Chapter 29 Epidemiology and Management Tips in the Professional Athlete
Introduction
Athletic competition has become normative in culture today. People enjoy competing against a worthy rival in the name of sportsmanship, the thrill of pushing the limits of the human body, for fitness, for the thrill of victory, and more recently as a full-time career. Evaluation and management of the elite athlete has been covered in Chapter 1. Foot and ankle injuries are among the most common maladies that plague the elite athlete. In professional sports, these injuries can result in the inability to participate and hinder a team’s chances for victory. For the individual, a prolonged recovery can lead to loss of playing time, a depressed sense of worth, an inability to contribute, and even a substantial loss of revenue, while jeopardizing a career.
Epidemiology
| NFL | |
| Cincinnati Bengals | Paul Sparling |
| New Orleans Saints | Scottie Patton |
| NBA | |
| Atlanta Hawks | Wally Blasé |
| Charlotte (New Orleans) Hornets | Terry Kofler |
| Golden State Warriors | Tom Abdenour |
| Los Angeles Lakers | Gary Vitti |
| Milwaukee Bucks | Troy Wenzel |
| Orlando Magic | Ted Arzonico |
| Utah Jazz | Gary Briggs |
| MLB | |
| Anaheim Angels | Ned Bergert |
| Arizona Diamondbacks | Paul Lessard |
| Baltimore Orioles | Richie Bancells |
| Chicago White Sox | Herm Schneider |
| Colorado Rockies | Tom Probst |
| Florida Marlins | Larry Starr |
| Houston Astros | — |
| Milwaukee Brewers | Roger Caplinger |
| Montreal Expos | Ron McClain |
| New York Yankees | Gene Monham |
| Oakland Athletics | Larry David |
| Texas Rangers | Danny Wheat |
| Toronto Blue Jays | Scott Shannon |
| NHL | |
| Buffalo Sabres | Jim Pizzutelli |
| Columbus Blue Jackets | Chris Mizer |
| Dallas Stars | Dave Suprenant |
| Minnesota Wild | Don Fuller |
| Montreal Canadiens | Graham Rynbend |
| Phoenix Coyotes | Gord Hart |
| San Jose Sharks | Ray Tufts |
| Tampa Bay Lightning | Dave Boyer |
| MLS | |
| Chicago Fire | Rich Monis |
| Colorado Rapids | Theron Enns |
| DC United | Rich Guter |
| New England Revolution | Mike Fritz |
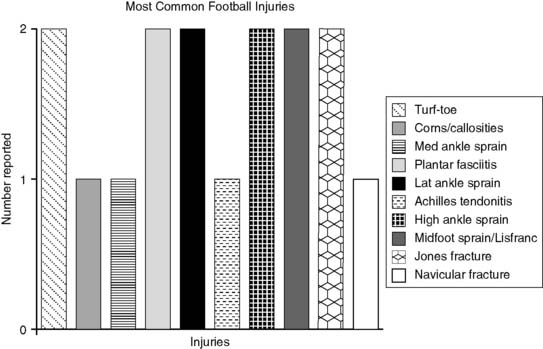
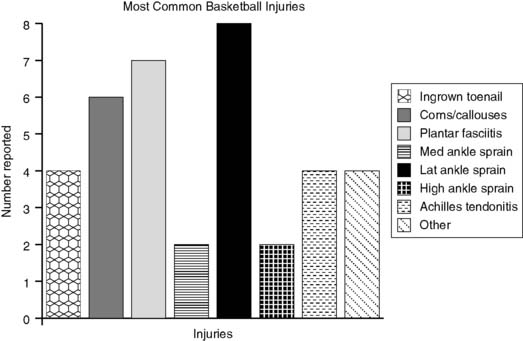
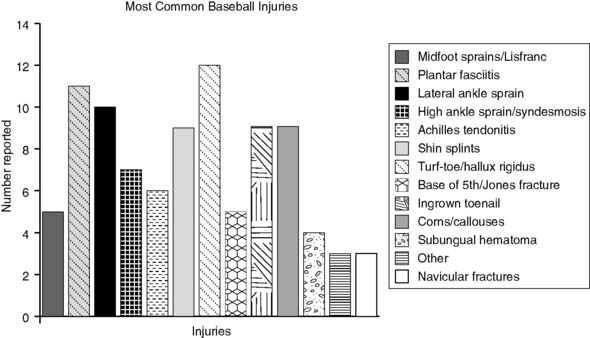
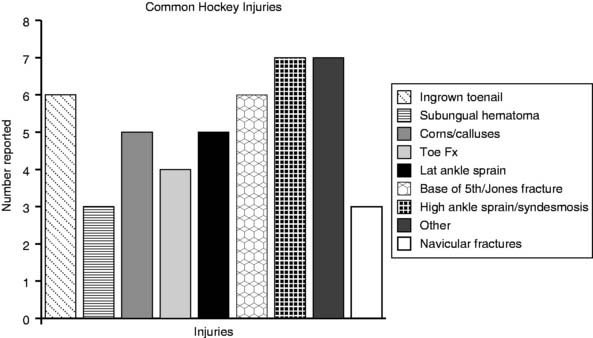
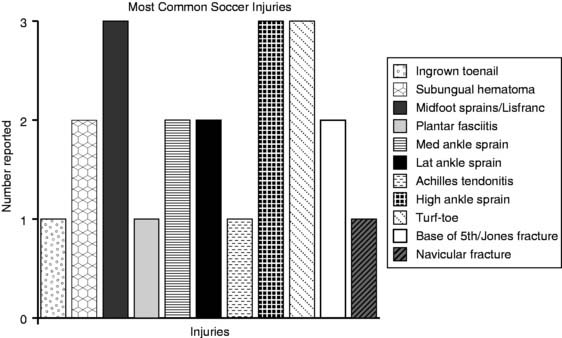
The 34 participants were asked to list the five most common foot and ankle injuries treated among their professional athletes. Equal weight was given to all responses, whether listed first or last, and to each responder. The results are listed below. The results also were subdivided among each particular sport and are plotted in Figs. 29-1, 29-2, 29-3, 29-4, and 29-5.
Turf-Toe/Hallux Rigidus
Turf-toe involves a severe dorsiflexion injury to the great toe metatarsophalangeal (MTP) joint as described in Chapter 18. Other, less common mechanisms include varus/valgus stresses resulting in a combined turf-toe and “traumatic bunion.” The joint capsule is strained, the plantar plate can be stretched, and the articular cartilage can be contused and lead to long-term joint arthrosis. These injuries are commonly described in football, with hard turf and flexible shoes increasing the incidence. This can be quite debilitating, with long periods of recovery, especially if the plantar plate is disrupted. One can imagine the difficulty in a football player dependent on push-off if there is significant limitation of motion and loss of power. Turf-toe (hyperextension with primary plantar soft-tissue injury) does occur in other sports but is much less frequent and typically is less severe. That being said, we have treated a Division I baseball pitcher who suffered a complete plantar plate disruption coming off the mound to field the ball, necessitating surgical repair. He is now in the minor leagues pitching without pain.