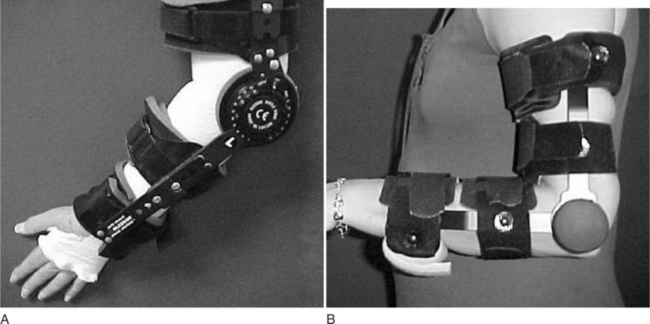
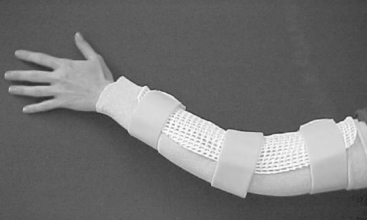
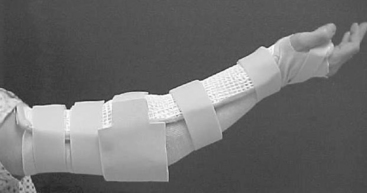
CHAPTER 10 1 Define anatomic and biomechanical considerations for splinting the elbow. 2 Discuss clinical/diagnostic indications for elbow immobilization splints. 3 Identify the components of elbow immobilization splints. 4 Describe the fabrication process for an anterior and posterior elbow splint. 5 Review precautions for elbow immobilization splinting. 6 Use clinical reasoning to evaluate a problematic elbow immobilization splint. 7 Use clinical reasoning to evaluate a fabricated elbow immobilization splint. 8 Apply knowledge about the application of elbow immobilization splints to a case study The elbow joint consists of three bones: distal humerus, proximal ulna (olecranon process), and the head of the radius. The elbow joint is comprised of three complex articulations: ulna-humeral, radio-capitellar, and proximal radio-ulnar. Flexion and extension of the elbow occur at the ulnohumeral joint. Flexion, extension, and rotation occur at the radiohumeral joint. Forearm rotation occurs at the proximal and distal radioulnar joints along a longitudinal axis [Morrey 2000a]. The elbow is particularly prone to contracture and stiffness due to the high congruity, multiple articulations, and the close relationship of ligaments and muscle to the joint capsule [Hotchkiss 1996]. For this reason prolonged immobilization is to be avoided whenever possible. The bony prominences, lateral and medial epicondyle, radial and ulnar heads, and olecranon require protection and special consideration during splinting. Splints are commonly constructed for elbow fractures, elbow arthroplasty, elbow instability, biceps and triceps repair, and cubital tunnel syndrome (Table 10-1). Table 10-1 Conditions That Require an Elbow Immobilization Splint Elbow trauma can result in a simple one-bone fracture or a complex fracture/dislocation involving a combination of bones. These injuries vary by the bones and structures involved, and the extent of the injury. Elbow dislocations occur in isolation or along with a fracture. Both fractures and dislocations often include concomitant soft-tissue injury such as ligament, muscle, or nerve. Seven percent of all fractures are elbow fractures [Jupiter and Morrey 2000], and of this one-third involve the distal humerus. The mechanism of injury is a posterior force directed at the flexed elbow, often a fall to an outstretched hand, or axial loading of an extended elbow. Thirty-three percent of all elbow fractures occur in the radial head and neck by axial loading on a pronated forearm, with the elbow in more than 20 degrees of flexion [Morrey 2000c]. Radial head fractures are often associated with ligament injuries. Radial head fractures associated with interosseous membrane disruption and distal radial ulnar joint dislocation are termed Essex-Lopresti lesions. Twenty percent of elbow fractures occur in the olecranon as a result of direct impact or of a hyperextension force [Cabanela and Morrey 2000]. When the radial head dislocates anteriorly along with an ulnar fracture, the result is a Monteggia fracture. Another common fracture location along the proximal ulna is the coronoid process [Regan and Morrey 2000]. Elbow fractures are managed conservatively with closed manipulation or immobilization and surgically with open reduction internal fixation (ORIF) or external fixation. Healing structures are protected in a brace, cast, or custom-molded thermoplastic splint to maintain alignment and prevent deformity. Splint designs vary and are based on the surgeon’s preference, therapist’s experience, and the client’s needs. The protective splint is worn for as long as 2 to 8 weeks postoperatively, depending on the stability of the fracture/joint and the severity of the injury. The position and angle of immobilization are based on the type of fracture. Distal humeral fractures are immobilized in 90 degrees of elbow flexion, with the forearm in neutral rotation (Figure 10-1A). Olecranon and proximal ulna fractures often involve injury to the triceps tendon. To protect the injured tendon, the elbow is immobilized in 60 to 70 degrees of flexion, the forearm in neutral, and the wrist in slight extension (Figure 10-1B). Complex radial head fractures/dislocations and radial head replacements are immobilized in up to 120 degrees of flexion to stabilize the radial head (Figure 10-1C). The protective splint is worn continuously at first, and is removed only for protected exercises (when indicated) and for hygiene. Once the fracture/joint is considered stable, the splint is removed more frequently for exercises and light functional activities. The splint is gradually weaned during the day, and continues to be worn for sleep and protection until the fracture is completely stable [Barenholtz and Wolff 2001]. Elbow arthroplasty refers to resurfacing or replacement of the joint. The primary goal of total elbow arthroplasty is pain relief with restoration of stability and functional motion (arc of 30 to 130 degrees). An elbow replacement is considered when the joint is painful, is restricted in motion, or has destroyed articular cartilage. Clients who are elderly or have low demands that present with rheumatoid arthritis, advanced post-traumatic arthritis, advanced degenerative arthritis, or nonunion and comminuted distal humeral fractures are good candidates for this surgery [Morrey 2000b]. Total elbow arthroplasty includes three types of implants: constrained, nonconstrained, and semiconstrained. The choice for a specific implant is based on the extent and cause of the disease, the specific needs of the client, and the surgeon’s preference [Cooney 2000, Morrey et al. Wolff 2000]. An immobilization splint or brace is provided on the first postoperative visit. Several options are available based on the preference of the surgeon and the experience of the therapist. Some surgeons prefer a brace such as the Bledsoe brace (Bledsoe Brace Systems, Grand Prairie) (Figure 10-2A) or Mayo Elbow Universal Brace (Aircast, Summit, NJ) (Figure 10-2B). The brace provides medial and lateral stability while allowing flexion and extension of the elbow. The parameters of the brace are preset to limit end range in both flexion and extension. Extension is set to tolerance, and flexion is determined by the condition of the triceps muscle and surgical repair. Protected range of motion exercises are initiated with the brace on for 2 to 3 weeks. Another common option is a posterior elbow immobilization splint (seeFigure 10-1A), a custom-molded thermoplastic splint positioned in 80 to 90 degrees of flexion. The advantages of this splint are that it fits well by conforming to the client’s elbow and that it can be remolded to accommodate changes in edema. Disadvantages of the splint include posterior pressure at the incision site and development of an elbow flexion contracture if the splint is not removed regularly for exercise. The splint is removed 3 to 4 times daily for the performance of protected range-of-motion exercises. In the presence of infection or instability, the splint is worn continuously and for a longer period of time. Many surgeons prefer no splint at all. Instead, the arm is wrapped lightly in an Ace bandage and positioned in a sling. This approach encourages early functional use and is comfortable and well tolerated. The rationale is that pain and postsurgical swelling will limit the end range of motion. Elbow instability results from a dislocation of the ulnohumeral joint and injury to the varus and valgus stabilizers of the elbow and the radial head [Hotchkiss 1996]. This injury often results from a forceful fall on an outstretched hand. The impact drives the head of the radius into the capitellum of the humerus [O’Driscoll 2000]. This may result in radial head and coronoid process fracture, medial collateral, and posterolateral and/or lateral collateral ligament disruption. When all of these structures are injured, the condition is described as the “terrible triad” [Hotchkiss 1996]. The treatment plan begins with fabrication of a custom thermoplastic posterior elbow shell with the elbow positioned in 120 degrees or more of flexion and the forearm in full pronation (seeFigure 10-1C). The wrist is included and splinted in neutral. A figure-of-eight strap may be added to further stabilize the elbow in 120 degrees for a larger-framed individual (Figure 10-3). The splint is worn at all times and removed 3 to 5 times daily for protected exercises. The elbow must be in 120 degrees or more of flexion to ensure approximation of the radial head. Distal biceps tendon rupture is uncommon and occurs more frequently in men than in women. The mechanism of injury is a strong extension force applied to the elbow in the flexed position, such as attempting to catch a heavy object with an outstretched hand [Kannus and Natri 1997]. Treatment varies from conservative management via immobilization to surgical repair via a one-incision or two-incision approach. The position and method of immobilization is determined by the preference of the surgeon. Common methods of immobilization include a brace or posterior elbow splint locked at 90 degrees of flexion and the forearm immobilized in pronation. Some physicians prefer that the forearm be immobilized in neutral rotation, and yet others immobilize in supination. Elbow flexion is permitted as tolerated from the locked position of 90 degrees. Three weeks postoperatively elbow extension is increased by 10 to 15 degrees per week. The brace is generally worn for a period of 6 to 8 weeks. The benefit of using a brace for biceps tendon repairs is that it is easily adjusted to accommodate the change in the angle of motion. A thermoplastic splint requires frequent readjustment and remolding that can be cumbersome and time consuming. Cubital tunnel syndrome is the second most common site of nerve compression in the upper extremity following carpal tunnel [Blackmore 2002, Rayan 1992]. Anatomically, the ulnar nerve is susceptible to injury at the elbow. Injury to the nerve may occur as a result of trauma or prolonged or sustained motion that compresses the nerve over time [Fess et al. 2005]. Symptoms include pain and parasthesias (numbness, tingling) over the sensory distribution of the ulnar nerve, the ulnar two digits of the hand. In advances stages, weakness and atrophy of the hypothenar muscles and thumb adductor may be seen. Conservative management focuses on avoiding postures and positions that aggravate the symptoms. Clients are instructed to avoid repetitive or sustained elbow flexion. For this purpose, a nighttime anterior elbow extension splint is fabricated with the elbow positioned in 30 to 45 degrees of extension (Figure 10-4). A commercial elbow pad is helpful to protect the ulnar nerve at the elbow. The pad can be reversed and worn anteriorly as an alternative to the splint to prevent elbow flexion. Serial static and static progressive splints are designed to increase motion in a stiff joint by providing a low-load and prolonged stretch [Flowers and LaStayo 1994]. Posttraumatic stiffness following elbow fractures and dislocations is the most common cause of elbow contracture. Other causes include osteoarthritis or inflammatory arthritis, congenital or developmental deformities, burns, and head injury. The elbow joint is prone to stiffness for several reasons. Anatomically, the joint is highly congruent. In most joints of the body, the tendinous portions of the muscles that act on the joint lie over the joint capsule. In the elbow, however, the brachialis muscle belly lies directly over the anterior joint capsule—making adhesion formation between the two structures inevitable following injury. The elbow is often held in 70 to 90 degrees of flexion post-injury, as that is the position of greatest intracapsular volume for accommodation of edema. The thin joint capsule responds to trauma by thickening and becoming fibrotic, quickly adapting to this flexed position of the elbow. This results in a tethering of joint motion, particularly in the direction of extension [Wolff and Altman 2006]. Biomechanically, the strong (and often co-contracting) elbow flexors overpower the weaker elbow extensors—which challenges the ability to regain extension [Griffith 2002]. Last, the elbow joint is prone to heterotopic ossification following trauma and surgery. For extension contractures of less than 45 degrees, an anterior thermoplastic serial static elbow extension splint (Figure 10-5) is fabricated for use at night. This provides low-load prolonged positioning at the end range of elbow extension [Gelinas et al. 2000]. It is remolded into greater extension as tolerated. For extension contractures of greater than 45 degrees, a static progressive elbow splint is either fabricated or provided. An effective design for a static progressive elbow extension splint is the turnbuckle splint (Figure 10-6). It should be noted that this splint requires experience, expertise, and time. A simpler alternative is the Mayo elbow universal brace (Aircast, Summit, NJ), described previously. The brace can be locked in position and has a static progressive component that can be used to gain motion in both flexion and extension (Figure 10-7).
Elbow Immobilization Splints
Anatomic and Biomechanical Considerations
Clinical Indications and Common Diagnoses
CONDITION
SUGGESTED WEARING SCHEDULE
TYPE OF SPLINT AND POSITION
Elbow fractures
After removal of the postoperative dressing, the therapist fabricates an elbow immobilization splint. The splint is worn at all times, and removed for exercises and hygiene if permitted.
Posterior angle depends on which structures need to be protected.
Elbow arthroplasty
After removal of the postoperative dressing the therapist fabricates an elbow immobilization splint or fits the client for a brace. The splint is worn at all times, and removed for protected range-of-motion exercises until the joint is stable.
Posterior in 90 degrees of flexion, or Bledsoe brace or Mayo elbow brace in 90 degrees.
Elbow instability
After removal of the postoperative dressing a posterior elbow immobilization splint in 120 degrees of flexion is provided. Therapist-supervised protected range-of-motion exercises are performed until the joint become more stable. The client is not permitted to remove the splint unsupervised.
Posterior in 120 degrees of flexion or brace locked in 120 degrees.
Biceps/triceps repair
Splint is worn at all times and removed for protected range-of-motion exercises.
Posterior elbow splint immobilized in prescribed angle based on structures requiring protection. Splint is usually adjusted to increase the angle of immobilization by 10 to 15 degrees per week at 3 weeks postoperatively.
Cubital tunnel syndrome
A nighttime splint is provided for use while sleeping. Proper positioning during work and leisure activities is reviewed.
Volar splint elbow immobilized in 30 to 45 degrees extension or reverse elbow pad.
Splinting for Fractures
Splinting for Total Elbow Arthroplasty
Splinting for Instability
Splinting for Biceps and Triceps Rupture
Splinting for Cubital Tunnel Syndrome
Serial Static and Static Progressive Splinting of the Elbow
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Elbow Immobilization Splints