Distal Metaphyseal Osteotomies in Hallux Abducto Valgus Surgery
Thomas J. Chang
As early as 1881, Reverdin introduced the concept of addressing hallux abducto valgus deformity at the level of the metatarsal head (1). Over time, the distal osteotomies have become the most commonly performed type of bunionectomy, most likely for several reasons. First, most of the procedures afford immediate or early return to functional weight bearing because of the inherent stability of the osteotomy. This basic tenet simplifies the postoperative management period and may reduce the risks associated with patient noncompliance compared with other osteotomy designs. Second, modifications in the techniques allow for multiplanar correction to address various levels of deformity in the transverse, sagittal, and frontal planes, as well as the metatarsal length.
Historically, distal metaphyseal osteotomies have been considered in patients with mild to moderate hallux valgus deformity with an intermetatarsal (IM) angle up to 15 degrees. However, some investigators have reported the ability of certain distal osteotomies to correct IM angles of up to 20 degrees (2, 3, 4, 5). In addition, distal osteotomies may be employed to correct deviations in the proximal articular set angle (PASA). Concomitant hallux limitus can also be addressed with several of the osteotomy designs.
Because of the significant benefits to the distal metaphyseal osteotomies, many investigators have considered these osteotomies as “universal” procedures. As a general statement, the distal procedures are considered technically easier to perform than the more proximally oriented procedures. However, patients with significant deformity, metatarsus adductus, or other conditions are still well served with proximal repair procedures.
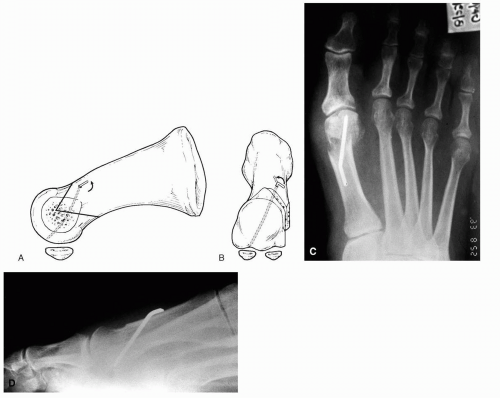
TECHNIQUE: APICAL AXIS GUIDE
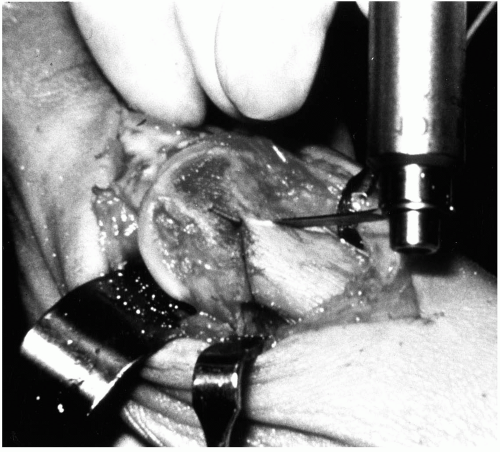
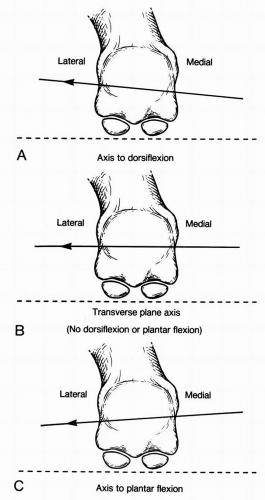
The axis guide concept was first introduced by The Podiatry Institute in 1980 (3). The guide is simply a Kirschner wire (K-wire) used for reconstructive surgery of the foot and ankle to help guide the angles and planes of the osteotomy being performed. Once the guide is in place, the surgeon simply needs to maintain the saw blade parallel to the axis guide for a well-executed cut. A Reese osteotomy guide placed on the axis guide can also be employed to assist in the execution of the osteotomy, but it is not necessary. The Reese osteotomy guide also relies on the concept of proper axis guide placement to work properly (Fig. 1). In hallux valgus correction, use of the axis guide can assist the surgeon in manipulating and executing an accurate osteotomy. This concept allows a K-wire to be placed from medial to lateral through the metatarsal head to help plan the actual direction of the capital fragment before the osteotomy is cut (6). The most common planes of manipulation are the sagittal and transverse planes (Fig. 2). Simple placement of the axis guide readily assists in manipulation of the (a) sagittal plane placement (plantarflexion) and (b) metatarsal length.
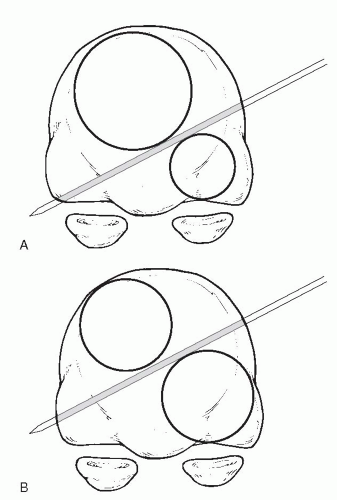
The apex of the osteotomy is usually selected as the central point of the metatarsal head medially after resection of the medial eminence. Depending on the angular manipulations desired, it is recommended to expand the cuts from the central point when necessary to create even segments of bone both above and below the apex (Fig. 3). This is most important in sagittal plane manipulations. For example, plantarflexion of the capital fragment is commonly selected for hallux valgus correction. Therefore, the axis guide is directed from dorsal medial to plantar lateral. If the wire enters centrally on the medial side of the metatarsal, then the osteotomy will exit the lateral cortex at a more plantar oriented position. Consequently, depending on the amount of plantarflexion desired, one may adjust the axis guide to enter the medial head above the central point. If dorsiflexion of the capital fragment is desired, then the medial entry of the pin may be below the midpoint medially and may exit above the midpoint laterally.
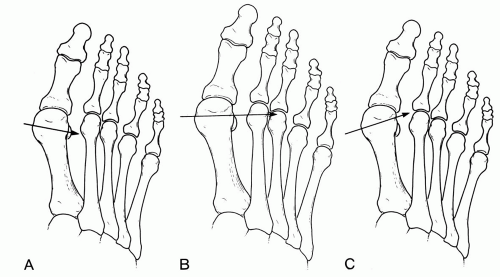
Manipulation of the metatarsal length can also be achieved using an apical axis guide pin (Fig. 4). Usually, the metatarsal is either shortened slightly or the length is maintained. Actually, the width of the power saw and normal bone resorption during healing result in some shortening of the bone. The relative length of the first metatarsal is usually measured with respect to the second metatarsal; similarly, the K-wire is delivered with respect to the second metatarsal as a reference. Again, the midpoint of the head is estimated, and the wire is driven from medial to lateral. To maintain length, the wire is driven perpendicular to the second metatarsal shaft. If shortening is desired, then the K-wire is directed in a slightly proximal position.
The foregoing comments apply well to an Austin-type
osteotomy, but the general concepts can also apply to most other distal osteotomies. The surgeon performs the osteotomy with the saw blade parallel to the axis guide. Any deviation of the blade from the pin causes the osteotomies to converge or diverge laterally and may compromise proper seating of the capital fragment.
osteotomy, but the general concepts can also apply to most other distal osteotomies. The surgeon performs the osteotomy with the saw blade parallel to the axis guide. Any deviation of the blade from the pin causes the osteotomies to converge or diverge laterally and may compromise proper seating of the capital fragment.
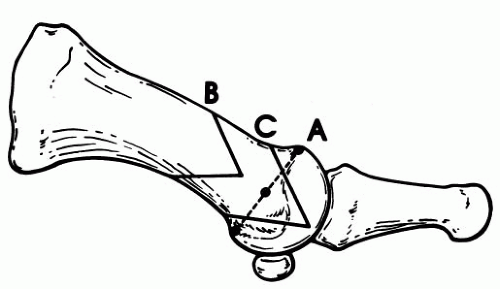
AUSTIN BUNIONECTOMY
Austin first performed this procedure in 1962 (Fig. 5) (7). The Austin bunionectomy is described as being inherently stable with the ability to correct an IM angle of up to 15 degrees, although authors have reported the ability to correct IM angles up to 22 degrees (2, 3, 4). The osteotomy is “V” shaped and is oriented from medial to lateral with the apex distally and two arms of the osteotomy exiting the proximal cortex. The apex is usually considered to be the central point of the medial metatarsal head. This point can be estimated by visualizing a line from the proximal extent of the dorsal cartilage to the proximal extent of the plantar articular surface. The midpoint of this line often provides a good location for the apex of the osteotomy. If the apex is positioned too proximally, then the osteotomy will be located within the diaphyseal portion of the metatarsal, more closely approximating the offset-V procedure. If the apex is placed too far distally, it will increase the chance of an intraarticular fracture (Fig. 6). The osteotomy is usually performed with an
angle of approximately 60 degrees between the dorsal and plantar segments.
angle of approximately 60 degrees between the dorsal and plantar segments.
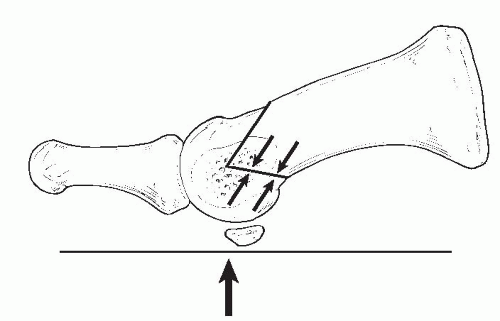 FIG. 5. Traditional Austin osteotomy angulated at 60 degrees. The inherent stability of the osteotomy results from the weight-bearing compression across the plantar arm. |
After the osteotomy is completed, lateral transposition of the capital fragment is executed. When the position of the capital fragment is deemed to be acceptable, impaction of the fragment provides early stability before fixation is introduced. This maneuver is performed by applying even proximal pressure against the entire width of the metatarsal head with one hand while stabilizing the metatarsal shaft with the other. When mild PASA deviations may exist, this can be addressed by more direct impaction on the medial half of the capital fragment to derotate the articular surface. This approach is helpful in repositioning the capital fragment with the articular surface directed in a more rectus or medial position. After initial stability is imparted to the capital fragment, then fixation may be introduced.
Results
Austin first performed this procedure in 1962 and reported his results in 1965 on 300 patients (7). In his early review, he reported 10% of recurrence of the bunion and only a few cases of hallux varus. When Austin and Leventen presented their “new” osteotomy in 1981, they had performed more than 1,200 procedures (7). An interspace release was performed from an intracapsular approach, and these investigators believed that impaction of the capital fragment provided enough stability to the osteotomy site without fixation.
Johnson et al. described their experience with a similar chevron osteotomy at the Mayo Clinic starting in 1976, with an article on their follow-up on 18 patients published in 1979 (8). Their approach was identical to that of Austin and Leventen, but it also included an occasional bone peg fashioned from the resection of the medial metatarsal shaft across the osteotomy site for added stability. Johnson et al. reported a 7-degree average decrease in the IM angle and an average of 12-degree correction of the hallux abductus angle.
In 1993, Hetherington et al. reported a follow-up study on the Austin bunionectomy to address the following issues: (a) long-term results of the Austin for hallux abducto valgus correction; (b) reproducibility of these results; (c) efficiency of capsular reefing to enhance results; and (d) comparison of fixated versus nonfixated osteotomies (9). They compared several groups of patients in four categories. The first two categories were a follow-up of 18 nonfixated Austin osteotomies performed by one of the primary authors. Group 3 procedures were performed with capsular reefing, and group 4 procedures were performed with K-wire fixation. Their conclusions were as follows: (a) long-term results appeared to be good and reproducible; (b) capsular reefing did not appear to improve results—an increase in joint stiffness and metatarsalgia was noted in this group; and (c) no difference was noted among the fixation techniques used.
Modifications
Since its introduction, certain modifications have been made to the original Austin design in an attempt to use this osteotomy as a universal procedure for correction of many conditions involving the first metatarsal. The modifications have allowed more dynamic manipulations in the transverse and sagittal planes to emphasize different aspects of correction or fixation.
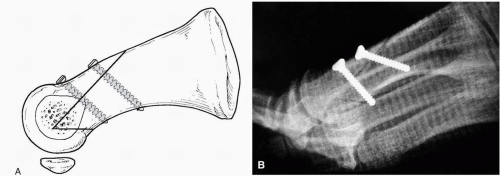
Long Dorsal Arm
A longer dorsal arm was employed under the premise that this would provide more stability to the capital fragment and would obviate the need for fixation. The more acute angulation of the osteotomy necessary to create the longer dorsal arm was reported to reduce some of the problems seen with the traditional design. This difference provided shorter postoperative immobilization and more rapid return to normal footwear (10). Some investigators have described favorable results with the modification (11, 12, 13, 14), although fixation is typically employed by most surgeons, in contrast to the original report (Fig. 7). In fact, the longer dorsal arm provided an excellent means of stabilizing the osteotomy with two dorsally to plantarly oriented screws (11). Two points of fixation are important in providing transverse plane rotational stability to the capital fragment. With these new modifications, surgeons began to extend the limits of the traditional Austin osteotomy to more aggressive levels. The modified osteotomy has been reported as successful in addressing patients with IM angles of 20 to 22 degrees (2) (Fig. 8). The screw fixation techniques also allow the capital fragment to be translocated up to one-half of the metatarsal width.
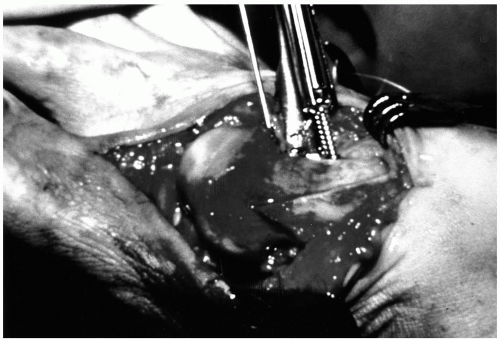
The dissection for the longer dorsal arm is slightly different, owing to the forms of fixation most commonly employed for stabilization. The dorsal synovial fold is typically dissected from the metatarsal head. Fixation of the long arm osteotomy is usually achieved with two parallel screws oriented perpendicular to the osteotomy site. In some instances,
threaded K-wires have also proven suitable. Two 2.7-mm AO screws are most commonly used, or sometimes a 2.0-mm screw is employed as the proximal anchor. A 0.045-inch K-wire is used for temporary fixation across the extremely distal portion of the dorsal arm of the osteotomy, directed from dorsal distal to plantar proximal, exiting proximal to the plantar arm of the osteotomy. The guide pin may also be used as a reference for the orientation of the screws (Fig. 9). The initial holes for the screws are on the dorsal cortex of the capital fragment and are often created with a 0.062-inch K-wire. Smith described identifying the dorsal position of the screws with either a marker or drill holes before making the osteotomy to ensure adequate bone surface for fixation (15). With the temporary fixation pin in place, a 0.062-inch K-wire is introduced in the location of the proximal screw and is driven parallel to the temporary fixation wire. With these two wires in place, the distal screw is inserted across the osteotomy site, parallel to the two K-wires (Fig. 10).
threaded K-wires have also proven suitable. Two 2.7-mm AO screws are most commonly used, or sometimes a 2.0-mm screw is employed as the proximal anchor. A 0.045-inch K-wire is used for temporary fixation across the extremely distal portion of the dorsal arm of the osteotomy, directed from dorsal distal to plantar proximal, exiting proximal to the plantar arm of the osteotomy. The guide pin may also be used as a reference for the orientation of the screws (Fig. 9). The initial holes for the screws are on the dorsal cortex of the capital fragment and are often created with a 0.062-inch K-wire. Smith described identifying the dorsal position of the screws with either a marker or drill holes before making the osteotomy to ensure adequate bone surface for fixation (15). With the temporary fixation pin in place, a 0.062-inch K-wire is introduced in the location of the proximal screw and is driven parallel to the temporary fixation wire. With these two wires in place, the distal screw is inserted across the osteotomy site, parallel to the two K-wires (Fig. 10).
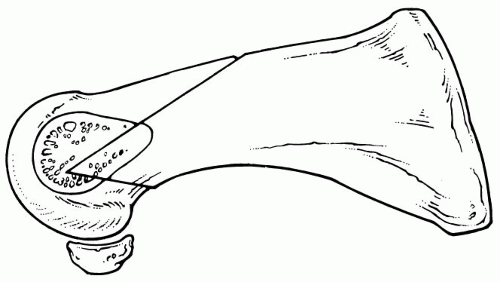 FIG. 7. Modified osteotomy (Kalish modification) with the angle measuring 55 degrees. This facilitates bicortical screw fixation across the dorsal arm of the osteotomy. |
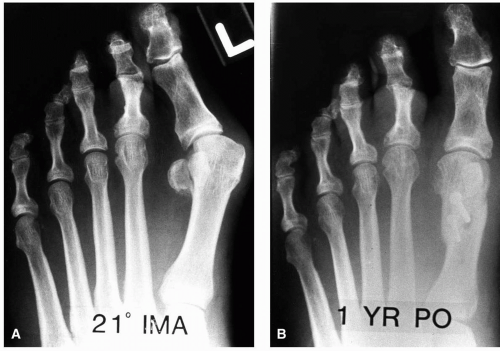 FIG. 8. A: Preoperative radiograph of a patient with a 21 -degree intermetatarsal angle. B: Postoperative radiograph at 1 year after the Kalish procedure, with good alignment noted. |
The two points of temporary fixation provide rotational stability to the capital fragment while the first screw is applied. After the first screw is secure, then the proximal wire is removed, and the second screw is placed into this hole. Again, two points of stability are provided by the temporary 0.045-inch wire and the first distal screw. With the oblique direction of the screws, it is possible for the screws to slide proximally along the plantar cortex of the metatarsal and to compromise stable fixation across the osteotomy (Fig. 11). Complications have been noted infrequently and have most often consisted of hallux varus (3%), fracture of the dorsal arm (2%), and stress reaction of the lesser metatarsals resulting from weight transfer (1%) (13,14).
Long Plantar Arm
A long plantar arm modification of the Austin osteotomy has also been described (16). The angle approaches 55 degrees, with the plantar arm exiting more proximally. Fixation is most often accomplished with two points of fixation across the plantar arm. Two 2.7- or 2.0-mm screws are usually employed. In addition, resection of a medially based wedge for PASA correction may be performed if necessary. One needs to ensure that the proximal extent of the plantar arm of the osteotomy is sufficiently long to avoid compromise of the sesamoid articulation with the fixation. Good results have been reported with this modification with few complications (16,17).
Youngswick Modification
Youngswick first described a modified osteotomy for addressing hallux valgus or hallux limitus (18). The procedure consists of the resection of a rectangular wedge of bone from the dorsal arm of the traditional Austin osteotomy. Removal of this segment of bone causes the capital fragment to seat more proximally on the first metatarsal shaft and to shift plantarly along the plantar arm of the osteotomy (Fig. 12). The amount of plantarflexion can be adjusted by varying the orientation of the plantar arm. A more vertically oriented plantar arm results in more plantarflexion of the capital fragment, but it also reduces stability as the angle of the osteotomy increases. A significant benefit of the procedure is the decompression of the first metatarsophalangeal joint, which should improve outcomes in patients with hallux limitus with or without concomitant hallux abducto valgus deformities. Lateral transposition of the capital fragment can simultaneously correct the transverse plane deformity.
Bicorrectional and Tricorrectional Osteotomies
The Austin osteotomy can also be modified to correct for deviations of the PASA (19,20). The procedure involves removal of a medially based wedge of bone from proximal aspect of both the dorsal and plantar segments to realign the articular surface. This procedure is technically more difficult because of the obliquity of the dorsal and plantar cuts. Successful fitting of the osteotomy is facilitated by initially cutting across only 80% across the osteotomy site to remove the wedges that are required. This maneuver provides stability to the capital fragment before the surgeon cuts through the lateral cortex (20). Lateral transposition of the capital fragment may then be performed to achieve reduction of the IM angle.
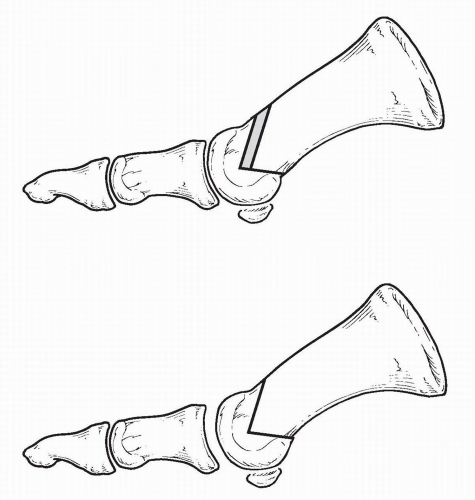 FIG. 12. Template of a Youngswick-Austin modification. Note the ability to decompress the first metatarsophalangeal joint while also achieving plantarflexion of the capital fragment. |
A “tricorrectional” bunionectomy has also been described (21). The V osteotomy is made through the metatarsal head from a dorsomedial to a plantar lateral direction.
Then a second V osteotomy is performed on the proximal segment removing a medially based wedge to reduce the PASA. The metatarsal head is then transposed laterally. Thus, the correction occurs in the transverse and sagittal planes as well as addressing the PASA. A 4.0-mm cancellous screw is used for fixation. K-wire fixation has been reported as successful in the same form of osteotomy (22). Good results have been reported in each study.
Then a second V osteotomy is performed on the proximal segment removing a medially based wedge to reduce the PASA. The metatarsal head is then transposed laterally. Thus, the correction occurs in the transverse and sagittal planes as well as addressing the PASA. A 4.0-mm cancellous screw is used for fixation. K-wire fixation has been reported as successful in the same form of osteotomy (22). Good results have been reported in each study.
Fixation of the Austin Procedure
Various fixation techniques have been recommended for the Austin bunionectomy. They are as varied as the modifications to the procedure, and each new modification is often described with recommendations for new fixation techniques.
When it was first described, the Austin osteotomy was stabilized by simple impaction of the capital fragment onto the proximal metatarsal shaft. Numerous reports have noted good to excellent results in patients with nonfixated Austin bunionectomies. Feit et al. reviewed 100 procedures, with 90 of the cases requiring a fibular sesamoidectomy (23). Average IM reduction was measured at 5.27 degrees, and only a single case required reoperation from a postoperative fracture. However, external forces acting on the metatarsal head during the postoperative period can result in rotation of the metatarsal head, dorsal malposition, and displacement of the capital fragment altogether (Fig. 13). Since the late 1980s, the preference for most surgeons has slowly shifted to employing some form of fixation for the procedure. However, as noted by the successes seen in the early studies, good results may be achieved without fixation.
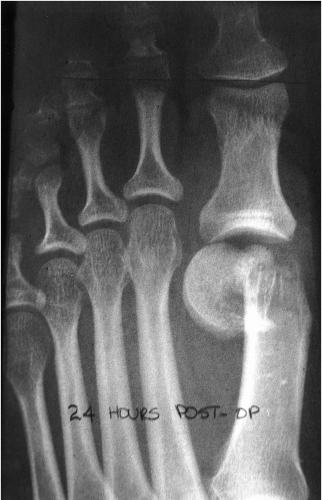 FIG. 13. Complete dislocation of the capital fragment of a nonfixated Austin osteotomy into the interspace 24 hours postoperatively. |
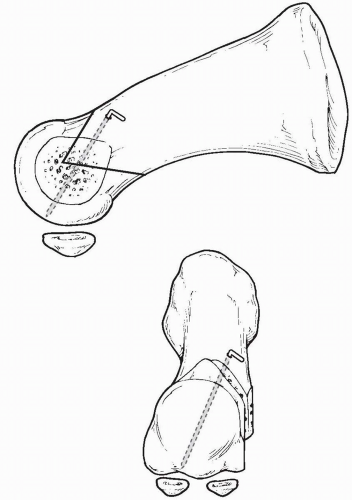
Many different forms of fixation have been advocated for the standard Austin procedure. K-wires are the simplest form of stabilization and have been used successfully for years. The most common technique is to direct the wire from dorsal proximal medial across the plantar arm of the osteotomy to enter the capital fragment plantar distal lateral. The wire may be left percutaneously or bent, cut, and turned to lie against the metatarsal shaft (Fig. 14). Care is taken to avoid protrusion of the K-wire into the joint space. A helpful technique is to visualize the wire within the joint and then to slowly move the wire in retrograde fashion until the tip lies just beneath the subchondral bone (24). Care should also be employed with percutaneous K-wires to avoid exiting along the dorsal margin of the joint, where it may restrict dorsiflexory mobilization.
Yu and Malay described an “intramedullary” locking K-wire technique in an effort to enhance the stability of K-wire fixation (25). The wire is introduced in a manner as described earlier. The wire is cut, leaving a small segment that is rotated from a medial to a dorsal position onto the top of the metatarsal shaft. If the angle of the bent wire is sufficiently acute, then the wire will need to be forced onto the dorsal cortex with pliers. Doing so results in a bending moment that is transferred to the portion of the K-wire inside
the metatarsal head. The key to locking the internal portion of the wire within the osteotomy successfully is to create a bend in the K-wire that is slightly more acute than the angle created by the exiting K-wire and the dorsal cortex of the metatarsal. This bending moment is analogous to intramedullary locking techniques for fixation of long bone fractures. When this is locked properly, it is extremely difficult to pull the K-wire free until it is rotated back medially and is “unlocked” from this position (Fig. 15).
the metatarsal head. The key to locking the internal portion of the wire within the osteotomy successfully is to create a bend in the K-wire that is slightly more acute than the angle created by the exiting K-wire and the dorsal cortex of the metatarsal. This bending moment is analogous to intramedullary locking techniques for fixation of long bone fractures. When this is locked properly, it is extremely difficult to pull the K-wire free until it is rotated back medially and is “unlocked” from this position (Fig. 15).
Some surgeons have employed threaded K-wires directed in a similar manner as the smooth counterpart. The threaded wire may then be cut flush with the bone. Several authors have described staple fixation for the osteotomy (26), one dorsally (27) and another medially (28). Absorbable pins and rods have also been employed with success (29,30). Allofix (Musculoskeletal Transplant Foundation, Edison, NJ) cortical bone allograft pins have been introduced and appear to provide good stability in the early follow-up period.
Screw fixation can also be used across the plantar arm of the Austin bunionectomy. Partially threaded screws are often considered in this technique. Because of standard screw design, it may be difficult to ensure that all the threads of a particular screw cross the osteotomy site. When possible, it is helpful to select a screw with a short thread pattern like the AO cannulated screws. The short thread pattern is one-third the length of the screw, in contrast to the standard half-length (Fig. 16). To assist in allowing more threads of the screw to cross the osteotomy site, it may be helpful to shift the apex of the osteotomy slightly more dorsally. In this fashion, the plantar arm exits further proximally along the plantar shaft of the metatarsal and provides a larger area of metatarsal head in which the screw can purchase. When a drill is used to prepare the direction of screw placement, it is helpful to drill into the joint space plantarly. After the measurement is taken, a screw length 2 to 3 mm shorter is selected to avoid intraarticular encroachment of the screw (Fig. 17). Any partially threaded screw can be used in this fashion, including the Herbert bone screw (31, 32, 33). Fully
threaded screws can also be used with proper preparation of the screw hole to achieve interfragmentary compression.
threaded screws can also be used with proper preparation of the screw hole to achieve interfragmentary compression.
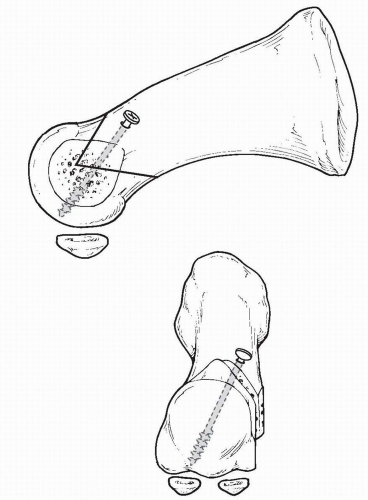 FIG. 16. Diagram of a partially threaded screw across the plantar arm of the osteotomy. This is similar to the direction of the Kirschner wire discussed earlier. |
Several authors have recommended adjusting the angle of the osteotomy to create a longer dorsal arm for screw fixation. The theory is that this approach allows the surgeon to translocate the capital fragment more aggressively. Fixation is often achieved with one or two screws or threaded K-wires. Specifically, this has involved one 2.7-mm cortical screw (34, 35, 36), two 2.7-mm cortical screws (13,37), or one 2.7-mm screw distally with a 2.0-mm screw proximally (2,3). It is ideal to place the fixation from the central portion of the dorsal fragment to the central portion of the plantar fragment. With this in mind, the fixation is oriented from dorsal lateral to proximal medial. The surgeon must make sure that the plantar exit point of the most distal is proximal to the plantar arm of the osteotomy. This approach secures stable cortical fixation to the osteotomy site. It is possible to aim too far laterally and for the screw to miss the plantar segment of the metatarsal altogether. If the angle of the screw is too oblique, the screw may fail to exit the plantar cortex and may slide along the plantar aspect of the medullary canal. In this instance, the screw may tighten, but less than optimal stabilization is achieved (Fig. 18).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree