Fig. 36.1
Lower leg and foot purpura with necrotic and superficial ulcerations of a patient with eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome)

Fig. 36.2
Diffuse erythematous plaque with a palpable subcutaneous nodule (circled) below the calf of a patient with eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome)
The so-called extravascular granulomas, initially described by Churg and Strauss as a possible manifestation of EGPA, may be seen in other systemic vasculitides and some connective tissue diseases and have, therefore, been given different other names, including Winkelmann’s granuloma [1, 8–10]. Clinically, these red-to-violaceous lesions may be linear (“rope sign”), on the trunk or extensor surfaces of the upper arms, but also frequently resemble large, annular, 2-mm to 2-cm-sized papulonodules or plaques.
Differential Diagnosis
Because skin lesions are rarely the first and isolated symptoms of EGPA (6 % of the patients), common causes of purpuric lesions, such as thrombocytopenia or Bateman’s syndrome, or urticarial rash, e.g., drug or contact allergy, are easily ruled out [3]. Some other diagnoses may be more challenging, because several of these diseases’ manifestations may mimic those of EGPA. Other systemic vasculitides like granulomatosis with polyangiitis (Wegener’s granulomatosis), parasitic infections, and hypereosinophilic syndromes especially should be evoked and actively looked for. Lymphocyte immunophenotyping, T-cell clonal studies, and molecular analyses to detect Fip1-like 1 (FIP1L1)–platelet-derived growth factor receptor-α (PDGFRA) gene fusion should probably be done in every ANCA-negative patients, to exclude myeloid neoplasms associated with eosinophilia. Other diagnoses to exclude are hypersensitivity vasculitis, Carrington’s disease, and malignant hemopathies (especially lymphomas), along with Crohn’s disease, sarcoidosis, eosinophilic fasciitis, or Gleich syndrome.
Biopsy
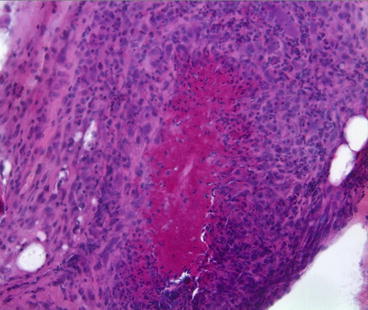
Histologically, vasculitis may be found in two-thirds of the positive skin biopsies of EGPA patients, but the most “typical” and/or eosinophilic granulomas are detected in less than half of them [8–10]. Examination of nodules may show granulomatous vasculitis, necrotizing vasculitis of arterioles in the deep dermis or the subcutis, or extravascular granulomas (Fig. 36.3). Purpuric lesions can reveal vasculitis, usually paired with eosinophil-rich inflammatory infiltrates. Two patterns of extravascular granulomas have been distinguished: the first is classic, with palisading granuloma and eosinophils when associated with EGPA, or basophilic debris (“blue” granuloma due to neutrophil–mucin degradation) in granulomatosis with polyangiitis (Wegener’s) or rheumatoid arthritis, and the second is focal basophilic necrosis, without a palisading organization.