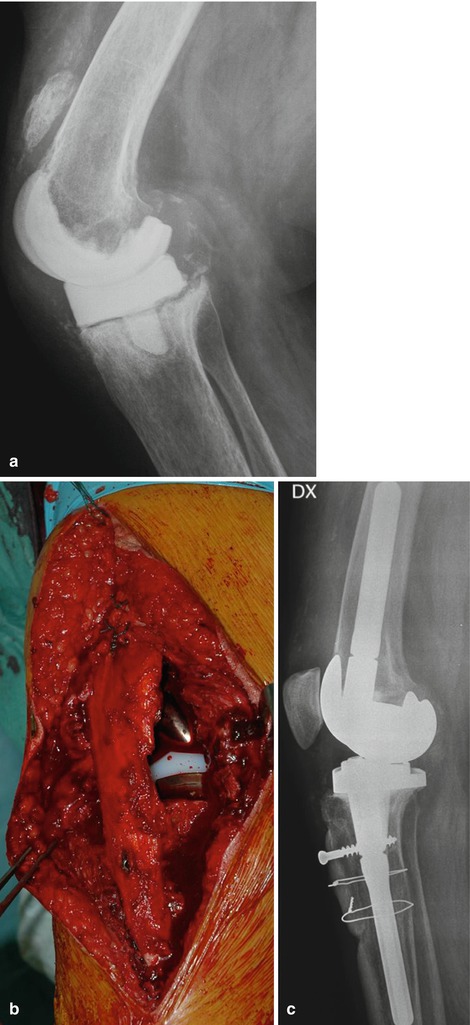
Fig. 58.1
(a, b) Trabecular metal fixed to the cortical remnants of the patella and a dome-shaped polyethylene button is fixed on
Fig. 58.2
Lateral view of a patient after tantalum patella replacement

Fig. 58.3
AP and lateral view of a knee with a linked GSB (Geschwend, Scheier, Bähler) prosthesis (GSB, Allopro, Switzerland) after compound fracture patellectomy was performed
The gull-wing osteotomy [36] may improve congruency to the patellar groove but cannot compensate for the loss of thickness with associated altered quadriceps lever arm (Fig. 58.4.).
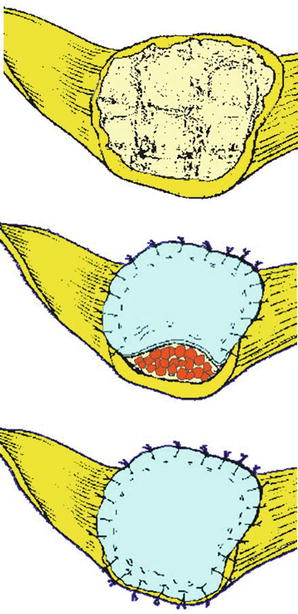
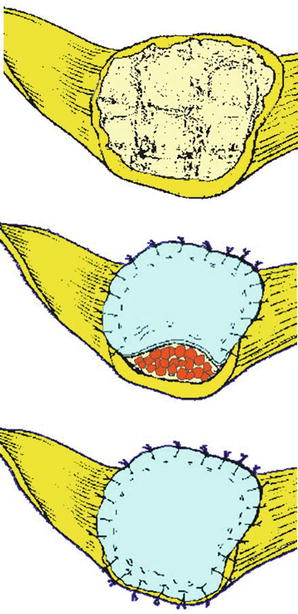
Fig. 58.4
Drawing illustrating the gull-wing osteotomy
The core bone in noninfected patients can now be replaced by porous metal (e.g. trabecular metal®), leading to good midterm results [5].
58.5 Augmentation or Repair of the Patellar Tendon
The use of autologous semitendinosus and gracilis tendons as repair tissue is an excellent procedure for augmentation of the patellar tendon. Both tendons are left attached to the pes anserinus and stripped proximally. A vertical tunnel (diameter 6–8 mm) is drilled through the lower part of the patella and the tibial tubercle. The semitendinosus and gracilis tendons are passed in opposite directions through the tunnels and sutured to each other (Fig. 58.5). The most difficult part is restoring correct patellar position in regard to the femur.
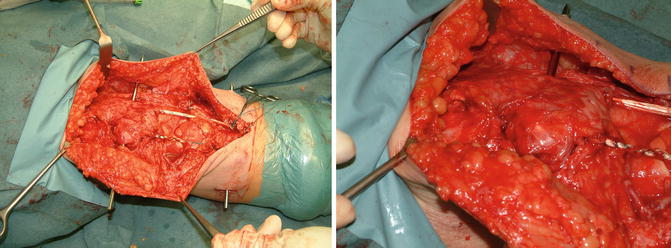
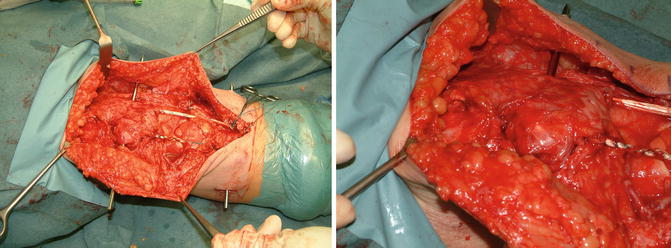
Fig. 58.5
Repair of the patellar tendon and augmentation using a semitendinosus and gracilis tendon autograft. Temporary unloading of the patella and hamstring grafts was achieved by using an external fixator
In case of a primary repair and for temporary protection, an external fixator might be of help. The patient will then be able to walk without restriction, and the knee can be ambulated directly after repair or reconstruction (Fig. 58.6).
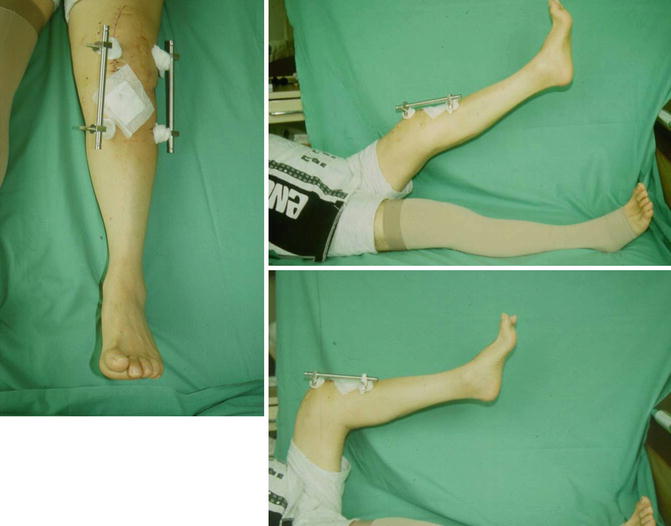
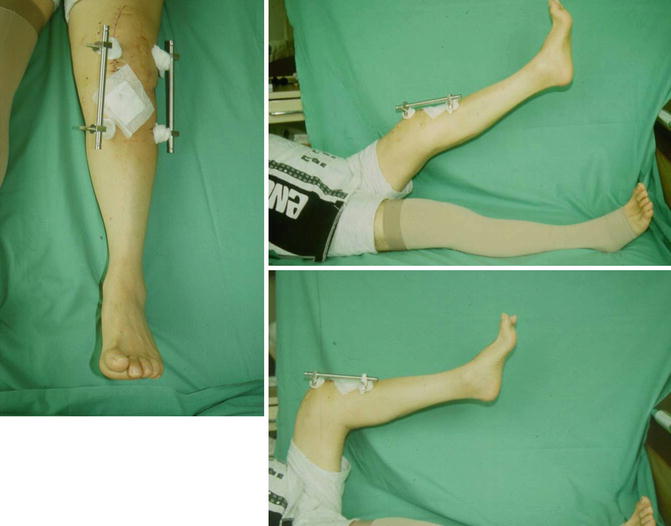
Fig. 58.6
Temporary external fixator to protect the repair of the patellar tendon. This technique allows immediate mobilisation and knee flexion under full weight bearing
58.6 Repair of the Medial Joint Capsule
Medial retinaculum insufficiency or secondary rupture of the capsule may cause patellar subluxation or dislocation (Fig. 58.7). In general, the patellar button then needs to be exchanged (Fig. 58.8a, b). The semitendinosus and/or gracilis tendon can be used for stabilising the patella due to the reconstruction of the medial patellofemoral ligament (MPFL) and the medial capsule. The MPFL was found to be the major restraint to prevent lateral displacement of the patella and contributes 53 % of the total force [40]. It has been shown that the MPFL has the largest effect from 0° to 20° of knee flexion regarding passive patellar stabilisation before diving into the trochlear groove [41]. The reconstruction of the MPFL should be performed only when femoral component malrotation has been excluded. The tendon is fixed at the upper pole of the patella using two 3.5 mm suture anchors (Fig. 58.9). An imaging intensifier should be used to identify the insertion site at the adductor tibial tubercle (Fig. 58.10a, b) [42]. The femoral insertion is slightly anterior to the posterior cortical line and between the two perpendicular lines drawn through the most posterior point of the Blumensaat line and the intersection between the dorsal femoral condyle and the posterior femoral cortex. Interference screw fixation is performed on the femoral side. The quadriceps tendon can be used as an alternative graft option. A 1 cm wide, 3 mm thick and 10 cm long quadriceps tendon strip is harvested. The strip should remain attached to the patella. Finally, the free end is fixed to the femoral insertion site using an interference screw.
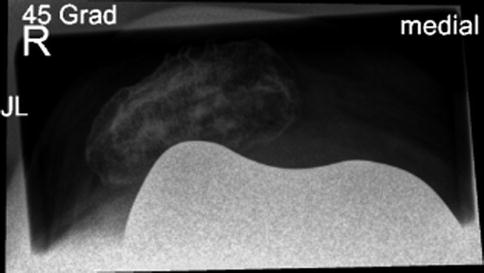


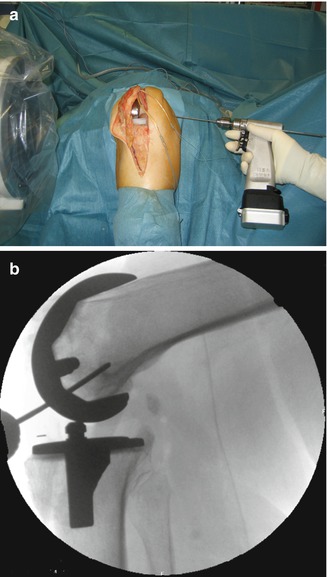
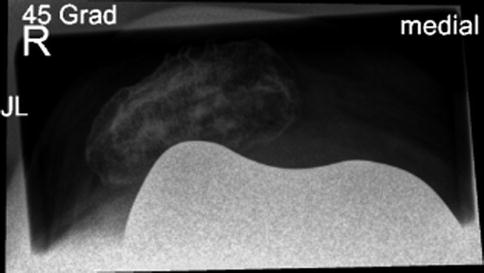
Fig. 58.7
Merchant’s view of a patient with a patellar subluxation after TKR. The patella rides over the lateral condyle of the femoral component

Fig. 58.8
Damage to the patellar button caused by patellar maltracking. The patella was running over the lateral femoral condyle. (a) Shows the button and (b) the button still in place

Fig. 58.9
Reconstruction of the medial patellofemoral ligament using the gracilis tendon. The tendon is already fixed in a groove created at the upper pole of the medial patella
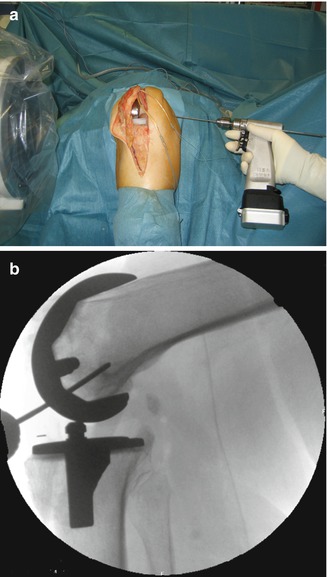
Fig. 58.10
Position of the femoral insertion site of the MPFL by using the imaging intensifier. The insertion point is identified and a blind canal 5 mm in diameter and 30 mm in length is drilled. MPFL medial patella femoral ligament
58.7 Restoration of the Extensor Apparatus
Severe cases may require allogenic transplants in order to replace the extensor apparatus from the quadriceps tendon down to the patellar tendon. These salvage procedures for the extensor mechanism have shown acceptable results, ranging from moderate to excellent [20, 24, 25, 27, 28, 43–47].
In most of the cases, a degeneration of the tendinous or osseous portions of the extensor mechanism was present before the actual traumatic or iatrogenic injury. For this reason, it is often problematic to repair such lesions with direct suturing. The deficient quadriceps or patellar tendon requires reinforcement or replacement by tendon grafts. Emerson et al. described an alternative technique using a complete extensor mechanism allograft (EMA) in 1990 [26] (Fig. 58.11a, b). A few years later, Crosset et al. [25] reported a successful technique for extensor mechanism repair using an Achilles tendon allograft (ATA) (Fig. 58.12).
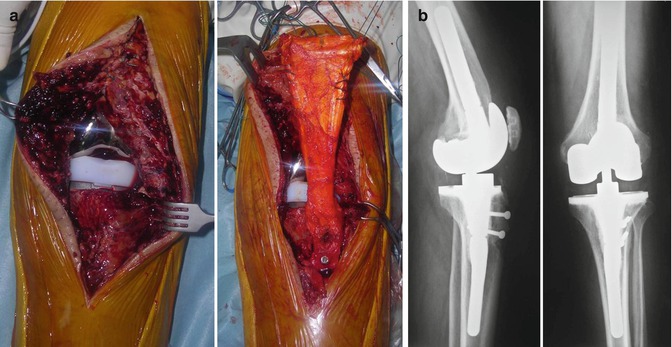

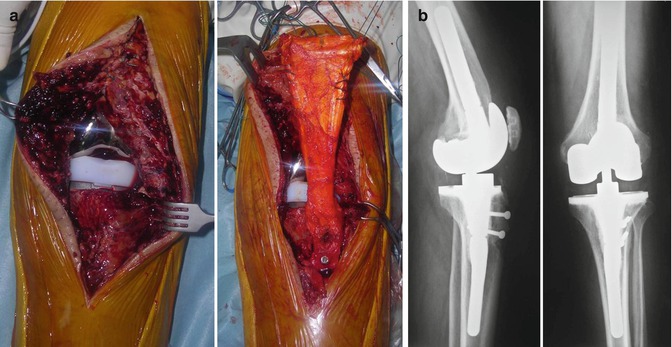
Fig. 58.11
Patellar tendon rupture after revision TKR in an otherwise well-functioning implant (left). Extensor mechanism reconstruction using an Achilles tendon allograft (right) (a). AP and lateral views at 5 years follow-up after Achilles tendon allograft (b)

Fig. 58.12
The two common types of allografts used for extensor mechanism reconstruction. On the left a total extensor mechanism allograft which includes the tibial tubercle (minimum required length: 6 cm), the patellar tendon, the patellar bone and the quadriceps tendon (minimum required length 6 cm). On the right an Achilles tendon allograft (minimum required length: 20 cm) with the calcaneus bone block (minimum required diameter: 4 cm)
The use of EMA is recommended in proximal (quadriceps) lesions, in extensive defects, in a patient older than 70 years or when the patella has been replaced already (Fig. 54.13a, b). The ATA technique is used when there is a lesion of the patellar tendon in a patient younger than 70 years (in order to use tissue from the host as much as possible) and without patellar resurfacing. A solid distal fixation of the graft (tubercle or calcaneus) with medullary screws and or wires is of paramount importance for the reconstruction technique. Proximal fixation is performed in full extension using both no. 5 and 2 nonabsorbable sutures. Immobilisation in a brace or cast (depending on patient compliance) in full extension should be maintained for at least 6 weeks.
If the extensor mechanism problem cannot be solved completely, a constrained revision TKR (rotating hinge) has to be carefully considered. This solution will limit the subsequent risk of sagittal instability and/or knee dislocation. However, even with a hinged implant, the extensor apparatus should be restored whenever possible in order to avoid mechanical implant failure such as loosening, dislocation, hinge buckle ruptures and bone fractures around the stem extensions. Forty-two extensor mechanism reconstructions in patients with TKR have been performed since 2005 in the author’s own series (AB). Indications for the reconstruction of the 37 patients were chronic rupture of the patellar tendon (53 % of the cases), quadriceps tendon (22 %), patellar fracture (8 %) or a combined patellar and quadriceps rupture (17 %). In an additional five patients, an extensor mechanism allograft procedure was performed, not because of a rupture but because of recurrent ankylosis after multiple procedures with nonfunctional calcified extensor mechanism. In this series, we employed an EMA in 25 cases, an ATA in 8 cases, an artificial tendon in 2 cases and a hernia mesh in 2 cases. The artificial tendons and the hernia mesh were used in salvage procedures when unexpected insufficiency was found during revision TKR and allograft was not available. This may happen, for instance, after revising an infected TKR treated with a static spacer where the extensor mechanism function cannot be assessed. The average time from extensor mechanism disruption to surgery was 10 months (range 1–120 months). At a mean follow-up of 40 months (range 6–96 months), all patients were community ambulators. The average postoperative maximum flexion was 106° (80–130°) for the ruptured group and 70° (50–90) for the ankylosed group. All patients thought their functional status had improved, and 70 % were very satisfied, 17 % were satisfied, and 13 % were not satisfied (this represented 3 of the 5 patients who sustained postoperative complications) with the results of the allograft reconstruction. All patients presented an extensor lag of more than 30° prior to surgery. The extensor lag was reduced to 3.5° ± 4.5° after surgery. The majority of the patients did not show any extensor lag (excluding the 5 patients with complications). Nine patients had lag up to 10°; only 2 patients had lag over 10°. There were 5 complications in this cohort. One patient had a recurrence of infection after the two-stage reconstruction (of the total 14 infected TKR cases treated in this cohort) with the allograft. This patient was already a “two-time” loser; for this reason, we decided to perform a revision with arthrodesis. Three cases had failure of the tibial tuberosity with patellar tendon graft avulsions. Two of them were successfully revised with another allograft (one patient is waiting for the revision procedure). One patient had a failure of the hernia mesh with recurrent lag. He was successfully revised with an EMA.
Five additional patients received operation because of an ankylosed knee after several failed surgeries. Of the patients treated with EMA and TKR revision for ankylosis, two were able to reach 90° of flexion (very satisfied), one reached 60° of flexion (moderately satisfied) and two had a recurrence of arthrofibrosis with very limited motion (unsatisfied).
58.8 Artificial Material for Augmentation
Different artificial products are available for augmentation of the extensor apparatus in order to provide primary stability, such as Mersilene tape, Leeds-Keio ligament (Neoligaments®, Leeds, UK), Dacron or the LARS (Ligament Augmentation and Reconstruction System – Arc-sur-Tille, France), which is composed of polyester material. The LARS ligament can be used for complete augmentation of the extensor mechanism including quadriceps tendon and the patellar tendon (Fig. 58.13). Good and excellent results have been reported in 56 % and some degree of extensor lag in tumour patients [31] (Fig. 58.14). The Leeds-Keio ligament was initially designed for ACL reconstruction [48].