Chapter 147 Evaluation of the Patient With a Bone Lesion About the Knee
History
Symptoms
A soft tissue mass may arise from direct tumor extension through cortical bone or may be the result of extension through the haversian canal system, as in the case of Ewing’s sarcoma. The resulting soft tissue mass may be the presenting symptom noted by the patient or may be the cause of diminished range of motion secondary to a mechanical block. A characteristic nocturnal pain pattern relieved by aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) in association with characteristic findings on plain x-ray or computed tomography (CT) scan is diagnostic for an osteoid osteoma.13
Patient Age
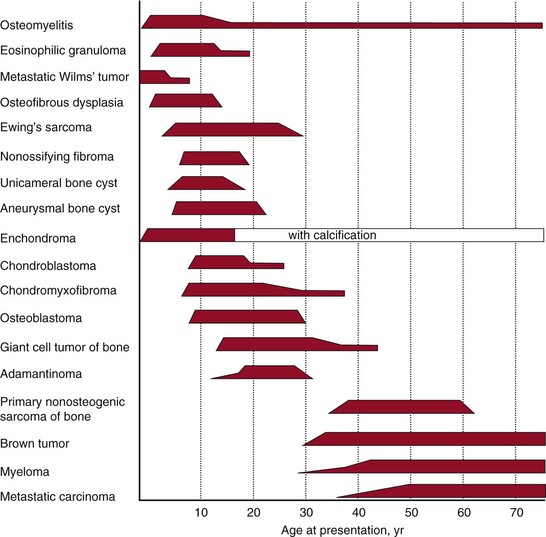
Although many bone tumors may have a similar appearance and presentation, patient age can narrow the differential diagnosis, with certain conditions being more likely to occur in a specific age range (Fig. 147-1).19 For example, a lytic epiphyseal lesion in a skeletally immature patient is more likely a chondroblastoma, and consideration must be given to a giant cell tumor of bone in the skeletally mature patient.20
Past Medical History
Past medical history can be helpful in uncovering significant diagnostic information. A personal history of cancer may lead to several diagnostic possibilities. A lytic bone lesion in a patient with a personal history of cancer is metastatic disease until proven otherwise.1 A patient with a medical history of metastatic carcinoma treated with radiation therapy may have a postradiation sarcoma or a radiation-related insufficiency fracture, and patients who have undergone chemotherapy and/or radiation treatment may have osteonecrosis.8 A past medical history of local or systemic infection should be evaluated for potential osteomyelitis. Patients with a history of chronic obstructive pulmonary disease (COPD), asthma, or conditions commonly treated with steroids should be questioned as to their steroid history, and consideration given to osteonecrosis.9
A family history should be obtained for benign familial osteochondromatosis.16 Li-Fraumeni syndrome is a well-known example of an inherited predisposition for cancer. Germline mutations of the p53 gene predispose patients to many cancers, including osteosarcoma.3
Imaging
Local
Plain radiography remains the most specific noninvasive means of establishing a differential diagnosis for primary bone tumors. Plain radiographs in two perpendicular planes should be the initial imaging study obtained in evaluating a bone tumor about the knee. Commonly, the benign or malignant nature of a tumor can be determined on plain radiographic evaluation. Enneking’s four questions should be asked of any bone tumor to formulate a differential diagnosis.4,5 These questions include (1) location, (2) what the tumor is doing to the bone, (3) what the bone is doing to the tumor, and (4) whether underlying matrix is present. Tumors may have diaphyseal, metaphyseal, or epiphyseal locations or may be surface tumors.
Computed tomography (CT) is the best tool with which to evaluate cortical bone endosteal, skeleton erosion, and lesion mineralization.6 Magnetic resonance imaging (MRI) provides information on anatomy, including bone and soft tissue, as well as definitive tumor margins.21 The MRI scan can give specific information as to the matrix of the tumor. An expansile bone lesion that is multiloculated with multiple fluid-fluid levels is suggestive of an aneurysmal bone cyst. A lesion that is dark on both T1- and T2-weighted sequences is suggestive of a fibrous lesion such as an extra-abdominal desmoid, and a tumor that is bright on both T1- and T2-weighted images is suggestive of a lesion high in water content such as a myxoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree