Dysplasia in the Skeletally Mature Patient
Perry L. Schoenecker
Key Points
• Early diagnosis is essential to provide the opportunity for optimal hip preservation treatments.
• History, examination, and plain radiographs are the essential components of the diagnostic workup.
Introduction
Instability secondary to hip dysplasia frequently does not become symptomatic until skeletal maturity. A history of previous treatment may be reported, as in an infant or young child with closed reduction with an orthosis or a spica cast; more often, no history of previous awareness or treatment of hip dysplasia is noted. Once an unstable hip has become symptomatic in the skeletally mature patient, surgical correction of existing acetabular dysplasia is necessary to arrest progressive pathologic processes.
Differential Diagnosis
Patients presenting with hip pain can be classified into many different categories. One early distinction is the site of the pain. Lateral hip pain often can be caused by a trochanteric bursitis, which can be related to abductor dysfunction. Low back pain or radiculopathy can also be present or can manifest as lateral hip pain. Most intra-articular hip pathology presents as groin pain. Patients with limited range of motion and pain may suffer from impingement about the hip with a femoral side “cam” lesion, an acetabular side “pincer” lesion, or both. They tend to report pain with sitting in low chairs or in a car for an extended period of time. Patients with hip dysplasia (and no impingement) typically exhibit a normal range of motion. They describe pain more with activities, walking, or running. Patients with either condition may experience labral tears and may have mechanical symptoms. Certainly other causes of adult hip pain are known, such as infection (septic arthritis or osteomyelitis), tumor, metabolic disease, avascular necrosis, trauma, or general osteoarthritis independent of dysplastic development. After a careful history and physical examination are performed, diagnostic imaging with plain radiographs is the next step in narrowing a differential diagnosis for hip pain in the adult. Figure 34-1 outlines a general algorithm for assessment of hip pain in the young adult.1
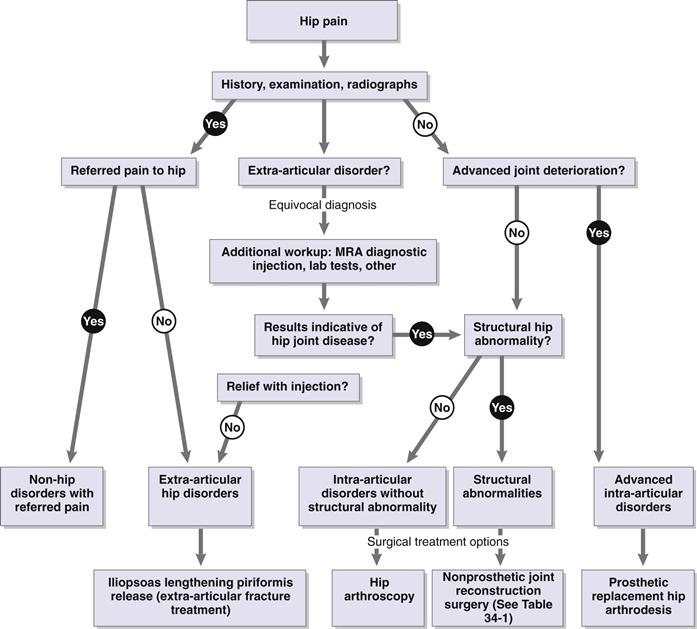
Figure 34-1 Algorithm for assessment and treatment of hip pain in the young adult. (Redrawn from Clohisy JC, Keeney JA, Schoenecker PL: Preliminary assessment and treatment guidelines for hip disorders in young adults. Clin Orthop Relat Res 441:168–179, 2005.)
Clinical Findings
History
Skeletally mature patients with symptomatic clinical instability secondary to hip dysplasia present with a history of variable hip pain and/or limp. This pain can be localized to various areas about the hip but primarily is reported as groin pain. The pain can be rather insidious, persisting for months to years before presentation. The pain is often accentuated with activity. A fatigue limp is often present. With this presentation, the pain initially may be localized to the hip abductors and/or the greater trochanter. This is attributed to lateralization of the hip center and increased load on the hip abductors. More active patients typically become symptomatic earlier in life given the same degree of dysplasia owing to increased demand placed on the hip. Other reports of mechanical symptoms such as catching, locking, or popping can accompany this, suggesting labral pathology or a chondral flap.
The level and character of pain, as well as its duration and associated symptoms, should be outlined; this can help in diagnosis and can guide treatment. Questions pertinent to hip joint function in daily activities used to calculate the Harris Hip Score are helpful for preoperative evaluation and can be used to assess the efficacy of treatment. Although typically used to evaluate outcomes of hip arthroplasty, this scoring system has also been used to assess hip preservation. Patients in studies of adult hip dysplasia treated with hip preservation techniques have preoperative scores that vary between 50 and 65 on a 100-point scale. If the patient had been treated as a child for hip dysplasia, a detailed history of childhood treatment, both nonsurgical and surgical, must be obtained.
Physical Examination
The first step in examining a painful hip is to evaluate the patient’s gait. Patients can present with an antalgic or a Trendelenburg gait. Patients with an antalgic gait may have significant labral pathology causing more acute pain or more involved degenerative changes from years of lateral point loading. Those with a Trendelenburg gait are exhibiting manifestations of a lateralized joint center and abductor weakness. If the hip joint is functionally unstable, the single-leg stance Trendelenburg test will be positive. Sometimes it is necessary to have the patient perform the test for several seconds. Occasionally, the patient will note reproduction of trochanteric hip pain while performing the Trendelenburg test.
Next, active and passive range of motion should be evaluated. Coupled with this is assessment of motor strength in the hip flexors, extensors, adductors, and abductors. Patients with pure acetabular dysplasia may have a normal passive range of motion. Occasionally, patients also have a femoral side osteochondral prominence or a cam-type lesion, leading to a positive impingement sign with the typical position of flexion, adduction, and internal rotation resulting in the reproduction of pain.
Radiographic Evaluation
Four standard radiographic views are helpful in evaluating dysplasia in the skeletally mature hip: a standing anteroposterior (AP) pelvis and false profile of both hips, a supine frog lateral, and a cross-table lateral2 (Fig. 34-2A through D). Additionally, a flexion, abduction, and internal rotation (Von Rosen) view can be added to show the coverage and congruence that can be obtained with pelvic and/or femoral osteotomies.

Figure 34-2 Normal examples of four initial radiographs taken in the evaluation of a young adult with a painful hip. A, Anteroposterior (AP) pelvis: beam centered between the pubic symphysis and the level of the anterosuperior iliac spine (ASIS), with both lower extremities in 15 degrees of internal rotation, to profile the proximal femur. B, Frog lateral: 45 degrees of hip abduction, 30 to 40 degrees of knee flexion, hip external rotation so that the sole of the foot faces the other leg. C, False profile (see Fig. 34-4A through C). D, Cross-table lateral. (From Clohisy JC, Carlisle JC, Beaule PE, et al: A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 90:47–66, 2008.)
The AP pelvis provides perhaps the most information on the shape and orientation of the acetabulum and offers a comparison with the contralateral hip. Figure 34-3 details the important lines and measurements taken from this radiograph. Shenton’s line, a curvilinear line connecting the obturator ring with the inferior border of the femoral neck, should be intact in a normal hip, and any discontinuity or irregularity is indicative of subluxation of the hip. A horizontal interteardrop line connecting the inferior aspect of the teardrop of each acetabulum provides a point of reference for further evaluation. This can serve as the reference for a parallel line drawn to connect the medial margins of the weight-bearing portion of the acetabular. The Tonnis angle, or acetabular index, is an angle created between this parallel line and its intersection with a second line outlining the weight-bearing portion of the acetabular dome. This angle should measure 0 to 10 degrees. Angles greater than 10 degrees indicate dysplasia. The AP pelvis x-ray also provides a measurement of the lateral center edge angle. This angle is created between a vertical line through the center of the femoral head and a line connecting the center of the femoral head with the lateral edge of the acetabulum. The center of the femoral head in a normal hip should be well medial to the lateral edge of the acetabulum, producing a lateral center edge angle of 25 degrees or greater. However, in a dysplastic hip, the femoral head may be subluxated and lateralized and/or the acetabular weight-bearing dome (the sourcil) relatively short with resultant decreased femoral head coverage. Another measure of femoral head coverage is the lateral head extrusion index. This is represented as a percentage of the femoral head, which lies lateral to the lateral border of the acetabulum. This serves not only as an indicator of the degree of dysplasia but also as a postoperative marker predictive of success for hip preservation osteotomies.3 The lateral center edge angle typically will be pathologically decreased, sometimes with a negative value (if the center of the head migrates lateral to the acetabulum). Direct measurement of hip joint lateralization relative to the pelvis can also be assessed on the AP view. A horizontal measurement in millimeters should be made from the ilioischial line to the medial aspect of the femoral head. This should be compared with the contralateral side if normal. An absolute value of less than 10 mm is considered normal.2 Finally, the relative length of the lower extremities can be indirectly assessed on the standing AP pelvis radiograph by observing (and measuring) any tilt of the pelvis. The presence of a leg length discrepancy can relatively uncover the hip on the side of the longer leg, potentiating the development of a low-grade dysplastic hip—a condition known as long leg arthropathy.

Figure 34-3 Standard anteroposterior (AP) pelvis radiograph with important landmarks/measurements: Shenton’s line, lateral center edge angle, Tonnis angle.
Another important radiograph in the evaluation of adult hip dysplasia is the false profile view. This view is obtained with the patient standing 25 degrees off axis from a true lateral of the pelvis, with the affected hip centered on the film (Fig. 34-4A through C). On this view, the anterior center edge angle is measured, indicating the amount of anterior coverage that the acetabulum provides over the femoral head. The angle is formed between a vertical line drawn through the center of the femoral head and a line between the center of the femoral head and the anterior edge of the articular surface of the acetabulum. This value should be greater than 20 degrees. Undercoverage indicates a dysplastic hip, whereas overcoverage seen as increasing values causes impingement.

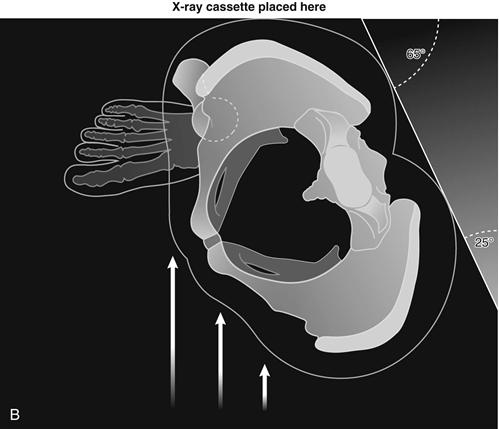
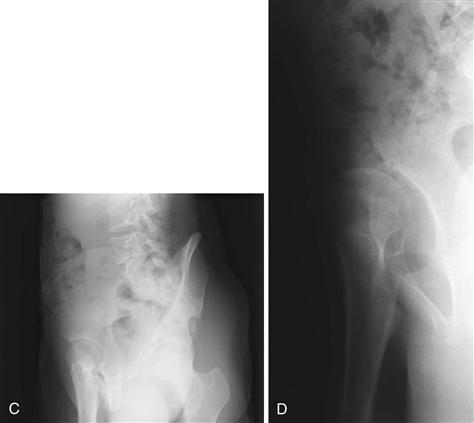
Figure 34-4 The false profile view. A, Patient is positioned standing with pelvis/torso rotated 25 degrees off the plane of a true lateral, producing a 65-degree oblique view of the imaged hip. The foot on the desired side is parallel to the cassette. B, Cross-sectional schematic of the same position. C, Example of a false profile view of a normal hip with measured anterior center edge angle. D, Example of a false profile view of a dysplastic acetabulum with anterior undercoverage. (Adapted from Clohisy JC, Carlisle JC, Beaule PE, et al: A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 90:47–66, 2008.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








