Injuries to the hip and pelvis are the least common of lower extremity injuries in youth sports, but include many of the more serious conditions. This article describes the bone and soft-tissue conditions of the hip and pelvis that may present to health care providers caring for the pediatric and adolescent sporting population. The article discusses epidemiology, mechanisms, clinical presentation, evaluation, and treatment options.
Injuries to the hip and pelvis are the least common of lower extremity injuries in youth sports, but include many of the more serious conditions . This article describes the bone and soft-tissue conditions of the hip and pelvis that may present to health care providers caring for the pediatric and adolescent sporting population. The article discusses epidemiology, mechanisms, clinical presentation, evaluation, and treatment options.
Bone development of the hip
The acetabulum and femur start development intrauterine at 6 weeks . The acetabulum begins as a shallow depression from bony precursor cells that eventually form the pubis, ilium, and schium of the pelvis. Other cells grow to start the formation of the proximal, central, and distal aspects of the femur. By week 8, the primary ossification centers of the femur appear with development of the surrounding soft tissue and internal rotation of the limb. At this time, development begins in the arterial supply of the proximal femur. By 12 to 14 weeks, the acetabulum develops a series of blood vessels while a network of vessels forms around the femoral neck. Hip growth and maturation continue for the next 20 weeks.
After birth, the acetabulum and femur undergo formation of secondary ossification centers at different stages. Initially, the acetabular bone is a cartilaginous complex that eventually forms ossification centers by age 8 to 9 years . The femoral shaft ossification center starts developing during the first year of life. During the first 3 years, the femoral head is slightly larger in its anterior-posterior length than in its transverse length. However, by age 3, it will become more spherical in nature. From birth to eventual physeal closure, the blood supply will be limited by the ability of the various vessels to supply the femoral head across the growth plate.
Throughout childhood and early adolescence, the underlying acetabulum, femoral bone, and pelvis continue to develop. Various apohyses appear, mostly occurring from ages 13 to 15 years ( Table 1 ). During this time, the underlying bone is weaker at the apohyseal joint compared with the surrounding tendons, ligaments, and muscles. Any excessive contraction of the muscles or stretching on the ligaments is more likely to lead to separation of the apophysis rather than tearing of the tendon or muscle . Fusion of the femoral complex and acetabulum with the ilium, ischium, and pubis is mostly completed by 16 to 18 years of age.
| Apophysis | Appearance (y) | Fusion (y) | Related muscle group(s) |
|---|---|---|---|
| AIIS | 13–15 | 16–18 | Quadriceps |
| ASIS | 13–15 | 21–25 | Sartorious |
| Lesser trochanter | 11–12 | 16–17 | Iliopsoas |
| Greater trochanter | 2–3 | 16–17 | Gluteal |
| Ischial tuberosity | 13–15 | 20–25 | Hamstrings |
| Iliac crest | 13–15 | 21–25 | Abdominal obliques |
| Latissimus dorsi |
Bone conditions
Apophyseal injuries: anterior inferior iliac spine, iliac crest
Apophyseal avulsion injuries occur in skeletally immature athletes because of the inherent weakness across the open apophysis . Incidence is increasing, especially in the 14- to 17-year-old age group as a result of increased participation in competitive sports . An apophysis is a bony growth center (physis) where tendon attaches to bone. Until skeletal maturation is reached, the tendon attached to the site is stronger than the connection between the apophysis and the underlying bone . Because of this biomechanical weakness, forceful contraction of the muscle results in separation of the epiphyseal plate (referred to as an avulsion fracture). Once the skeleton is mature, the physes are fused and thus stronger than the muscle or tendon, making apophyseal injuries obsolete. The same muscle contraction that causes apophyseal avulsion in adolescents causes tendon or muscle tears in adults. Though avulsion fractures can occur at any major muscle attachment, the most common sites are the sartorius attachment at the anterior superior iliac spine, the rectus femoris attachment at the anterior inferior iliac spine, and the hamstring attachment at the ischial tuberosity.
Patients present with a history of activity-induced acute-onset pain, often accompanied with an audible pop or snap . The injuries often occur during sports involving explosive or burst types of movement, such as American football, dance, soccer, and gymnastics. The patient characteristically assumes a position that minimizes stretch of the associated muscle . Physical examination reveals tenderness and possibly swelling at the region overlying the apophysis, pain with passive stretch of the associated muscle group, and often pain with resisted contraction of the affected muscle.
Plain radiographs show a pathologic widening of the physis and the avulsed bone. Though the diagnosis is often made clinically, radiographs are helpful in determining the size of the avulsed fragment and the degree of bony displacement . Treatment includes rest, ice, and protected weight-bearing with crutches for pain-free ambulation. Casting or bracing is not needed. Once the patient can ambulate without pain, a simple program of therapeutic exercise with a goal of stretching and strengthening the affected muscles. Low-impact activities, such as cycling, elliptic training, and swimming, can be initiated at this time as well. This is followed by a gradual return to running with progression to cutting, sprinting, and jumping . Once these activities can be done without pain in a controlled environment, the patient can return to practice and eventually to competition. Follow-up radiographs are not required unless symptoms continue to limit activities. Surgical intervention is rare and is reserved for cases with significant ongoing symptoms. Surgery may also be indicated when there is a large fragment with greater than 2-cm displacement, though optimal timing for surgical intervention remains debatable . There are no significant potential complications other than prolonged healing time and persistent symptoms.
Hip dislocation
Pediatric hip dislocation is relatively rare. Most cases are posterior dislocations. Low-energy dislocations (resulting from sporting or playing activities or from a fall from less than 10 ft) account for roughly 65% of posterior pediatric hip dislocations, with high-energy dislocations (resulting from a motor vehicle accident or fall from greater than 10 ft) accounting for the remaining 35% . Posterior dislocations can occur when someone falls on top of a kneeling player .
Standard radiographs are the preferred initial imaging studies. Additionally, CT scan can be done to evaluate for fracture not seen on radiograph if there is high clinical suspicion or in cases where there is persistent or suspected posterior joint instability .
Closed reduction under conscious sedation or, less commonly, general anesthesia is the initial treatment. Occasionally, additional open reduction may be indicated if there are associated intra-articular fracture fragments or interposed soft tissue . After a closed reduction, traction followed by mobilization and protected weight-bearing with crutches for 6 weeks is often used. An alternative postreduction course involves 6 weeks of using a spica cast followed by protected weight-bearing with crutches . Physical therapy may be prescribed to focus initially on range of motion, progressing to strengthening and gait-training as weight-bearing restrictions are removed.
The vast majority of patients have full recovery without residual pain or limitation in sporting activities. Some experience mild aching with changes in the weather or a mild limp. Very few have moderate or severe pain or limp (approximately 5%) . In a retrospective study of pediatric hip dislocations , the most common complications were associated fractures (17%) and avascular necrosis (12%). Associated fractures can include the posterior wall acetabulum or femoral head osteochondral, and occur almost exclusively in high-energy dislocations. Avascular necrosis of the femoral head can become evident on radiographs as soon as 2 months following dislocation. It is associated with prolonged time to reduction (greater than 6 hours) and does not appear to be associated with patient age, energy level of the dislocation, or the associated fracture. Persistent asymmetry postreduction can be due to soft-tissue interposition of a torn labrum, including lateral acetabular apophysis trapped within the joint . Other potential complications include coxa magna, heterotopic ossification, and recurrent dislocation.
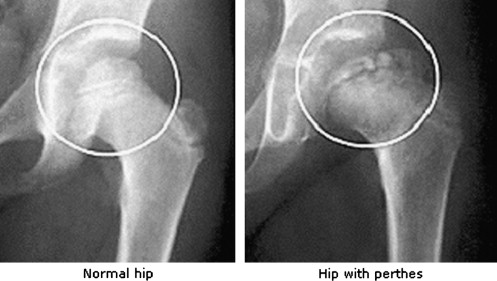
Legg-Calvé-Perthes disease
Legg-Calvé-Perthes disease comes on in the first decade, predominates in boys ages 4 to 8 years, and has a male/female ratio of 5:15 . Bilateral cases occur in 8% to 24% of cases . Literature is conflicting on potential causes of Legg-Calvé-Perthes disease. Most agree that the predominant cause is hypovascularity due to repetitive vascular injuries, though the underlying mechanism causing vascular insufficiency is still debated. Hypotheses center on thrombophillic mechanisms or transient elevations in intracapsular pressure. Pathology of this disease is complex, involving idiopathic self-limiting avascular necrosis of the femoral head . Following the necrosis, there is resorption, collapse, and subsequent remodeling repair. More complete remodeling, which can be influenced with treatment, occurs more often in children with earlier presentation because of greater time for growth and remodeling before reaching skeletal maturity .
Patients present with insidious-onset painless limp, usually affecting only one leg. If pain is present, it is usually mild, exacerbated with exercise, and often referred to the knee . Limitations of internal rotation and abduction are seen on physical examination. These limitations can be caused by either muscle spasm or synovitis in early stages and by bony impingement in later stages .
There are several classification systems used. Most widely used is the Herring lateral pillar classification system, which uses anteroposterior radiographs to determine the degree of involvement of the lateral portion of the femoral head. Group A hips have no involvement of the lateral pillar, meaning no density changes or loss of height in the lateral third of the femoral head (lateral pillar). Group B hips have some lucency in the lateral pillar and up to 50% of height loss. Group C hips have more lucency and greater than 50% height loss . The Stulberg classification uses the shape of the femoral head to delineate between groups. Class I hips are normal. Class II hips have spherical, larger than normal femoral heads, shorter femoral necks, or abnormally steep acetabulae. Class III hips have heads that are nonspherical (ovoid, mushroom-shaped, or umbrella-shaped) but not flat. Class IV hips have flat heads and acetabulae . The Caterall classification based on percent involvement of the epiphysis (25%, 50%, 75%, or 100%) is now infrequently used.
Plain radiographs are usually sufficient for diagnosis ( Fig. 1 ). Treatment can be nonoperative (bracing) or operative (osteotomy). A large multicenter study has shown that in children up to 8 years of age who present with lateral pillar group B hips have similar favorable outcomes whether treated operatively or nonoperatively. However, children over 8 years old with presentation in group B or B/C border had statistically significantly improved outcomes with surgery than with nonoperative management. Children who presented in the lateral pillar C classification had poorer outcomes regardless of age or treatment.
Osteitis pubis
Osteitis pubis is not commonly seen in young children, but may be seen in late-adolescent runners, late-adolescent soccer players, and young women during pregnancy. It is one of the most common causes of chronic groin pain in the athletic population . There is a reported incidence of 0.5% to 0.7% in the overall athletic population , but there are no reports specifically on pediatric incidence. It is most commonly seen in adults age 30 to 40. Pain at the pubic symphysis is the hallmark of osteitis pubis. It is an aseptic inflammatory condition that can cause erosion and sclerosis at the joint margins . The most likely mechanism is repetitive stress from shearing forces at the joint or from traction of pelvic musculature . Limited hip or sacroiliac range of motion may contribute to increased stresses at the pubic symphysis as well .
Patients present with complaint of insidious-onset, activity-related pain in the groin, anterior hip, or low abdomen. Male patients may have referred scrotal pain. Most do not note pain specifically at the pubic symphysis. However, they are quite tender to palpation over the joint. Pain may also be provoked by resisted active adduction if the distal symphysis is involved, or by sit-ups if the proximal symphysis is involved .
Plain radiographs are frequently normal in early or mild cases, but may show widening of the symphysis, irregular contour, or sclerosis in more advanced cases. In pediatric cases, radiographic abnormalities at the pubic symphysis may be difficult to distinguish from normal developmental ossification. Bone scan may show increased radioisotope uptake, but some symptomatic patients may not show abnormalities. MRI, which is increasingly used for definitive diagnosis, can show marrow edema in early stages or low signal on both T1 and T2 images in later stages .
This condition is usually a self-limited process, but some patients have a prolonged healing course, taking more than a year for complete resolution. Symptoms may be modified with use of oral anti-inflammatory medications or physical therapy aimed at stretching the adductors and improving hip range of motion. Correction of any biomechanical abnormalities that cause increased stress at the symphysis should be addressed in therapy as well. Any notable leg-length discrepancy should be corrected with a heel wedge or orthotics. In selected patients, fluoroscopy-guided diagnostic/therapeutic steroid and anesthetic injection may be used to confirm and treat the condition . However, in the pediatric population, injection should be considered only after conservative measures have been exhausted. Some adults with persistent symptoms go on to have surgical interventions, but there is no literature recommending this type of intervention in children. Other than chronic pain in persistent cases, no significant complications of osteitis pubis are known.
Slipped capital femoral epiphysis
Slipped capital femoral epiphysis (SCFE) is an acquired separation of the proximal femoral head (epiphysis) from the remainder of the femur through the growth plate . A query of a national pediatric database found the incidence to be 10.80 for every 100,000 children with average age of onset of 12.7 years for boys and 11.2 years for girls, with overall male/female ratio of 1.65:1. Incidence was higher in black, Native American, Latino, and Asian/Pacific Islander children than in white children. Bilateral SCFE occurs in roughly 25% to 40% of cases .
The condition is caused when greater shearing stress is applied to the femoral head than can be tolerated by the open physis. It is usually associated with local trauma and may be mediated by other factors, including obesity and endocrine disorders . Children present with pain in the hip, groin, thigh, or, occasionally, the knee (due to sensory distribution of the obturator and femoral nerves) . History of trauma may or may not be noted predating pain or limping gait. Most will be able to bear weight, but may have an abnormal gait. Classic physical examination finding is external rotation and abduction of the hip when testing hip flexion in a supine patient . In chronic cases, there may be mild disuse atrophy of the thigh and gluteal muscles. In cases of unstable SCFE, there is specific history of injury or fall leading to pain and inability to bear weight on the affected limb.
SCFE is considered stable if the child can ambulate and unstable if the child cannot tolerate even crutch-assisted ambulation. Radiographic classification can be made on the amount of slippage. Up to 32% slippage or up to 30° slip angle is considered mild; 33% to 50% slippage or 30° to 60° slip angle is moderate; and greater than 50% slippage or greater than 60° slip angle is severe. Clinical classification includes acute (symptoms less than 3 weeks), chronic (symptoms greater than 3 weeks), or acute on chronic (recent exacerbation of previous symptoms lasting more than 3 weeks.)
Anteroposterior and frog-leg views of the pelvis can help confirm diagnosis, though frog-leg position should be avoided when an unstable slip is suspected ( Fig. 2 ). In cases with high clinical suspicion and normal radiographs, MRI can detect edema or other abnormality of the physis . Non–weight-bearing restrictions (crutches or wheelchair) should be instituted as soon as SCFE is suspected to avoid potentiating further slippage. Stable slips are treated electively with in situ percutaneous pinning (minimally invasive with fluoroscopic guidance). Postoperatively, 6 to 8 weeks of limited or non–weight-bearing status is required. Unstable or severe slips usually require an open procedure, possibly corrective osteotomy. Because of the fairly frequent rate of bilateral SCFE, the contralateral hip should be monitored until skeletal maturity is reached.

Early diagnosis and treatment are key to avoiding potential prolonged morbidity. Avascular necrosis of the femoral head is the most serious potential complication, and occurs most often in severe or unstable cases. Chondrolysis (acute cartilage necrosis) occurs in 5% to 7% of SCFE cases and, if not self-limited, can progress to severe pain and contracture, requiring arthrodesis . Other potential complications include loss of motion, pain, and arthrosis . More severe or untreated cases can lead to altered hip mechanics, causing early degenerative change, potentially leading to need for total hip arthroplasty at an early age.
Stress fractures: femoral neck, pubic ramus, sacral
Stress fractures in young athletes usually stem from one or more of the following: relative osteoporosis due to nutritional or hormonal imbalances, inadequate muscle strength or endurance to provide maximum shock absorption during impact activities, changes in footwear or running surface, or acute increases in training regimen . The most common sites for children are the tibia, fibula, and pars interarticularis of the lumbar spine. These combined account for approximately 85% of pediatric stress fractures . Stress fractures in the hip region are much less common and can occur in the femoral neck, pubic ramus, and sacrum. These types of fractures are also seen in adult athletes, and more commonly in the elderly with osteoporosis.
In children, adolescents, and young adults, stress fractures are related to trabecular inability to withstand increased stresses applied to the area over time . Contributing mechanisms include repetitive overload and impact, abnormal stress distribution from continued activity in the presence of muscle fatigue, and change in ground reaction force (altering the stress pattern in the bone) . These are considered to be fatigue fractures in the adolescent population, in contrast to the insufficiency fractures seen in the elderly with suboptimal bone mass to withstand normal physiologic stress .
The location of the stress fracture determines the clinical presentation. Femoral neck and pubic ramus lesions cause groin or anterior thigh pain; sacral lesions cause lower back or gluteal pain . Physical examination may show limited painful internal rotation or pain with hopping on the affected leg in femoral neck or pubic ramus stress fractures. Pain may be difficult to localize in femoral neck fractures, but tenderness with direct palpation over the pubic ramus is common. In sacral stress fractures, in addition to pain with hopping, patients may have paramedian tenderness on one side of the sacrum or at the sacroiliac joint, positive flamingo test (pain with single-leg stance on the affected side), or positive FABER maneuver (flexion, abduction, external rotation of the hip) .
Abnormalities on plain radiographs may be absent or mild and frequently lag behind symptoms by a month or more. They are usually insufficient to detect sacral stress fractures . Bone scintigraphy can help make early diagnosis, but isotope uptake in the sacral region may be attributed to sacroiliac pathology rather than stress fracture. CT scan and MRI are more specific and are the imaging studies of choice. CT scan can help stage the fracture line and gives better imaging of the bony morphology, while MRI has the benefit of imaging without ionizing radiation .
Femoral neck stress fractures can be superior (traction/tension side) or inferior (compression side). Due to the high risk of progression, superior femoral neck stress fractures are treated surgically with open reduction and internal fixation. The other types of stress fractures mentioned here usually respond to relative rest for 6 to 12 weeks with a gradual return to sport after symptoms resolve. Treatment should also aim to address and modify risk factors. Maintenance of appropriate hormonal and nutritional balance, modification of training (eg, intensity, duration, surface), and modification of footwear can help reduce recurrences . Stress fractures at the traction/tension location have high risk of progressing to complete fracture with associated complications of potential displacement and avascular necrosis . Lesions on the compression side, pubic ramus, and sacrum have low risk of progression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







