Exercise is frequently used to enhance the recovery rate of all components of the movement control system, namely the musculoskeletal and central nervous system (CNS), to increase the range of motion, increase muscle strength, develop a higher level of proprioceptive feedback and develop an overall improvement in sensori-motor control. However, the list of benefits does not end here; exercise is used in rehabilitation of the cardiovascular and pulmonary systems (Rees et al. 2004), which are required to provide the raw fuels for the physiological processes involved in muscle contraction. Also, exercise has been shown to have beneficial effects on the higher centres, reducing the effects of some mental illnesses (Galper et al. 2006). This explains its invaluable use in this area of healthcare. Therapists commonly employ several types of strengthening exercise Muscle strength can be evaluated in a number of ways: manually, functionally or mechanically. The Oxford scale has been devised to manually assess muscle strength and is widely used by physiotherapists. According to the Oxford scale, muscle strength is graded 0 to 5. Table 13.1 summarises the grades. Table 13.1 There are limitations to the usefulness of the Oxford scale. These include: • a lack of functional relevance; • non-linearity (the difference between grades 3 and 4 is not necessarily the same as the difference between grades 4 and 5); • a patient’s variability with time (alternating between grades owing to fatigue, for instance); • a degree of subjectivity between assessors; • assessment of muscles acting only concentrically; • the difficulty of applying the scale to all cases in clinical practice (so that strength is rarely evaluated throughout full range as many individuals seen by physiotherapists do not possess full range in the first place). Isokinetic assessment has been used with increasing frequency since its inception in the 1970s. It involves the use of computerised evaluation of movement when exercising at a preset angular velocity on the isokinetic equipment (Figure 13.1). Additional limitations have been acknowledged by Lieber (1992). These include the time required to recruit muscle fibres (50–200 ms), making this period of data obtained unusable. Another drawback is the limb striking the testing bar at the end of the movement, although some isokinetic units employ a damping mechanism to prevent this. • increased cross-sectional area of muscle; • increased muscle fibre size; • increased or maintained bone density; • increased tensile strength of tendons and ligaments; Muscles can contract in three different ways: concentrically, eccentrically and isometrically. The characteristics of these different types of contractions are summarised in Table 13.2. Table 13.2 Individual muscles often exhibit more than one type of contraction at a time. Consider the muscle work occurring in the hamstring muscles in Figure 13.2. The features of eccentric exercise when compared with concentric exercise are, on the positive side, that it is mechanically more efficient and metabolically more efficient, but, on the negative side, it is less resistant to fatigue and may result in DOMS micro-trauma inflammation between sarcomeres. See Table 13.3 for further examples of eccentric activity. Table 13.3 The functions of eccentric muscle work DOMS is typically felt most acutely 48 hours after eccentric exercise has been completed (Howell et al. 1993; Rodenberg et al. 1993; Leger and Milner 2001). This commonly occurs in certain muscles of individuals undertaking a particular activity infrequently that has quite a high eccentric component. Examples include fell running (quadriceps in the downhill component) or playing squash (gluteus maximus when reaching for a low shot). DOMS is effectively the occurrence of local micro-trauma within the muscle. A key site for this inflammation is between adjacent sarcomeres or within the Z bands. Evidence for this inflammatory reaction can be found in increased levels of creatine kinase (CK) in the blood following exercise. This enzyme is released into the bloodstream following a muscular injury. Occasionally, the high CK levels found following eccentric exercise can confuse the clinical picture of a patient in whom CK levels may be used as a means of informing clinical diagnosis (Gralton et al. 1998). Saxton et al. (1995) have also reported a decrease in proprioceptive function with high-level eccentric exercise. Despite many suggestions of dietary, medicinal, massage and exercise remedies there is conflicting evidence as to how best to enhance recovery from DOMS (Bennett et al. 2005; Close et al. 2005; Racette et al. 2005; Rahnama et al. 2005). Eccentric exercise has been identified as a key treatment technique when rehabilitating tendon injuries, such as in the tendo-achilles. Stanish et al. (1985) proposed treatment protocols with eccentric exercise involving alteration in both load and speed. The benefits of using eccentric exercise programmes for tendon injuries are thought to include: • enhancing muscle strength to improve movement efficiency in the musculo-tendinous complex; • increasing the tensile strength of the tendon; • stressing healing tissue in a functional manner to influence collagen deposition; Knowledge of the types of contraction whether eccentric, concentric or isometric, is required when planning strengthening exercises. Eccentric contractions are capable of producing more torque than isometric, which, in turn, are stronger than concentric contractions. Isometric exercises are particularly useful when an area is immobilised, for instance when a joint is immobilised in Plaster of Paris, provided the contraction does not further damage soft tissues or destabilise fracture sites as active movement would be more likely to. It is useful to apply eccentric and concentric exercises in a functional context during rehabilitation. The functions of eccentric exercise being the deceleration of limb part, for example hamstrings braking knee extension when kicking a football, the absorption of force, for example when landing from a jump, or controlling a movement with the recoil of resistance or with gravity, for example during sit to stand (Figure 13.3). The following are some of the proposed benefits of closed chain exercises in the lower limb: • the shear force acting at the knee joint is reduced compared with the last 30 degrees of open chain extension (Wilk et al. 1996); • they encourage more functional movement patterns; • they stimulate co-contraction of the hamstrings, helping to reduce anterior tibial translation (important in ACL rehabilitation); • they increase shoulder stability in the upper limb by stimulating co-contraction of surrounding muscles of the glenohumeral joint and scapula-thoracic articulation. There are three main types of muscle fibre, usually called I, IIa and IIb, but newer subdivisions are now being described, such as Ic, IIc and IIab (Scott et al. 2001). Individual muscles are composed from all types, but have different proportions of each. Some of the differences in the physiological make-up of these muscle fibres are illustrated in Table 13.4. Table 13.4 Some characteristics of the muscle fibre types The exact proportion of different fibre types is not consistent between muscles or between individuals. These characteristics are generally thought to be partly genetically determined and are part of the reason for the natural selection that sees individuals excel in different sports or play in different positions within a team. They are also influenced by training applied to the muscle (Scott et al. 2001). However, some general points can be made. • Postural muscles such as the soleus are involved in maintaining position rather than dynamic activity and therefore have a higher number of type I fibres. • Muscles that may be involved in more dynamic activity, such as the gastrocnemius, will have proportionately greater numbers of fast twitch fibres – types IIa and IIb. • With age, the number and size of type II fibres decreases (Rogers and Evans 1993), making tasks that require a quick burst of strength more difficult. This should be an important consideration when rehabilitating elderly patients. • There is evidence that muscle fibres can convert from one fibre type to another. This occurs between types IIa and IIb (Scott et al. 2001) in particular and is known as plasticity. The majority of protocols that are in existence for strength training are based upon what are known as the ‘one repetition maximum’ (1RM) and the ‘ten repetition maximum’ (10RM). The 1RM is the weight that can be lifted once and only once in an exercise, with further completed effort being prevented by fatigue (Cahill et al. 1997). Determining the 1RM therefore prevents a challenge in the clinical environment and perhaps explains the sometimes arbitrary nature of repetitions given. The 10 RM is calculated similarly, i.e. the weight that can be lifted ten times. Once the 1RM or 10RM are established, weight training protocols can be calculated using percentages of this figure. Mobilising exercises are a fundamental component of the rehabilitation process as they enhance normal tissue healing and are necessary to load the soft tissues progressively. Ultimately, the resultant scar tissue is stronger (Melis et al. 2002) and this enables it to more effectively withstand the stresses and strains it encounters during normal functional use (Hunter 1998). For the purposes of this chapter, exercises are divided into the following classes: Passive exercises can be defined as exercises by which movement is produced entirely by an external force with the absence of voluntary muscle activity on behalf of the patient. This external force may be supplied by the therapist (as is the case with passive movements) or by a machine. For example, continuous passive motion (CPM) units might be used following total knee arthroplasty or other knee surgical procedures, or in stroke rehabilitation (Lynch et al. 2005) to enhance recovery of the shoulder. If performed appropriately, stretching exercises may be a simple, yet very effective, form of treatment. For example, in the elderly a loss of hip extension during walking implies the presence of functionally significant hip flexor tightness (Kerrigan et al. 2001) and predisposes individuals to falls and subsequent femoral neck fractures. Overcoming hip tightness with specific stretching exercises as a simple intervention shows some improvement in walking performance and possibly fall prevention in the elderly (Kerrigan et al. 2003). Stretching is commonly employed within the athletic population. Increasing the range of motion available at a joint has obvious advantages in increasing function and performance. It is suggested that regular stretching improves force, jump height and speed, although there is no evidence that it improves running economy (Shrier 2004). It has also been suggested that it contributes to injury prevention, although research does not suggest that stretching reduces risk of injury or reduces the effects of DOMS at present (Herbert and Gabriel 2002). Stretching exercises are performed with the target structure moving towards a lengthened position. The stretching exercise will involve further movement in this direction so as to further lengthen the structure. Collagen fibres realign rapidly as a result of stretching forces and become aligned (and therefore stronger) in the direction of the stretching force (Melis et al. 2002). The limiting factors to further movement, such as the degree of pain experienced, will govern the extent to which any further movement is possible. Stretches are commonly used to increase range of movement by mobilising restrictions within soft tissue (e.g. scar tissue) and are specifically used in the lengthening of tight muscles. The time at which stretching is commenced after an injury needs careful consideration. After any soft tissue injury, the length of the immobilisation depends on the grade of injury and must be optimised so that the scar can withstand the longitudinal forces operating on it without re-rupture. Mobilisation of soft tissues by stretching will aid reabsorption of the connective tissue scar and recapillarisation of the damaged area (Kujala et al. 1997). Stretching may also be used as a preventative measure, for example to prevent joint contractures. However, while the primary intervention for the treatment and prevention of contracture is to regularly stretch the soft tissues, and the rationale behind this intervention appears sound, the effectiveness of stretching has not been verified with well-designed clinical trials on subjects who have sustained soft tissue injury (Shrier and Gossall 2000). One such trial (Malliarapolous et al. 2004) looked at the frequency of stretching protocols in athletes with hamstring injuries and found a significant difference in rate of recovery when the protocol was applied three times daily compared with once a day. However, a lack of control group limits our insight into the effectiveness of this modality and a lack of longer-term surveillance limits insight into its effect on reinjury rates. Stretches may be applied in one of two ways: either dynamically or statically (Table 13.5). Table 13.5 Stretching exercises: A summary
Exercise in rehabilitation
Introduction
Strengthening exercises
Introduction
Measurement of muscle strength
The Oxford scale
Grade
Muscle contraction
0
No contraction
1
Flicker of a contraction
2
Full-range active movement with gravity eliminated (counterbalanced)
3
Full-range active movement against gravity
4
Full-range active movement against light resistance
5
Normal function/full-range against strong resistance
Isokinetic assessment

Drawbacks
Strength training
Benefits
Free active exercise
Muscle contractions
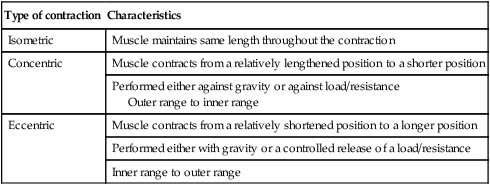
Type of contraction
Characteristics
Isometric
Muscle maintains same length throughout the contraction
Concentric
Muscle contracts from a relatively lengthened position to a shorter position
Performed either against gravity or against load/resistance
Outer range to inner range
Eccentric
Muscle contracts from a relatively shortened position to a longer position
Performed either with gravity or a controlled release of a load/resistance
Inner range to outer range

Function
Example
Deceleration of a limb part
Kicking a football: the hamstrings act to decelerate hip flexion and knee extension
Force absorption
Landing from a jump: the quadriceps contract absorbing some of the ground reaction force thus reducing the joint reaction forces
Controlling a movement against gravity
Sitting down in a chair: gluteus maximus and the upper part of the hamstrings are controlling hip flexion
Treatment with eccentric exercise

Open-chain and closed-chain kinetic strengthening
Resisted exercise
Types of muscle fibre
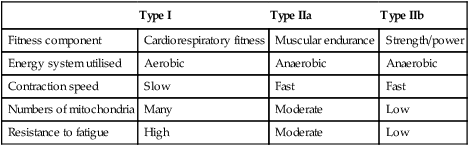
Type I
Type IIa
Type IIb
Fitness component
Cardiorespiratory fitness
Muscular endurance
Strength/power
Energy system utilised
Aerobic
Anaerobic
Anaerobic
Contraction speed
Slow
Fast
Fast
Numbers of mitochondria
Many
Moderate
Low
Resistance to fatigue
High
Moderate
Low
Number of repetitions
Mobilising exercises
Introduction
Classes of mobilising exercise
Passive exercises
Stretching exercises
Dynamic stretch
Static stretch
Feature of stretch technique
Faster, rhythmic, higher velocity, motor control, functional
Slow, controlled, emphasis on postural awareness, bodily alignment
Duration of stretch
Repetitive, progressive
Sustained 30-second hold
Stage employed
End-stage rehabilitation
Early, middle and end-stage rehabilitation
Training motor patterning
Client types
Sportsmen, active persons
All ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




