Etiology of Amputation
Caroline C. Nielsen and Milagros Jorge
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
1. Describe the epidemiology of nontraumatic, traumatic and congenital amputation.
2. Compare and contrast the major causes of amputation.
4. Explain the differences in risk factors of amputation among various racial and ethnic groups.
5. Describe health-promotion efforts for the prevention of dysvascular disease.
Throughout the history of medicine, amputation has been a relatively frequently performed medical procedure and has often been the only available alternative for complex fractures or infections of the extremities. The earliest amputations were generally undertaken to save lives; however, their outcomes were often unsuccessful—many resulted in death from shock caused by blood loss or onset of infection and septicemia in those who survived the operation. In these early amputations, removal of the compromised limb segment as quickly as possible was essential. With the advent of antisepsis, asepsis, and anesthesia in the mid nineteenth century, physicians focused increasingly on the surgical procedure and conservation of tissue.1 The development of modern medical treatment has provided alternatives to amputation. Today, when amputation is necessary, surgery is undertaken with consideration for the functional aspects of the residual limb. This chapter reports the epidemiology of amputation; reviews the causes for amputation; describes the expected outcomes for persons with limb pathology resulting in amputation; and discusses approaches to rehabilitation of the person with limb loss.
Epidemiology of amputation
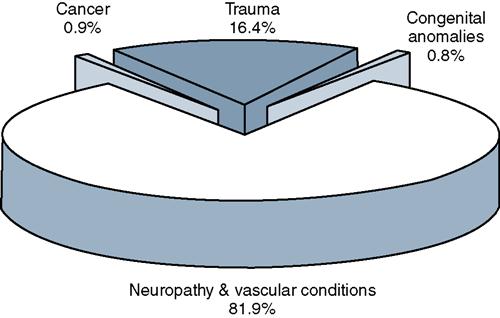
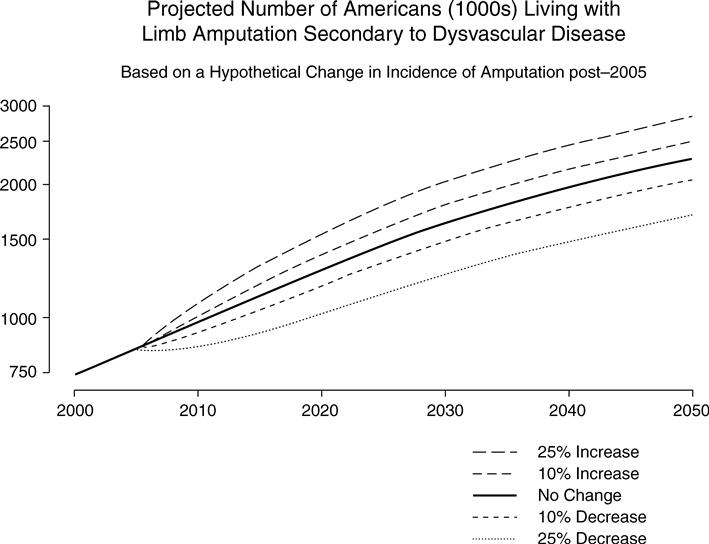
Surveillance data on persons living with limb loss is limited, because in the United States there is no national database for compiling data specific to persons with amputation. Information on persons with amputation is derived from a variety of sources including hospital discharge diagnoses information. The 1996 National Health Interview Survey has the most comprehensive data on amputation and persons living with limb loss.2 The number of Americans living with limb loss is estimated at 1.6 million.3 In the United States, each year, an estimated 185,000 persons lose a limb. Limb loss occurs for a variety of reasons including dysvascular diseases, trauma, cancer, and congenital anomalies (Figures 17-1 and 17-2). In 2008, Ziegler-Graham and colleagues3 conducted an epidemiological study that estimated the prevalence of limb loss in the United States for the period 2005 to 2050. According to statistical analysis based on the figure that 1.6 million Americans were living with limb loss in 2005, it is estimated that the number of persons living with limb loss will increase to 3.6 million by the year 2050. It is anticipated that the number of persons living with amputation will more than double in the next 45 years. Increase in life span and health-related age factors will figure significantly in the increase number of persons living with limb loss (Figure 17-3).3
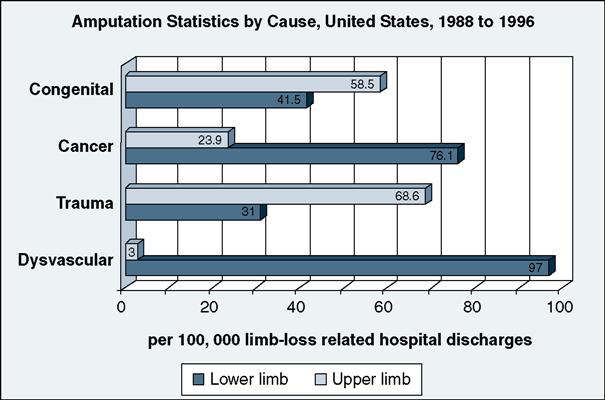
The leading cause of amputation is dysvascular disease. Predisposing factors for amputation include diabetes, hypertension, and dyslipidemia. Health conditions that affect the blood vessels such as peripheral vascular disease (PVD), peripheral arterial disease (PAD), and diabetes are the leading cause of amputation. Dysvascular disease accounts for approximately 82% of all limb loss hospital discharges.4 Between 1988 and 1996, the estimated increase in the rate of dysvascular amputations was 27%, with the highest percentage of disease-related amputations occurring in persons 65 years of age and older.4 Most of these were lower-extremity amputations, which are performed 11 times more frequently than upper-extremity amputations.5 More amputations occur among men than women, and amputation rates increase steeply with age.3,6 The health condition most frequently related to amputation is dysvascular disease including PVD and PAD complicated by neuropathy. Although PVD and neuropathy are frequently associated with type 2 diabetes, vascular disease also occurs independently of diabetes. The increased frequency of amputation for PVD likely reflects increased growth in the older population. This increase is likely to continue with current population projections. The population in the age group 45 to 64 years is projected to increase 23.8% between 2002 and 2020, and the population at greatest risk for amputation, those 65 to 85 years and older, is expected to increase by 71%.7 The population of individuals older than 85 years of age is projected to increase at the highest rate. Because the prevalence of dysvascular increases with age, these demographic changes will likely have a large impact on the amount of vascular reconstruction and amputation that will be performed.3
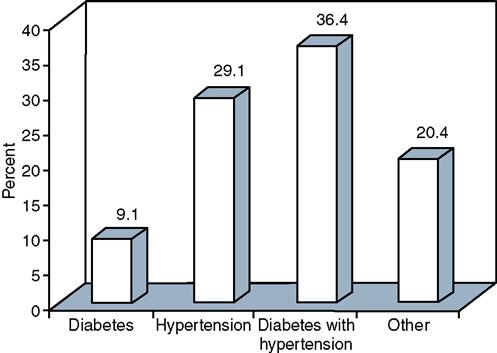
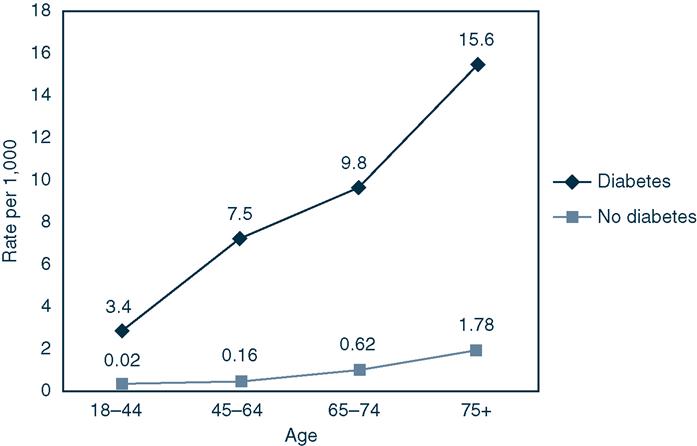
Diabetes and smoking are the strongest risk factors for developing PAD. Other well-known risk factors are advanced age, hypertension, and hyperlipidemia.8 The number of Americans with diabetes with limb loss will continue to rise because of the persistent reports that diabetes is a national health problem. In 2007, approximately 1.6 million new cases of diabetes were diagnosed in people age 20 years or older. If current trends continue, one in three Americans will develop diabetes sometime in their lifetime.9 Diabetes is the leading cause of new cases of nontraumatic lower-extremity amputations among adults (Figure 17-4).9 The number of hospital discharges for nontraumatic lower-extremity amputation with diabetes as a listed diagnosis increased from 45,000 in 1991 to 86,000 in 1996. From 1988 to 2006, the number of hospital discharges for persons with diabetes who had amputation increased by 20%.10,11
The second leading cause of amputation is trauma. Traumatic amputation is most common in the young adult age group (20-29 year olds). The leading causes of trauma-related amputation are injuries involving machinery (40.1%), power tools and appliances (27.8%), firearms (8.5%), and motor vehicle crashes (8%).4 The incidence of trauma-related major amputation continues to decrease over time. This reduction in traumatic amputation is attributable to implementation of new safety regulations, the development of safer farm and industrial machinery, improved safety in work conditions, and medical advancement in techniques for salvaging traumatized limbs. Whenever there is a period of significant armed conflict, the number of veterans with traumatic amputation increases. U.S. engagement in the wars in Afghanistan and Iraq, has resulted in more than 1000 service men and women who have sustained traumatic amputations.12
The third cause of limb loss is cancer related. In the data compiled by the U.S. National Center for Health Statistics, Healthcare and Utilization Project 1988–1996, limb loss as a consequence of cancer showed a marked decrease over this period, from 0.62 per 100,000 persons in 1988 to 0.35 per 100,000 persons in 1996.4 The tumor most commonly associated with amputation is osteosarcoma, which primarily affects children and adolescents in the 11- to 20-year-old age group. Currently amputation is no longer the primary intervention for osteosarcoma, and the current rate of amputation for this disease is less than 1%.5 With development of new surgical techniques, including bone graft and joint replacement, and advancement in chemotherapy and radiation, the incidence of amputation as a consequence of osteosarcoma has decreased significantly.
Congenital limb deficiencies, as well as the amputations used to adjust or correct them, are relatively rare, and little has changed over time in the birth prevalence of congenital limb deficiencies. Rates have been reported ranging from 3.8 per 10,000 births to 5.3 per 10,000 births.4 This percentage has remained relatively stable and is less than 1% of all amputations.
Levels of amputation
Amputation can be performed as a disarticulation of a joint or as a transection through a long bone. The level of amputation is usually named by the joint or major bone through which the amputation has been made (Table 17-1).5 An amputation that involves the lower extremity can affect an individual’s ability to stand and walk, requiring the use of prosthetics and, often, an assistive device for mobility. Amputation involving the upper extremity can affect other activities of daily living, such as feeding, grooming, dressing, and a host of activities that require manipulative skills. Because of the complex nature of skilled hand function, prosthetic substitution for upper limb amputation does not typically restore function to the same degree that lower extremity prosthetics do.
Table 17-1
Terminology Used to Describe the Site of Lower-Extremity Amputation
| Site | Terminology |
| Toe | Phalangeal |
| Forefoot | Ray resection (one or more complete metatarsal) Transmetatarsal (across the metatarsal shaft) |
| Midfoot | Partial foot (e.g., Chopart, Boyd, Pirogoff) |
| At the ankle | Syme |
| Below the knee | Transtibial (long, standard, short) |
| At the knee | Knee disarticulation |
| Above the knee | Transfemoral (long, standard, short) |
| At the hip | Hip disarticulation |
| At the pelvis | Hemipelvectomy |
The levels of amputation surgery that are most commonly performed today involve the lower extremity below the knee (including transtibial, foot, and toe amputations), accounting for 97% of all dysvascular limb loss hospital discharges (Table 17-2). This high percentage reflects the prevalence of PVD of the lower extremities. Transfemoral amputations account for approximately 26% of all dysvascular amputations.4 In general, the proportion of lower-limb amputations in relation to upper-limb amputations is increasing. This most likely reflects an increase in the number of older persons with lower-extremity amputations rather than an actual decrease in the number of upper-extremity amputations.
Table 17-2
| Level of Amputation | Number | Percent (%) |
| Toe | 338,288 | 33.11 |
| Foot and ankle | 116,302 | 11.38 |
| Transtibial | 287,295 | 28.12 |
| Knee disarticulation | 5291 | 0.52 |
| Transfemoral | 266,465 | 26.08 |
| Hip and pelvis | 6588 | 0.64 |
| Bilateral amputations | 1504 | 0.15 |
| Total | 1,021,733 | 100 |
Source: From Dillingham TR, Pezzin LE, Mackenzie EJ. Limb amputation and limb deficiency. Epidemiology and recent trends in the United States. South Med J. 2002;95(8):875-883.
Because dysvascular disease typically affects both lower extremities, a significant number of individuals eventually undergo amputation of both lower extremities. Approximately 50% of persons undergoing diabetes-related amputation will have contralateral amputation within 3 to 5 years.13 Between 25% and 45% of persons with amputations have had amputations of both lower extremities, most often at the transtibial level in both limbs, or a combination of transtibial amputation of one limb and transfemoral amputation of the other.13
Today, the majority of transtibial and transfemoral amputations are performed with an understanding of wound healing and the functional needs and constraints of prosthetic fitting, so that rehabilitation outcomes are usually positive. Other levels of amputation, although less commonly performed procedures, continue to pose challenges for the surgeon, prosthetist, physical therapist, and patient during prosthetic fitting and rehabilitation.
Causes of amputation
Currently the most likely reasons for amputation are poor wound healing associated with diabetes4,14 and dysvascular disease,4,15 trauma,4,16 or cancer.4,17 Children with congenital limb deficiencies are a special population group and may require surgical revision during or after periods of significant growth or after conversion to a more functional level for prosthetic fitting.
Diabetes and Peripheral Arterial Disease
Diabetic foot ulceration is a common complication of diabetes that often results in lower-extremity amputation. Elevated blood sugars associated with diabetes damage blood vessels and nerve fibers, and impair circulation. Nerve damage causes peripheral neuropathy, a condition of loss of sensation to the feet. The loss of protective sensation in the feet would not alert an individual to foreign substance in their shoe such as pebbles or gravel. This lack of awareness may lead to blisters or other minor injuries. Once the skin is broken, sores on the feet may not heal because of poor circulation. The Centers for Disease Control confirms that neuropathy is a major contributor to diabetic amputations.18
The prevalence of PAD in persons with diabetes is four times greater than in persons without diabetes.19 Dysvascular disease is the most common contributing factor for lower-extremity amputations. In epidemiological studies, two symptoms are classic indicators of vascular insufficiency: (a) intermittent claudication and (b) loss of one or more lower-extremity pulses. Intermittent claudication is a significant cramping pain, usually in the calf, that is induced by walking or other prolonged muscle contraction and relieved by a short period of rest. In arteriosclerosis obliterans, at least one major arterial pulse (dorsal pedis artery at the ankle, popliteal artery at the knee, or femoral artery in the groin) is often absent or markedly impaired (Figure 17-5).20 The major risk factors for development of PAD are the same as those for cardiovascular and cerebrovascular disease, most notably poorly managed hypertension, high serum cholesterol and triglyceride levels, and a history of tobacco use and smoking. Peripheral neuropathy and PAD are the major predisposing factors for lower-extremity amputation in individuals with diabetes.21
According to the National Hospital Discharge Survey, the number of hospital discharges that listed diagnoses of amputation and diabetes increased 27% from 1988 to 1996.4 The prevalence of PAD among persons with diabetes, whether men or women, is significantly greater than in those without diabetes. The Framingham Heart Study22 found a four to five times greater relative risk of intermittent claudication in persons with diabetes, even when controlling for blood pressure, cholesterol, and smoking. The age-adjusted rate of lower-extremity amputation among persons with diabetes in the United States is approximately 28 times that of the nondiabetic population. More than 50% of the lower-limb amputations in the United States are diabetes related, although persons diagnosed with diabetes represent only 3% of the population.23 Although major improvements have been made in noninvasive diagnosis, surgical revascularization procedures, and wound-healing techniques, between 2% and 5% of individuals with PAD and without diabetes and between 6% and 25% of those with diabetes eventually undergo an amputation.24,25
The three most common predisposing factors for lower extremity amputation appear to be (a) concurrent diabetes and hypertension, (b) hypertension without diabetes, and (c) diabetes without hypertension (Figure 17-6). Other predisposing factors include race, gender, history of smoking, and previous vascular surgery. The incidence of lower-extremity amputation among persons with diabetes is almost 50% higher for men than for women.4 The most frequently cited criteria for amputation among persons with diabetes include gangrene, infection, nonhealing neuropathic ulcer, severe ischemic pain, absent or decreased pulses, local necrosis, osteomyelitis, systemic toxicity, acute embolic disease, and severe venous thrombosis.19,21
In individuals with diabetes, the prevalence and severity of dysvascularity increases significantly with age and the duration of diabetes, particularly in men. Initial amputation may involve a toe or foot; subsequent revision to transtibial or transfemoral levels is likely to occur with progression of the underlying disease. In individuals with diabetes, dysvascular disease increases the risk of a nonhealing neuropathic ulcer, infection, or gangrene, all of which increase the likelihood of amputation. Twenty percent to 50% of patients will have amputation of the contralateral leg in 1 to 3 years.13,19 Patients with diabetes who are 65 years old or older account for most diabetes-related lower-extremity amputations. The estimated amputation rate in 1996 was 1.4 times higher for persons with diabetes who were 65 to 74 years old and 2.4 times higher for those 75 years of age or older, compared with those 0 to 64 years of age.26,27
Peripheral neuropathy is a common complication of diabetes. Neuropathy is as important and powerful as dysvascular disease as a predisposing factor for lower-extremity amputation. Peripheral neuropathy is suspected when one or more of the following clinical signs are present: deficits of sensation (loss of Achilles and patellar reflexes, decreased vibratory sensation, and loss of protective sensation), motor impairments (weakness and atrophy of the intrinsic muscles of the foot), or autonomic dysfunction (inadequate or abnormal hemodynamic mechanism, tropic changes of the skin, and distal loss of hair).20 The resulting loss of thermal, pain, and protective sensation increases the vulnerability of the foot to acute, high-pressure and repetitive, low-pressure trauma. Patients may also experience significant numbness or painful paresthesia of the foot and lower leg. Individuals with peripheral neuropathy may not be aware of minor trauma, pressure from poorly fitting shoes along the sides and tops of their feet, or pressure from thickening plantar callus, all of which contribute to the risk of ulceration, infection, and gangrene. Motor neuropathy and associated weakness and atrophy contribute to development of bony deformity of the foot. The bony prominences and malalignments that are associated with foot deformity change weight-bearing pressure dynamics during walking, further increasing the risk of ulceration. Peripheral neuropathy is one of the most crucial precursors of foot ulceration, especially in the presence of dysvascular disease. Nonhealing or infected neuropathic ulcers precede approximately 85% of nontraumatic lower extremity amputations in individuals with diabetes.23
Lower-extremity amputation continues to be a major health problem for the diabetic population. For this group of patients, amputation is associated with significant morbidity, functional limitation and disability, mortality, and high health care costs. Approximately 185,000 persons undergo amputation each year in the United States.3 The average cost for a patient per hospitalization for amputation is approximately $30,000. The cost of health care for persons with chronic diseases such as diabetes and PAD is estimated by the American Diabetes Association at $174 billion per year.28 According to the U.S. Public Health Service, reducing the incidence of lower-extremity amputations in persons with diabetes is a key health care objective in terms of quality of life and containment of health care costs. It is estimated that the current prevalence of 1.6 million persons living with limb loss will more than double to 3.6 million by the year 2050.3 Planned health promotion efforts will hopefully reduce the risk of diabetes and amputation, minimizing the impact of risk factors and increasing access to care by multidisciplinary health care teams.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree