Fig. 13.1
The articular end of the radius slopes in an ulnar and palmar direction. The carpus will thus have a natural tendency to slide in an ulnar direction, resisted for the most part by the intracapsular and interosseous carpal ligaments arising from both the radius and the ulna
13.3 Classification
The most complex and often used classification is that of the AO. Type A fractures are extraarticular, B are partial articular, and C are complete articular fractures. The A 1 fractures are extraarticular fractures of the ulna with an intact radius and they increase in severity from A 1.1 to A 1.3 [17] (Fig. 13.2).
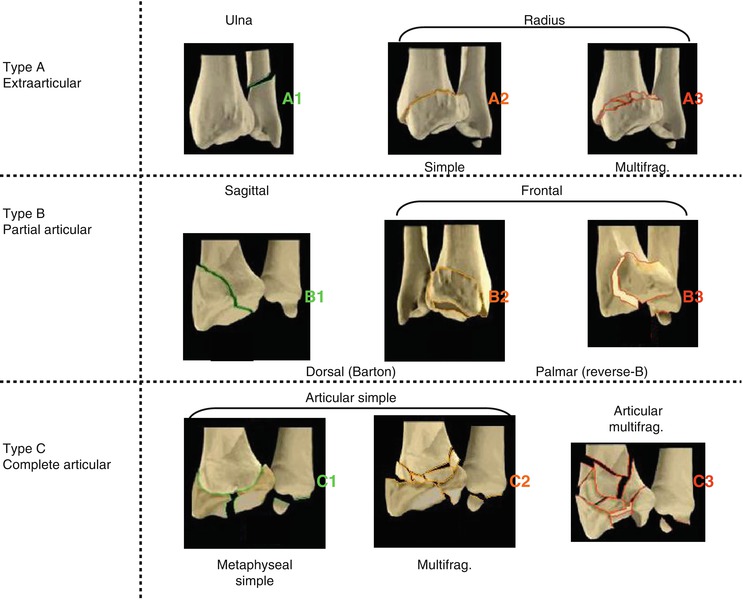
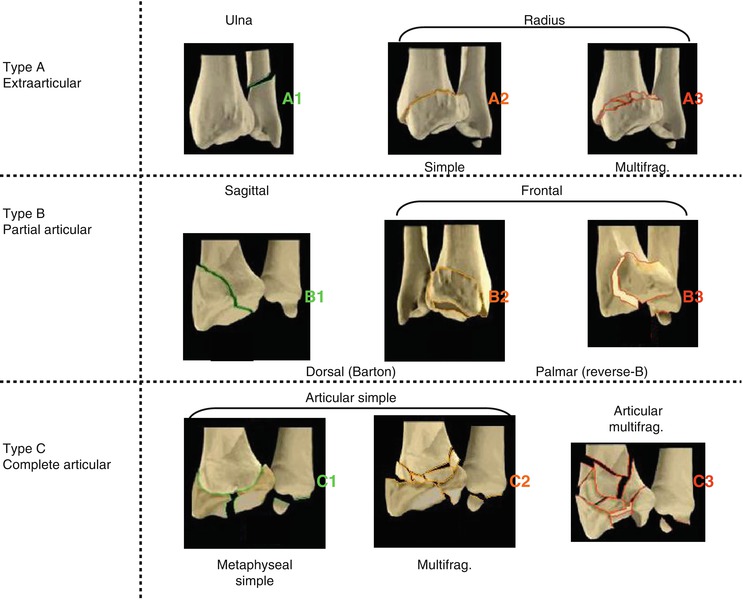
Fig. 13.2
AO classification of distal radius fractures
The A 2 fractures are extraarticular, either undisplaced A 2.1, with dorsal tilt A 2.2 or with volar tilt A 2.3. Any extraarticular fractures with metaphyseal comminution falls into the A 3 group, with increasing comminution from A 3.1 to A 3.3, with A 3.3 fractures being those with comminution extending into the diaphysis. The A 3.2 fracture is the typical Colles’ fracture with metaphyseal comminution.
The B type are partial articular. The B 1 fractures are sagittal fractures of the radius (B 1 is the styloid process fracture), B 2 are fractures of the dorsal rim, and B 3 affect the volar rim [17].
The C fractures are complete articular where the articular surface is fractured and totally separated from the metaphysis. C 2 fractures are simple articular with metaphyseal comminution, and C 3 fractures are the most complex, with multiple articular fracture lines and increasing metaphyseal comminution. Additionally, there are several classification systems only for intraarticular fractures. Melone described four possible parts: the radial shaft, the radial styloid, and the dorsal and volar portions of the lunate facet, which he termed the medial complex. Type 1 injuries are stable and type 2 occur when the radial styloid splits from the intact medial complex. Type 3 injuries are like type 2 but with a volar spike, which may damage the soft tissue. Type 4 injuries occur when, along with other features, the dorsal and volar parts of the medial complex are split. In 1993, Melone added a type 5, which he described as an explosion injury with severe articular comminution [15] (Fig. 13.3).
Fig. 13.3
Classification of intraarticular fractures according to Melone. 1 radial shaft, 2 radial styloid, 3 dorsal medial fragment, 4 palmar medial fragment. The medial fragments ande their strong ligamentous attachments with the proximal carpal bones and the ulnar styloid have been termed the “medial complex “ by Melone
13.4 Mechanism of Injury
A fall on an extended hand is the classical cause of distal radius fractures. The force of the body weight is transmitted through the carpus directly to distal metaphysis, where the cortex is thinnest.
13.5 Diagnostic Features
Besides pain and swelling, the typical bayonet or fourchette position is often seen. There is a possibility of concomitant injuries such as scaphoid fractures, SL ligament lesions, and radial head fractures.
13.5.1 Radiology
Plain radiographs remain the mainstay in diagnostics. The posteroanterior view (PA) obtained in neutral variance as well as a lateral view with a beam that is inclined 20° will assess ulnar variance and effectively visualize the articular surface. A 45° pronated oblique view is helpful in that it profiles the dorsal ulnar cortex and lends insight into this biomechanically important region. Sometimes, improved fracture visualization through computed tomography is valuable (Fig. 13.4). A high number of fractures classified as extraarticular by standard radiographs are revealed to be intraarticular injuries. Special angles and lengths characterize the fracture pattern [7, 24].


Fig. 13.4
CT gives information about step in the articular surface and SL lesion
13.5.1.1 Radial Length (Fig. 13.5a)
Fig. 13.5
The radial length (a) (height) averages in the frontal plane 11–12 mm in reference to the distal radioulnar joint 1. Line tangential to the top of the radial styloid and perpendicular to the long axis of the radius 2. Line perpendicular to the long axis of the radius and tangential to the ulnar head. The ulnar inclination (b) is measured from a coronal view as the angle between a line connecting the most distal points of the radial and rims of the articular surface and a perpendicular to the long axis of the radius. The palmar tilt or inclination (c) is measured from a sagittal view as the angle between a line connecting the most distal of the dorsal and palmar rims of the articular surface and perpendicular to the long axis of the radius
Radial length is measured on the a.p. radiograph. This measurement (in millimeters) represents the distance between a line drawn at the tip of the styloid radial process, perpendicular to the long axis of the radius with a second perpendicular line at the level of the distal articular surface of the ulnar head. The normal length is 10–12 mm.
13.5.1.2 Radial Slope
In the frontal view, the slope or inclination of the distal end of the radius is represented by the angle formed by a line drawn from the tip of the radial styloid process to the ulnar corner of the articular surface of the distal end of the radius and a line drawn perpendicular to the longitudinal axis of the radius. The average inclination is between 22° and 23° (Fig. 13.5b).
13.5.1.3 Palmar Inclination
To obtain the palmar inclination of the distal radius in the sagittal view, a line is drawn connecting the most distal point of the dorsal and volar cortical rims. The angle that this line creates with a line drawn perpendicular to the longitudinal axis of the radius reflects the palmar inclination. This angle has an average inclination between 10° and 12° (Fig. 13.5c).
13.5.1.4 Ulnar Variance
The vertical distance between a line parallel to the articular surface of the ulnar head and a line parallel to the proximal surface of the lunate facet of the distal radius has been referred to as the ulnar variance. The ulnar head and the medial corner of the radius are normally at the same level bilaterally.
With fracture displacement, the ulnar head will commonly be in a distal relationship (positive variance).
13.5.1.5 Radial Width, Shift
This width is the distance in mm from the most lateral tip of the radial styloid process to the longitudinal axis through the center of the radius on the a.p. radiograph.
13.6 Conservative Treatment
While clinical practice guidelines are not able to recommend one form of treatment over another, there has been a rise in surgical treatment of distal radius fractures [10, 27].
13.6.1 Reduction
Many fractures are simply reduced by traction. Classically, dorsal bending fractures are reduced by applying longitudinal traction, palmar flexion, ulnar deviation, and pronation. Another reduction technique introduced the concept of multiplanar ligamentotaxis, in which longitudinal traction is combined with palmar translation. Palmar translation creates a moment force in which the capitate will rotate the lunate palmarily. This, in turn, will produce a rotatory force that can effectively tilt the distal radial fragment in a palmar direction. Radioulnar translation is advocated to realign the distal fragments with the radial shaft.
13.6.2 Immobilization
The immobilization technique by L. Böhler [4] is based on the concept of a three-point cast.
Displaced but intrinsically stable extraarticular dorsal bending fractures can be effectively maintained initially in a sugar tong splint followed by a below-elbow immobilization, provided care is taken to apply appropriate molding of the cast [22]. Cast immobilization carries with it concerns regarding restricted range of motion, muscle weakness, and long-term disability [19].
13.6.2.1 Duration of Immobilization
Most well-reduced extraarticular dorsal bending fractures will heal by 4–5 weeks postinjury.
13.6.3 X-Ray Control
After 48 h, 7 days, 14 days, and 28 days, X-ray controls are recommended for conservative treatment.
The reasons are to avoid malunion resulting from secondary displacement, either by a second reduction and conservative treatment or by changing the procedure from conservative to operative management.
13.7 Operative Technique
13.7.1 Indications and Contraindications of Operative Treatment
Because of a high degree of secondary displacement and malunion, sympathetic reflex dystrophy, and other complications after conservative treatment, a change to operative treatment of displaced distal radius fractures has happened (Table 13.1).
Table 13.1
The treatment of distal radius fractures has changed to internal fixation. The indication, the surgical approach (palmar, dorsal, combined palmar and dorsal) and the choice of implants must be based on patients history, pathomechanics of the fracture, fracture pattern (x-ray), bone quality and the demands of the individual patient
A2 | Angle stable plate | K-wire |
A3 | Angle stable plate | K-wire |
B1 | Screw Fixation | (Lag screw) |
B2 | Angle stable plate | |
B3 | Angle stable plate | |
C1 | Angle stable plate | |
C2 | Angle stable plate | |
C3 | Ext. Fix and K-wires, Angle stable plate |
Open reduction of articular fractures of the distal radius is indicated when intraarticular congruity of the fracture cannot be achieved by closed manipulation, joint distraction, or percutaneous reduction maneuvers in manually active patients with good bone quality and absence of preexisting wrist pathology. Open reduction and internal fixation is also indicated in open fractures and in fractures with associated carpal disruption and tendon or nerve injuries because immediate skeletal stability is a prerequisite for undisturbed soft tissue healing. Delayed open reduction may be indicated for secondary intraarticular displacement in a fracture that undergoes loss of reduction after a conservative trial with closed reduction and plaster fixation. Articular fractures in elderly inactive patients and those with massive osteoporosis indicate open reduction and fixation with angular stable plates. Contraindications, not related to the fracture itself, may include the general condition of the patient, associated diseases, and the presence of degenerative changes of the wrist joint prior to injury (e.g., nonunion of the scaphoid, Kienböck’s disease, rheumatoid arthritis). Operative treatment might be contraindicated in unreliable, unmotivated, and noncooperative patients.
13.7.2 K-Wire Fixation
The method of Willenegger [26] is based originally on the description of Lambotte.
13.7.2.1 Reduction
A tourniquet should be applied if limited or formal open reduction becomes necessary. With the image intensifier properly draped, a classical closed manipulation with traction, palmar flexion, and ulnar deviation is performed. The quality of reduction is assessed under fluoroscopy, while traction is maintained by the surgeon and countertraction by the assistant. Alternatively, horizontal longitudinal traction can be applied using sterile finger traps with 2.5–5 kg weights and countertraction across the upper arm. This frees both the surgeon’s hands for manipulation and pinning.
13.7.2.2 Surgical Technique
An open or closed procedure is possible. The advantage of the open procedure is the identification of superficial radial nerve by a 2 cm incision over the styloid process. After identification of the nerve and closed reduction, three 1.8mm K-wires are inserted via the tip of the styloid process into the distal fragment. The pins should cross in both planes. An additional forearm cast is necessary. Implant removal usually is performed after 6 weeks (Fig. 13.6).


Fig. 13.6
A3 Fracture K-wire fixation. Crossing wires in both planes
13.7.2.3 Principles of Intrafocal Pinning and Surgical Technique
Traditionally, fractures of the distal end of the radius were fixed, after manual reduction, with pins drilled through the distal fragment and pinned into the proximal one. Quickly, because of the pins’ flexibility, the distal fragment moves back until the pins bump into the inferior edge of the proximal fragment.
In the original method of intrafocal pinning, a smooth K-wire is inserted after a manual reduction, through a short skin incision, directly into the fracture line [12, 13] (Fig. 13.7). In this way, any subsequent tilt of the distal fragment is prevented. Secondary displacement is made impossible by the immediate contact of the distal fragment with the pins, which are working as an abutment, not as a resistance component. Additional cast immobilization is not necessary with this technique, allowing immediate rehabilitation and, therefore, better functional results [23]. A good fixation needs three pins, inserted at precise points. The first pin is pushed laterally between the tendons of the extensor carpi radialis and that of the extensor pollicis brevis; the second pin is inserted postero-laterally, close to Lister’s tubercle, and, taking great care to avoid the extensor pollicis longus, the third is postero-medially set, passing between the extensor digitorum tendons and the extensor carpi ulnaris tendon. Clearly, this approach needs to avoid the tendons.
Fig. 13.7




Intrafocal pinning (Kapandji). This technique remains most effective in those unstable fractures without substantial volar comminution.3 pins (a) are placed into the fracture line, functioning to help reduce the fracture as well as to provide an internal splint, under reduction the pins (b) are directed approximately at a 45° angle to the long axis of the radius and driven to the intact proximal cortex.The pins (c) are located between ext carpi rad. and ext. pollicis brevis, between ext. pollicis longus and ext. indicis and between ext. digit. and ext carpi ulnaris tendons
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








