CHAPTER 28 Elbow Dislocations
INTRODUCTION
The elbow is the second most commonly dislocated joint, after the shoulder, in adults. In the pediatric age group, it is the joint most commonly dislocated. Despite the prevalence of this injury, there are few analyses of series of this dislocation in the literature.7,16,19,25,29,36,46,52,68,76,96
MECHANISM OF INJURY
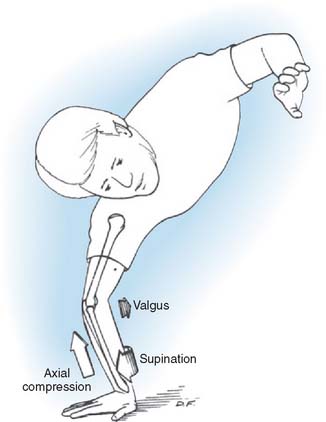
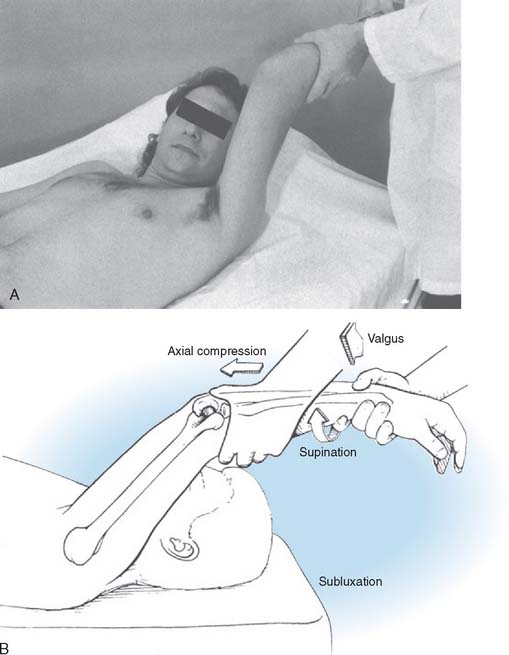
Although it used to be thought that dislocations occurred by hyperextension, it is now widely accepted that the mechanism of posterolateral rotatory posterior displacement of the elbow is responsible for most posterior dislocations resulting from falls on the outstretched hand. Motor vehicle accidents, direct trauma, and miscellaneous causes that account for the rest can have other mechanisms. The elbow experiences an axial compressive force during flexion as the body approaches the ground. As the body rotates internally on the elbow (forearm rotates externally on the trunk), a supination moment occurs at the elbow. A valgus moment results from the fact that the mechanical axis is lateral to the elbow (Fig. 28-1). This combination of valgus instability and supination with axial compression during flexion is precisely the mechanism that results in a posterolateral rotatory subluxation or dislocation of the elbow and can be reproduced clinically by the lateral pivot-shift test, which is described later.55 We have documented this exact mechanism in two patients whose dislocations were caught on video camera during wrestling matches.
Osborne and Cotterill64 first suggested a posterolateral rotational displacement as the mechanism of elbow dislocation. The radial collateral ligament and the lateral capsule are torn. They suggested a method of repair for recurrent dislocation based on this theory of mechanism, which involved imbrication of the lateral soft tissues. The method has been used with success.25
The forces acting on the joint, besides producing tensile forces that disrupt the ligamentous constraints, also produce substantial compressive and shear forces on the articular surfaces. Therefore, adjunctive fractures, such as those occurring in the radial head and neck or capitellum, are frequent.2,15 There is evidence from reports of dislocations treated by open means that chondral injuries to the capitellar and trochlear surfaces are probably much more common than was previously believed.11,23
In the child, late nucleation and closure of the physes alter the response to dislocation forces and certainly increase the difficulty of radiographic interpretation. This is covered separately in Chapter 16.
CLASSIFICATION
Acute elbow dislocations are classified as posterior, anterior, and divergent.
POSTERIOR DISLOCATIONS
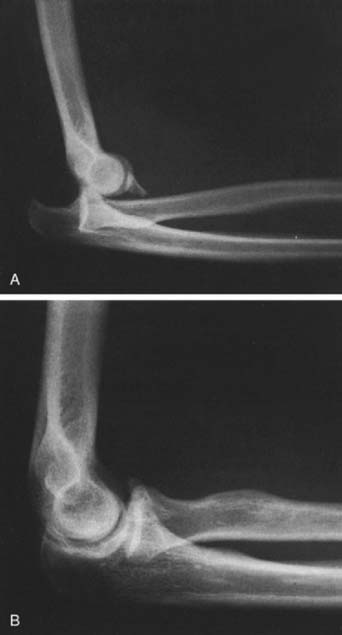
By far the most common dislocation occurs posteriorly (Fig. 28-2). Whether the forearm is medially or laterally displaced is irrelevant to the pathologic condition seen or the ultimate treatment.
ANTERIOR DISLOCATIONS
Anterior dislocations are extremely rare and are usually seen in younger individuals (Fig. 28-3).5,93 The forearm bones are displaced anterior to the distal humerus. The mechanism of injury is not well understood or proven, but there is a forward rebounding force that allows the olecranon to slide under the trochlea and the radial head to dislocate from the capitellum. In adults, the olecranon is usually fractured.
PATHOMECHANICS OF ELBOW INSTABILITY
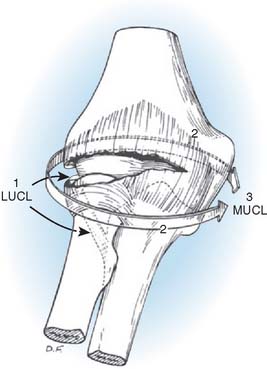
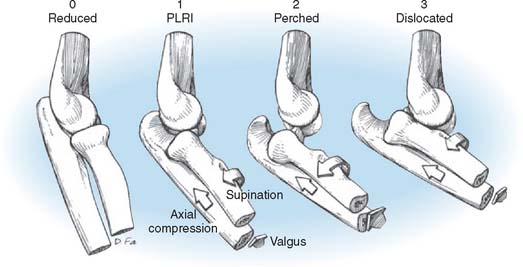
The pathoanatomy can be thought of as a circle of soft tissue disruption from lateral to medial in three stages (Figs. 28-4 and 28-5).
In stage 1, the ulnar part of the lateral collateral ligament is disrupted (the remainder of the lateral collateral ligament complex may be intact or disrupted). This results in posterolateral rotatory subluxation of the elbow, which reduces spontaneously.6,55,61
With further disruption anteriorly and posteriorly, the elbow is capable of an incomplete posterolateral dislocation (stage 2). The concave medial edge of the ulna rests on the trochlea in such a way that a lateral radiograph gives one the impression that the coronoid is perched on the trochlea.51
Stage 3 has two parts. In stage 3A, all the soft tissues are disrupted around to and including the posterior part of the medial collateral ligament, leaving the important anterior band intact. This permits posterior dislocation by the previously described posterolateral rotatory mechanism. The elbow pivots around on the intact anterior band of the medial collateral ligament. In stage 3B, the entire medial collateral complex is disrupted. Gross varus and valgus as well as rotatory instability is present following reduction, owing to the fact that all ligaments and capsules are disrupted. Surgical exploration has established that the anterior medial collateral ligament usually is disrupted by a complete dislocation of the elbow.7,9,11,13 These pathoanatomic stages correlate with clinical degrees of elbow instability.
Therefore, dislocation is the final of three sequential stages of elbow instability resulting from posterolateral ulnohumeral rotatory subluxation, with soft tissue disruption progressing from lateral to medial. In each stage, the pathoanatomy is correlated with the pattern and degree of instability. This has been confirmed in studies of cadaver elbows; 12 of 13 of the elbows could be dislocated posteriorly, with the anterior medial collateral ligament intact.21,56 In all 13 elbows, the coronoid could be perched on the trochlea after release of the lateral collateral ligament complex and the lateral half of the anterior capsule. Following reduction, the elbows were clinically stable to valgus stress.
This hypothesis explains the spectrum of instability, from posterolateral rotatory instability to perched dislocation to posterior dislocation without or with disruption of the anterior medial collateral ligament, which occurs with further posterior displacement. Such a posterolateral rotatory mechanism of dislocation is compatible with those suggested by Osborne and Cotterill,64 Roberts,76 and others.1,27,63 The injury patterns in the lateral collateral ligament have been documented.47 The overwhelming majority are by detachment of the lateral collateral ligament (LCL) complex from its origin on the lateral condyle. In most cases, the common extensor tendon is also disrupted.
ASSOCIATED INJURIES
Associated injuries with elbow dislocation are com-mon.28,32,62,77,80,95,97 Radial head and neck fractures occur in about 5% to 10% of cases secondary to compressive loading at the radiocapitellar joint. Avulsion of fragments from either the medial or the lateral epicondyles occurs in approximately 12% of cases, and fractures of the coronoid process occur in 10% of dislocations (see Fig. 28-2). It is essential to obtain stability following a fracture-dislocation because the treatment of persistent instability following fracture dislocations is unpredictable.65 One should be particularly careful to assess for fractures of the anteromedial facet of the coronoid (computed tomography [CT] scanning with three-dimensional surface rendering is best) because even an apparently minor fragment can be the only sign of a very serious injury with a grave prognosis due to posteromedial rotatory instability from a fracture subluxation.10,57,59,60
Displacement of the medial epicondyle in adolescents ranges from minimal to incarceration of the epicondyle within the joint (Fig. 28-6).36,69,79,88,90,98 The latter, if undetected, results in significant traumatic arthrosis (Fig. 28-7). Medial epicondylar fracture can predispose to late secondary dislocation.36 This may be explained by the loss of medial collateral ligament integrity.
Intra-articular fracture, as in the capitellum, occurs occasionally, but osteochondral injuries are probably much more common than standard radiographs would lead one to suspect.18
Injuries at other sites are also common with elbow dislocations, occurring in approximately 12% of the cases.36,52,94 Fractures of the distal radius and the ulnar styloid, perilunar dislocations, and shoulder injuries of the same extremity are the most common of these injuries, with multiple injuries of other areas secondary to severe trauma accounting for the rest.
Neurovascular injuries occur with elbow dislocations just as with any other joint injury.69 Neurovascular compromise can also develop following the dislocation rather than during it.
ASSESSMENT AND TREATMENT OF ACUTE ELBOW INSTABILITY
ASSESSMENT OF STABILITY
On the basis of the aforementioned observations and interpretations, it can be recommended that posterior elbow dislocations be reduced in supination to clear the coronoid under the trochlea, thereby minimizing additional trauma to the medial soft tissues that have not yet been disrupted. Following reduction, instability isbest assessed with the patient under general anesthesia, but this is not always practical. It is indicated when there is any clinical or radiographic evidence for suspicion of persistent instability. The elbow is examined for valgus, varus, and posterolateral rotatory instability (Fig. 28-8). Forced pronation prevents instability by using the intact medial soft tissues as a hinge or fulcrum, just as the periosteum is used for this purpose during the reduction of a supracondylar fracture in a child. Both valgus and varus testing are performed with the elbow in full extension and several degrees of flexion up to about 30 degrees to unlock the olecranon from the olecranon fossa. Posterolateral rotatory instability is diagnosed by the lateral pivot-shift test of the elbow, which is described in the next section on recurrent instability and is described in detail in Chapters 47 and 48. A positive test is manifested by a clunk that is heard and felt when the ulna and the radius reduce on the humerus. With severe soft tissue disruption, the elbow can sometimes remain dislocated even when flexed past 90 degrees. The patient should be followed with sequential radiographs for any radiographic signs of instability. The drop sign is a key radiographic warning sign of elbow instability, and it indicates severe soft tissue disruption both laterally and medially and a propensity for persistent or recurrent instability.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree