Patellar Fractures
Patellar fractures complicating TKA usually do not interrupt the extensor mechanism. The common vertical fracture can often be treated without surgery unless a patellar component has loosened. Some of these fractures may result from rotational positioning problems of the tibial and femoral components.13,72,73,103 Improved implant design and surgical techniques make old information regarding causes and incidence irrelevant. Sinha and colleagues100,101 have indicated that the incidence of all patellar fractures after TKA ranges from 0.27%116 to 5.4%. The incidence with the original Insall-Burstein posterior-stabilized prosthesis was as high as 8.4%, attributable to larger (thicker) patellar components, prominent anterior trochlear groove, increased flexion, and higher level of activity.52,94 Most of those fractures, however, were longitudinal, without disruption of the extensor.
All studies of patellar fracture after TKA have concluded that transverse fractures with extensor mechanism disruption (and extensor mechanism lag) are uniquely problematic. Goldberg and colleagues,43 in a 1988 report, segregated patellar fractures after arthroplasty by anatomic site. Goldberg types II (fractures involving the implant-cement interface or quadriceps mechanism) and IIIA (inferior pole fracture with patellar ligament rupture) resulted in extensor discontinuity and accounted for 6 of 36 (16.7%) and 8 of 36 (22.2%) patellar fractures in their series, respectively, establishing that over one third of all patellar fractures disrupted the extensor in that era.
More recently, Keating and colleagues58 identified 177 patellar fractures in 4583 TKAs (3.9%). They segregated them into four groups: (1) 22 vertical fractures with a well-fixed implant and an intact extensor mechanism; (2) 21 with disruption of the extensor mechanism of less than 1 cm; (3) 17 with disruption of the extensor by more than 1 cm; and (4) 114 with a loose component but an intact extensor mechanism. Accordingly, only in group 3, 17 of 4583 cases had a ruptured extensor (0.37%) with the patellar fracture. Ortiguera and Berry81 have identified 85 fractures after 12,464 TKAs (0.68%) at the Mayo Clinic. Only 12 fractures (0.09%) were associated with extensor mechanism rupture.
Risk Factors for Extensor Mechanism Disruption Through the Patella
Sinha and associates,100 in their careful review of patellar fractures, found three factors, that statistically increased the risk for patella fracture: resurfacing, lateral patellar retinacular release, and revision surgery. Several trends have emerged, including a decreased incidence of all nonseptic complications (including patellar fractures and patellar tendon ruptures) and growing evidence that resurfacing delivers, on average, slightly better pain relief.89 Data from three representative studies have illustrated this trend,61,114,117 arguing against leaving the patella unresurfaced for fear of complications and in favor of better implant designs and superior surgical technique. Extensor mechanism maltracking probably heightens the risk for all patellar complications, including fracture.72 If internal rotation of the femoral and/or tibial components is at the root of a patellar fracture, most treatments short of revision arthroplasty are likely to produce poor results. Hozack and coworkers49 reviewed their patellar fractures in 1988, predating studies that link internally rotated components and patellar complications.13,16 Revision surgeries were not usually done and the results, consistent with subsequent studies on the surgical treatment of extensor mechanism rupture through the patella, were poor.57,81
Whether avascular necrosis or patellar maltracking has a greater impact on the development of patellar fractures is unknown. Avascular necrosis of the patella is more frequent after lateral patellar retinacular release.96 However, lateral releases are performed for maltracking, which usually results from internal rotation positioning of tibial and/or femoral components. Does the release itself cause avascular necrosis and fracture, or does maltracking cause the lateral portion of the patella to dislocate, separating itself from that portion of the patellar component that wants to stay in the trochlear groove?46,91,93
The statistical significance of lateral patellar retinacular release was indicated by Healy and colleagues in 1995,46 Scott and associates in 1982,93 and Tria and coworkers in 1994.106 Again, it is difficult to argue against performing lateral release and even more difficult to discern whether this effect originates from avascularity, maltracking, or a combination of the two. In general, with improved designs, greater understanding of the importance of rotational positioning of femoral and tibial components, and improved surgical approaches,15 the incidence of lateral patellar retinacular release has decreased dramatically in clinical practice.
Component positioning is certainly the factor most directly under the control of the surgeon. Other factors postulated but unproven to increase the risk for fracture via avascular necrosis include compromise of the patellar blood supply by excision of the infrapatellar fat pad and thermal necrosis of bone from the heat of polymethylmethacrylate cement as it polymerizes.26,44
Progressive compromise of patellar circulation after medial arthrotomy, fat pad resection, and then lateral patellar retinacular release was quantified by laser Doppler to be 30.6% of normal.50 In a hydrogen washout study, the same surgical sequence demonstrated reduction to 17% of control.80 The threshold at which a patella necroses has not been established. Although the fat pad contributes to the blood supply of the patella, the link has not been established between patellar fracture and its removal. Many surgeons routinely excise it, without an apparent increase in patellar fractures, much less disruption of the extensor mechanism. Cadaver studies have demonstrated that the prepatellar or anterior blood supply is very important.56
Thermal necrosis may result from polymerization of polymethylmethacrylate bone cement, but to a depth that is unlikely to result in structural impairment. In fact, when this effect is avoided with uncemented patellar implants, the incidence of patellar fracture is higher.46,91 Bone saws create high temperature in bone.66
A frequent concern is that a thicker resurfaced patella will result in a stiff knee. A biomechanical test measured a 22% increase in anterior patellar strain with a conventional resurfacing prosthesis and a 28% increase with an inset-style patellar prosthesis. Increased strain is likely to increase the risk for fracture. Progressive overresection of bone was significantly more detrimental with inset designs.118
The final statistically significant feature associated with patellar fractures is revision surgery. Grace and Sim44 found patellar fractures in 3 of 495 revision knee arthroplasties (0.61%) and 9 of 7754 primary replacements (0.12%; P < .05). Multiple surgeries have a deleterious effect by virtue of thinner, weaker, often osteolytic patellar bone, compromised vascularity, and poor flexion. This can be improved with attention to detail in the surgical approach.97
Patellar Fractures: Treatment
Patellar fractures must be treated differently when they complicate a TKA. Without an arthroplasty, the patella is a normal size and shape and blood supply is intact, and it is important to reestablish articular congruence. Consequently, tension band wiring based on the principles of Pauwel is appropriate.27 The fracture fragments are held by two parallel wires, around which 18-gauge stainless steel wire is wrapped in a figure-of-eight and then tightened. This induces a force vector across the anterior aspect of the patella that may be strong enough to create a gap on the articular side. With knee flexion, the femoral condyle theoretically compresses the gap and forces the fracture fragments together.107 Conceptually, tension should be converted to compression, but this mechanism has been difficult to validate in experimental models.115
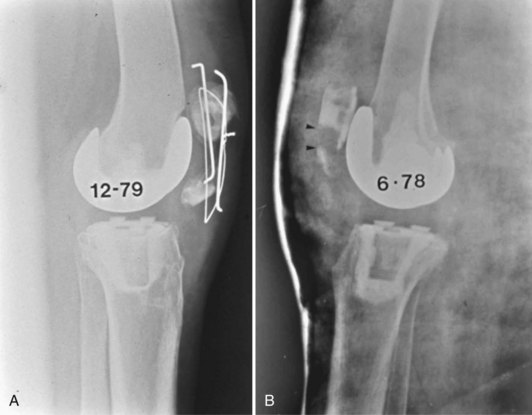
A resurfaced patella, by contrast, cannot be expected, even theoretically, to benefit from tension band wiring. There is barely enough room to admit the parallel wires. The deep surface of the bone, usually forced together by tension banding, no longer exists, and thus the principles are not applicable. Furthermore, if the patella was not avascular at the time of fracture, there is a strong possibility that the surgical approach has compromised the blood supply, so important for fracture healing. Simply stated, tension band wiring is not recommended for patellar fractures complicating knee arthroplasty (Figs. 133-5 and 133-6).
Despite fracture displacement, loose patellar prostheses, and even an acute extensor lag, it is useful to temporize before fixing a fractured resurfaced patella. The knee joint can usually be immobilized in extension and reevaluated within 2 to 4 weeks. Many of these patellae, although relatively avascular and fragmented, may consolidate without surgery (Fig. 133-7). Immediate intervention can only remove the loose component and perhaps cerclage the residual bone fragments, and has been associated with poor results.
A persistent lag or a loose component after 4 to 6 weeks clarifies the need for surgery. If the lag improves, surgery can be limited to removal or revision of a loose button. Prerevision computed tomography (CT) scanning may help determine whether the rotational positioning of the tibial and femoral components would indicate revision to improve tracking.13
Keating and colleagues57 have observed that four of nine patients with patellar fractures and loose components suffered infection after simple removal of the components. Both patients in whom open reduction plus internal fixation was performed ended with nonunion. They recommended nonoperative treatment and acknowledged the advantage of patellectomy with repair of the residual tendon. Ortiguera and Berry81 have described 12 patellar fractures with extensor disruption out of 85 that complicated knee arthroplasty. One patient treated with prolonged immobilization (and no surgery) was pain-free, with a 5-degree lag. Of six who underwent open reduction and internal fixation, one patella united. Five had partial patellectomies and tendon advancement to bone, with three requiring additional surgery. Six of the 12 suffered complications; 5 underwent reoperations, and 7 had pain, patellar instability (suggesting tibial or femoral internal rotation), or extensor weakness. Both of these studies illustrate examples of catastrophically failed tension band wiring.
A fixation device for inferior pole avulsion fractures of the patella (in the absence of knee replacement), the basket plate, has been described.58 As yet unreported in the presence of a knee replacement, it risks failure for many of the same reasons as tension band wiring—limited bone stock and avascularity. Although cerclage fixation has been recommended for patellar fractures with an extensor lag, no data substantiate this recommendation, other than the abysmal results with tension band wiring. The ultimate recourse will be reconstruction with an extensor mechanism allograft, something that if considered earlier in the treatment of these patients, may avoid the complications of multiple procedures (Fig. 133-8). The technique can be modified, as will be described later in the case of the patellectomy patient, to safeguard the patient’s own patellar tendon attachment to bone should the graft fail.
Patellar Tendon Rupture and Avulsion
Risk Factors
Patellar tendon rupture or avulsion has been reported in 0.17% to 2.5%22,69,87,92 of patients with TKA. Careful attention to detail during difficult exposures with the extensor mechanism tenolysis approach should spare the patellar tendon and its attachment to the tibia.97 Aracil and associates2 reported patellar tendon disruptions with TKA for ankylosed knees, revisions, after distal realignment procedures, and after a Maquet osteotomy. Some surgeons recommend the insertion of a pin or Kirschner wire (K wire) through the patellar tendon and into the tubercle to protect it during difficult exposures. Although a useful reminder to exercise caution, inordinate force will tear the tendon through the pin. Medial rather than midline arthrotomies will stay to the side of the patellar tendon, whereas arthrotomies that divide any portion of the tendon necessarily elevate some of its insertion to bone, a partial rupture from the outset.
Treatment
Because of its relative rarity, large studies have not been conducted and the ideal treatment is uncertain. Conventional wisdom once recommended arthrodesis in these cases, but the resulting disability is severe. More functional reconstructions have been described, including one chronic, neglected patellar tendon rupture in the presence of severe osteoarthritis that was treated by patellectomy and TKA with advancement of the tendon.24 Only proximal patellar tendon ruptures would be structurally amenable to this treatment; flexion may be restricted and the considerable benefit of the patellar fulcrum would be lost.
The typical appearance of midsubstance patellar tendon ruptures in TKA-attenuated fibrous tissue stretched over the usual area of the patellar tendon will surprise surgeons35 accustomed to the mop ends of acute ruptures in the absence of a TKA. Simply put, the very strong tensile bands of collagen have suffered plastic deformation and are gone, and attempts to shorten and repair the residual structure without supplementary tissue are tempting but futile.
Surgeons have sutured the end of the avulsed tendon into a trough in the tubercle and supplemented the repair with cerclage wiring.1 Fujikawa and coworkers37 treated 25 ruptures with a Leeds-Keio synthetic ligament with good results in the 18 that they assessed. Aracil and colleagues2 also reported success with this device.
Other techniques, studied in limited numbers, include reconstructions with semitendinosus,22 fascia lata (Fig. 133-9), Dacron 4-mm vascular grafts (U.S. Catheter and Instrument, Glen Falls, NY), and bovine xenografts.91 Zanotti and associates119 have described success with the bone–patellar tendon–bone complex used for anterior cruciate ligament reconstructions. The patella was fused to the proximal end of the tibia in an unusual case of ruptured patellar tendon complicating a TKA in the presence of metabolic bone disease.59 Recently, a quadriceps tendon was successfully turned down to repair what must have been a proximal patellar tendon rupture.
Extensor Mechanism Allografts
Indications
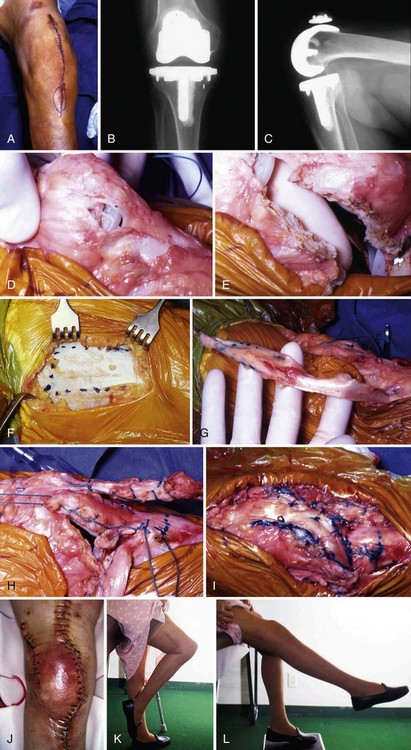
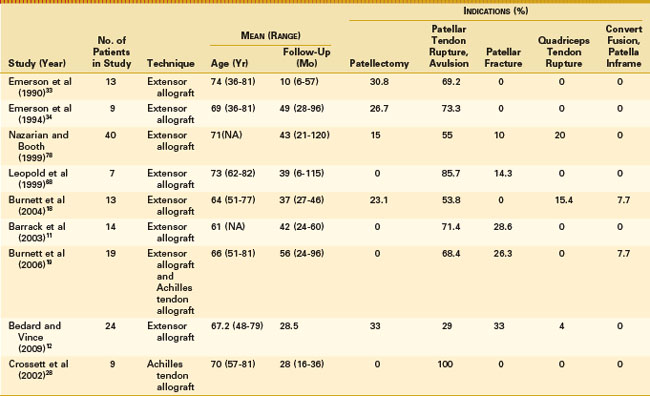
Reconstruction with an intact allograft consisting of the tibial tubercle, patellar tendon, patella, and quadriceps tendon (Fig. 133-10) was first reported by Emerson and coworkers in 1990.36 Several studies of this and related techniques have established important surgical principles (Table 133-1). Five series have been studied—Dallas,33,34 Philadelphia,78 Chicago,17,18,68 St. Louis,11,19 and Los Angeles.12 Three cases with good results have been reported from Omaha.84
These patients were slightly older than the mean for most series of TKAs, but similar to those for revision TKAs. Extensor allografts have been used for disruptions anywhere from the tibial tubercle to the quadriceps tendon, but most have been used for ruptures between the tubercle and patella. Up to 25% of allografts have been used in patellectomy patients, beginning with the first report.18,33,34,78 There is another case of an extensor graft for a patellectomy patient, with a similar but modified technique.65 Extensor allografts are used from 10% to 20% of the time for unhealed patellar fractures with a debilitating lag (and some of the patellectomy patients originated as patellar fractures). Quadriceps tendon ruptures have been treated successfully with extensor mechanism allografts in some series but not attempted in others.
Some series have reported allografting at the time of the primary TKA for concomitant osteoarthritis and chronic extensor rupture,33,34 but most procedures are for failed extensors in primary or revision TKA. Unusual indications include extensor reconstruction when a knee fusion has been converted to a TKA19 and TKA with severe patella infra.17
Infection makes any difficult situation worse, and there is good reason to recommend arthrodesis for an infected arthroplasty without an extensor mechanism. In the most comprehensive report of treating infected TKAs, which included patients revised up until 1994 (the Mayo Clinic experience), did not include the combination of extensor mechanism rupture with sepsis,45 presumably because these patients were not admitted to the treatment protocol. In a state of the art review of treatment for infected TKAs, the same group included the state of the extensor mechanism as one of eight major considerations as to whether reimplantation is reasonable and recommended fusion when the extensor is ruptured and the TKA infected.67
Nonetheless, allograft reconstruction is feasible after prior sepsis. With successful healing of a two-stage reimplantation protocol, Emerson and colleagues33 performed one graft as a third stage. Grafting at the time of reimplantation comprised 17% to 32% of cases in other series.12,18,68 In the largest experience, 2 of 13 patients with an allograft after a two-stage reimplantation became reinfected and proceeded to an above-knee amputation.78
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree