Extensively Porous-Coated Cylindrical Uncemented Femoral Stems
Scott M. Sporer
INDICATIONS
Despite the overwhelming success and long-term reliability of total hip arthroplasty, several situations necessitate the revision of a femoral component. The most frequent indications for femoral revision include aseptic loosening, recurrent instability from a malpositioned component, component fracture, periprosthetic fracture, delayed infection, and the need for improved acetabular exposure. Relative indications for femoral component removal include progressive distal femoral osteolysis or revision of a femoral component with a poor track record encountered during acetabular revision.
A successful surgical result following femoral reconstruction requires the extraction of the previous component with minimal bone loss, the insertion of a new component with resistance against rotational and axial stresses, and a stable articulation following reduction. The use of an extended trochanteric osteotomy is often recommended to extract a well-fixed stem, to insert a femoral component into a femur that has exhibited varus remodeling, or to facilitate the removal of distal cement. This surgical technique allows preservation of proximal bone stock and allows concentric reaming of the remaining isthmic femur.
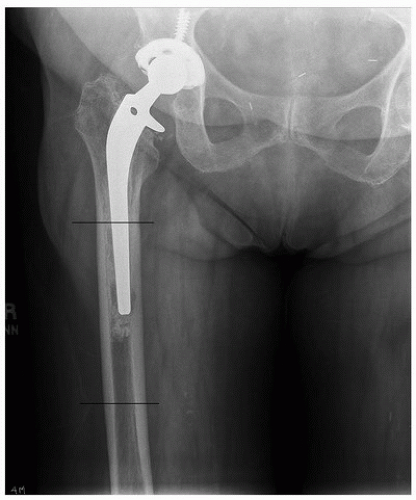
The type of femoral component utilized during revision surgery ultimately depends on the quality of remaining host bone. The femoral defect classification of Paprosky et al. is helpful in preoperative planning and in assisting the surgeon with reconstructive options (Table 27-1) (1). The majority of femoral revisions encountered in daily practice have an intact diaphyseal segment with a compromised metaphyseal region (Paprosky type II) (Fig. 27-1) or more severe involvement of the proximal diaphysis (Paprosky type IIIA) (Fig. 27-2). In these patients, the metaphyseal region cannot be relied upon to provide stable component fixation. High failure rates have been observed when metaphyseal fixation has been attempted in this patient population (2). It is the author’s preference to always use an implant that obtains distal fixation for type II and greater defects.
Distal fixation can be achieved through either a cemented or cementless implant. A cementless implant is recommended in the majority of patients due to the high rate of osseointegration and long-term clinical results. There are two philosophies regarding the optimal distal femoral geometry
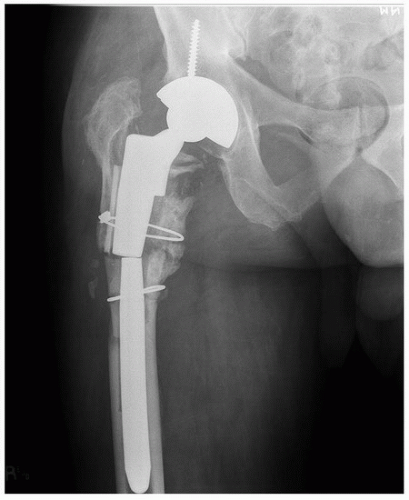
in order to obtain distal femoral fixation. A tapered stem with splines will obtain axial stability through the tapered distal segment, while the splines will provide rotational stability (Fig. 27-3). An extensively fully porous-coated cylindrical stem relies upon a press fit between the distal portion of the cylindrical stem and the reamed diaphyseal bone (Fig. 27-4). Excellent clinical results have been observed with both modular and nonmodular tapered as well as extensively coated cylindrical stems.
Diaphyseal fixation with a monoblock extensively coated cylindrical stem remains the authors preferred implant choice in Paprosky type II and IIIA defects. A monoblock extensively porous-coated cylindrical stem avoids the potential for modular junction fractures (Fig. 27-5) and, unlike a tapered stem design, allows the ability to use a trephine to remove the distal segment of a well-fixed stem should extraction be required in the future.
in order to obtain distal femoral fixation. A tapered stem with splines will obtain axial stability through the tapered distal segment, while the splines will provide rotational stability (Fig. 27-3). An extensively fully porous-coated cylindrical stem relies upon a press fit between the distal portion of the cylindrical stem and the reamed diaphyseal bone (Fig. 27-4). Excellent clinical results have been observed with both modular and nonmodular tapered as well as extensively coated cylindrical stems.
Diaphyseal fixation with a monoblock extensively coated cylindrical stem remains the authors preferred implant choice in Paprosky type II and IIIA defects. A monoblock extensively porous-coated cylindrical stem avoids the potential for modular junction fractures (Fig. 27-5) and, unlike a tapered stem design, allows the ability to use a trephine to remove the distal segment of a well-fixed stem should extraction be required in the future.
TABLE 27-1 Paprosky Classification | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 FIGURE 27-2 AP femur radiograph demonstrating a Paprosky type IIIA femoral defect. Note that greater than 5 cm of diaphyseal bone remain available to achieve implant stability. |
 FIGURE 27-3 The distal splined tapered stem of a modular revision hip system. Note the splines that provide rotational stability while the taper provides axial stability. |
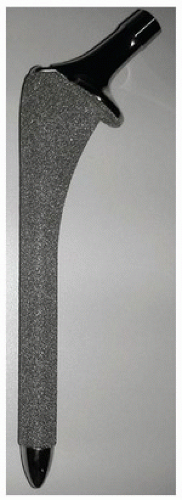 FIGURE 27-4 An extensively porous-coated cylindrical stem. Note the cylindrical porous coating relies upon a scratch fit in order to obtain axial and rotational stability. |
CONTRAINDICATIONS
Extensively porous-coated cylindrical stems rely upon the interference “press fit” between the remaining host diaphysis and the femoral component. It has been suggested that a minimum of 4 to 5 cm of diaphyseal bone be available and engaged by the extensively porous-coated cylindrical implant in order to provide adequate rotational and axial stability to minimize micromotion and to facilitate bone ingrowth (3). The authors recommend alternative reconstructive options when there is less than 5 cm of diaphyseal bone remaining (Paprosky type IIIB or IV defect) or when the patient has compromised biologic activity such as a tumor or radiation that would prevent bone ingrowth. Additionally, patients with a type IIIA or IIIB femur (Fig. 27-6) and an associated endosteal diameter greater than 19 mm have been shown to have a higher incidence of subsidence and a decreased likelihood of achieving boney ingrowth (4). In these patients, age, medical comorbidities, and activity level are important factors to consider when choosing a femoral component. A modular tapered stem can be used successfully in the majority of these large femoral defects (5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree