INTRODUCTION
Despite increased focus on injury prevention, as well as osteoporosis identification and management, distal radius fractures continue to be one of the most common injuries in clinical practice. They occur in a bimodal fashion with predictable peaks in the young and elderly. Many lower-energy nonarticular fractures and most epiphyseal fractures in children can be treated with closed reduction and casting with excellent outcomes. On the other hand, comminuted fragility fractures of the distal radius secondary to osteoporosis in the elderly may be easy to reduce but difficult to maintain in a cast after closed reduction. Similarly, fractures in younger patients as the result of higher-energy injuries often result in unstable fracture patterns that require surgery.
All displaced distal radius fractures should be reduced and splinted to correct gross deformity and improve the neurovascular status and relieve pain. Postreduction radiographs should be critically assessed for signs of instability. Lafontaine et al. (
1) proposed five factors that correlated with fracture instability: (a) initial dorsal angulation >20 degrees, (b) dorsal comminution, (c) radiocarpal intra-articular involvement, (d) associated ulnar fractures, and (e) age >60 years. In these authors’ experience, patients with three or more of these factors had a high incidence of loss of reduction with cast treatment alone. Nesbitt et al. (
2) used the Lafontaine et al. criteria and determined that age was the only significant risk factor in predicting instability. In patients over the age of 58 years, there was a 50% risk for secondary displacement, while patients over 80 years had a 77% increased risk. More recently, MacKenney et al. (
3) prospectively evaluated 4,000 distal radius fractures and identified age, metaphyseal comminution, and ulnar variance as risk factors for early or late instability. In addition to the loss of reduction, carpal malalignment and postreduction joint incongruity (articular step-off or fracture gap) have been shown to have a negative impact on functional outcome (
4,
5 and
6).
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
Closed reduction and casting is utilized for the majority of patients with fractures of the distal radius. Nonoperative management is indicated if after reduction the radial length is within 3 to 4 mm of uninjured wrist, the radial inclination is 22 degrees or more and articular step-off or gap is <2 mm. The carpus must be aligned with the radial shaft. Loss of the volar tilt should be no more than 10 degrees (
Table 13.1). Our philosophy has been to accept less deformity in younger, highly active patients, and to accept more deformity in the lower demand elderly osteoporotic patients. Minor degrees of shortening or angulation usually do not adversely affect clinical outcomes (
7,
8 and
9). After closed reduction follow-up, x-rays are obtained in the clinic every 7 to 10 days for the first 3 weeks to ensure maintenance of reduction and to assess the need for surgical intervention. The cast should not block full metacarpal phalangeal joint flexion and is continued for 6 weeks followed by a removable prefabricated splint. If finger motion is maintained, occupational therapy is not usually required. If stiffness or swelling persists, then supervised therapy is recommended.
Unstable and displaced fractures of the distal radius usually require surgical repair due to the latent instability of even well-reduced fractures. We believe that there is a subset of patients with acceptable initial reductions that might benefit from early surgery based on LaFontaine’s criteria who have a high likelihood of
redisplacement. In general, early surgery is recommended for most patients with volarly displaced fractures and in most patients with severe initial displacement, shortening, and dorsal comminution. Treatment decisions in this group of patients are individualized.
In the past decade, locking plates for internal fixation of unstable distal radius fractures have become widely available. These include anatomically designed plates for the volar, radial, and dorsal aspects of the radius, which are low profile and can be locked. The ability to lock the screws into the plate dramatically increases fixation stability even in patients with severe osteopenia. Both fixed angle and variable angle screw trajectories allow the surgeon to target and stabilize displaced articular facets. This has led to a dramatic and rapid change in surgical indications for unstable distal radius fractures. Locked plating of the distal radius fractures has virtually replaced the previous standard of spanning external fixation in North America. However, modern external fixation with either spanning or nonjoint spanning frames can achieve satisfactory outcomes when combined with K-wire augmentation and metaphyseal bone grafting, which supports the articular reduction in similar fashion to the subchondral screws of a volar locked plate.
In our practices, we have shifted almost completely to plating of distal radius fractures. However, there still are indications for augmented external fixation utilizing supplemental K-wire fixation for the highly comminuted distal radius fractures that are not amenable to internal fixation or when trying to prevent or treat infection or significant soft-tissue injury.
Strong Indications for External Fixation Include:
Highly comminuted and, at times, very distal intra-articular distal radius fractures not amenable to internal fixation
Contaminated grade II and III open fractures of the distal radius
Open fractures associated with bone loss
Open or closed fractures associated with neurovascular injuries requiring repair or massive soft-tissue injury
Highly unstable fractures associated with extrinsic ligament injuries such as volar lip-shearing type or ulnar translocation of carpus
Relative Indications for External Fixation Include
Widely displaced fractures with significant soft-tissue swelling, abrasions, or blisters
Multiply injured patients
Complex ipsilateral limb injuries
Infected wrist or forearm fractures
PREOPERATIVE PLANNING
History and Physical Examination
A thorough history and physical examination is essential with particular attention focused on the soft-tissue integrity and neurocirculatory examination of the extremity. The brachial, radial, and ulnar pulses should be palpated and/or dopplered. A careful neurologic exam of the extremity should assess the motor and sensory integrity of the radial, median, and ulnar nerves. This must be clearly documented. The skin should be inspected for the presence of open wounds including small wounds on the ulnar side of the wrist. Furthermore, the forearm and elbow should be checked for swelling and tenderness to rule out an associated Galeazzi, Monteggia, or an Essex-Lopresti injury. The forearm musculature should be palpated to rule out a frank or evolving compartment syndrome. The hand should also be examined for pain or deformity, which might indicate a combined injury such as a carpal or metacarpal fracture or dislocation. Patient-specific information, hand dominance, occupational requirements, medical comorbidities, and expectations often guide treatment recommendations. Once the physical examination has been completed, a closed reduction of the fracture and a sugar-tong or long-arm splint should be applied. The wrist should not be placed in a “hyper-flexed” posture that might increase pressure in the carpal canal. Any signs or symptoms of increasing pain or paresthesias mandate that any splints or cast be loosened or removed for a more precise evaluation and treatment. Osteoarthritic fingers are especially vulnerable to postfracture swelling and pain. Acute tendon injuries are rare following closed distal radius fractures.
Imaging Studies
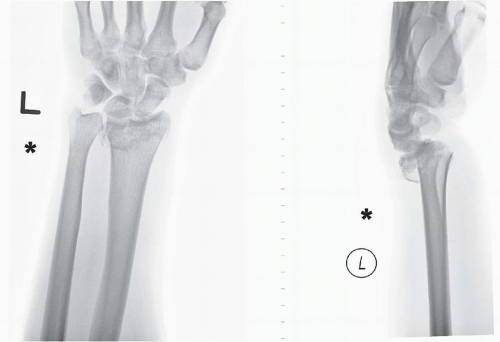
High-quality anteroposterior (AP) and lateral radiographs of the wrist and entire forearm must be obtained. In some cases, comparative contralateral wrist films are helpful. Postreduction radiographs often clarify the fracture pattern and help determine fracture stability. In comminuted or complex fracture patterns, CT scans with axial, coronal, and sagittal reconstructions can be useful to better clarify the fracture pattern and morphology. CT scans should only be obtained after the fracture has been reduced and splinted. Scans done with the fracture shortened, displaced, and angulated rarely provide useful information and waste health care resources. For selected unstable fractures, fluoroscopic traction views can also provide useful information about facet displacement and may determine or alter the surgical approach. Traction films can also reveal subtle, combined, carpal bone, and/or ligamentous injury.
Timing of Surgery
Unstable closed fractures of the distal radius without neurovascular compromise require timely but thoughtful intervention. Surgery should be scheduled semielectively following reduction and splinting. Open fractures, on the other hand, require urgent irrigation, débridement, and stabilization. All patients with compartment syndromes or acute carpal tunnel syndrome require emergent decompression.
In a subset of patients following closed reduction, there is redisplacement on follow-up radiographs. Patients treated nonoperatively should be followed weekly for 21 days to monitor this potential redisplacement. We caution against a “slippery slope” phenomenon whereby a small amount of displacement is accepted at 1 week and a bit more at 2 weeks followed by a grossly unacceptable reduction at 3 or 4 weeks. If there is more than 2 to 3 mm of displacement on follow-up radiographs, surgery is recommended.
Treatment Paradigm
The definitive treatment plan is based upon fracture stability, patient expectations, functional requirements, and medical comorbidities. Significant alterations in radial length, radial inclination, and reversal of palmar tilt have been correlated with less favorable results. These outcomes are worsened with articular incongruity and carpal subluxation (
4,
5 and
6). However, mild or even moderate degrees of deformity do not preclude a satisfactory result, increasing the importance of individualizing treatment. All patients with a displaced distal radius fracture should have a closed reduction and application of a sugar-tong splint or split long-arm cast. We use either an intravenous Bier block or a fracture hematoma injection. If a hematoma block is used, it is important to also inject the ulnocarpal joint to improve patient comfort when there is an ulnar styloid fracture or concomitant ligament injury. Unstable fractures are treated with surgery. In most cases, it is better to perform primary osteosynthesis rather than corrective osteotomy.
Unstable distal radius fractures should not be treated with joint-spanning external fixation alone (
Fig. 13.1). Outcomes are improved with adjunctive techniques such as Kapandji dorsal intrafocal pinning, transradial styloid-intramedullary pinning, and metaphyseal grafting with allograft or calcium phosphate bone cement (
10,
11) (
Fig. 13.2). In minimally comminuted fractures, with sufficient distal fragment bone stock, nonspanning external fixation may be preferable, as it allows better control in restoring radial length, inclination, and palmar tilt (
12). Dorsal or volar shear fractures, such as Smith’s and dorsal or volar Barton’s, should be treated with a locked buttress plate. Occasionally, in highly comminuted fractures, a bridging frame is used as an adjunct to an open reduction and internal fixation (
Fig. 13.3). This can be helpful with the small volar or dorsal pericapsular shear fractures associated with carpal instability. Scaphoid or lunate die-punch injuries should be treated with elevation of fragments and subchondral bone grafting stabilized with K-wire fixation. This can be performed with arthroscopic assistance or via fluoroscopic guidance (
10) (
Fig. 13.4).


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access






