Elbow Dislocation
EPIDEMIOLOGY
Elbow dislocation accounts for 11% to 28% of elbow injuries.
Posterior dislocation is most common, accounting for 80% to 90% of all elbow dislocations.
Annual incidence of elbow dislocations is 6 to 8 cases per 100,000 population per year.
Simple dislocations are purely ligamentous.
Complex dislocations are those that occur with an associated fracture and represent slightly less than 50% of elbow dislocations.
Highest incidence occurs in the 10- to 20-year-old age group and is associated with sports injuries; recurrent dislocation is uncommon.
ANATOMY
The elbow is a “modified hinge” joint with a high degree of intrinsic stability owing to joint congruity, opposing tension of triceps and flexors, and ligamentous constraints.
Three separate articulations are:
Ulnotrochlear (hinge)
Radiocapitellar (rotation)
Proximal radioulnar (rotation)
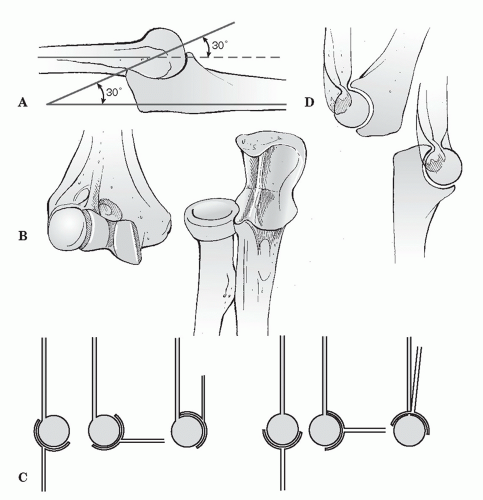
Stability (Fig. 18.1)
Anterior-posterior: trochlea-olecranon fossa (extension); coronoid fossa, radiocapitellar joint, biceps-triceps-brachialis (flexion).
The anterior joint capsule is also felt to play a role in ulnohumeral stability.
Valgus: The medial collateral ligament (MCL) complex
Anterior band is the primary stabilizer in flexion and extension.
Anterior capsule and radiocapitellar joint function in extension.
Varus: The lateral ulnar collateral ligament is static, and the anconeus muscle is dynamic stabilizer.
Function of the MCL
Primary medial stabilizer, especially the anterior band.
Full extension provides 30% of valgus stability.
Ninety degrees of flexion provides >50% of valgus stability.
Resection of anterior band will cause gross instability except in extension.
Lateral ligaments
Prevent posterior subluxation and rotation of the ulna away from the humerus with the forearm supination (posterolateral rotatory instability).
Normal range of motion: 0 to 150 degrees flexion, 85 degrees supination, and 80 degrees pronation.
Functional range of motion (ROM) requires: a 100-degree arc, 30 to 130 degrees flexion, 50 degrees supination, and 50 degrees pronation.
More recent reports suggest increased ROM is needed to perform contemporary activities of daily living such as talking on a cell phone or using a computer mouse and keyboard.
MECHANISM OF INJURY
Most commonly caused by a fall onto an outstretched hand or elbow, resulting in a levering force to unlock the olecranon from the trochlea combined with translation of the articular surfaces to produce the dislocation.
Posterior dislocation: This is a combination of elbow hyperextension, valgus stress, arm abduction, and forearm supination.
Anterior dislocation: A direct force strikes the posterior forearm with the elbow in a flexed position.
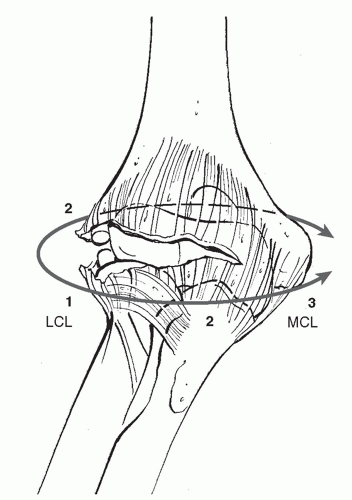
Most elbow dislocations and fracture-dislocations result in injury to all the capsuloligamentous stabilizers of the elbow joint. The exceptions include transolecranon fracture-dislocations and injuries with fractures of the coronoid involving nearly the entire coronoid process.
The capsuloligamentous injury progresses from lateral to medial (Hori circle) (Fig. 18.2); the elbow can completely dislocate with the anterior band of the MCL remaining intact. There is a variable degree of injury to the common flexor and extensor musculature.
CLINICAL EVALUATION
Patients typically guard the injured upper extremity, which shows variable gross instability and swelling.
A careful neurovascular examination is essential and should be performed before radiography or manipulation.
Following manipulation or reduction, repeat neurovascular examination should be performed to assess neurovascular status.
Serial neurovascular examinations should be performed when massive antecubital swelling exists or when the patient is felt to be at risk for compartment syndrome.
Angiography may be necessary to evaluate vascular compromise.
Following reduction, if arterial flow is not reestablished and the hand remains poorly perfused, the patient should be prepared for arterial reconstruction with saphenous vein grafting.
Angiography should be performed in the operating room and should never delay operative intervention when vascular compromise is present.
The radial pulse may be present with brachial artery compromise as a result of collateral circulation.
The absence of a radial pulse in the presence of a warm, wellperfused hand likely represents arterial spasm.
Medial ecchymosis, a sign of MCL disruption, is typically apparent 3 to 5 days after injury.
ASSOCIATED INJURIES
Associated fractures most often involve the radial head and/or coronoid process of the ulna. Shear fractures of the capitellum and/or trochlea are less common.
Acute neurovascular injuries are uncommon; the ulnar nerve and anterior interosseous branches of the median nerve are most commonly involved.
The brachial artery may be injured, particularly with an open dislocation.
RADIOGRAPHIC EVALUATION
Standard anteroposterior and lateral radiographs of the elbow should be obtained.
Congruence of the ulnohumeral and radiocapitellar joints should be assessed.
Radiographs should be scrutinized for associated fractures about the elbow.
Valgus stress views at 30 degrees elbow flexion and full forearm pronation, obtained after initial reduction or at surgery, may help identify an MCL injury.
Computed tomography (CT) scans may help identify bony fracture fragments not visible on plain radiographs.
CLASSIFICATION
Simple versus complex (associated with fracture)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree